The outbreak of the SARS-CoV-2 coronavirus pandemic, the lockdown decreed on 14th March 20201 and the need to restructure resources has had a strong impact on the different medical specialties.2
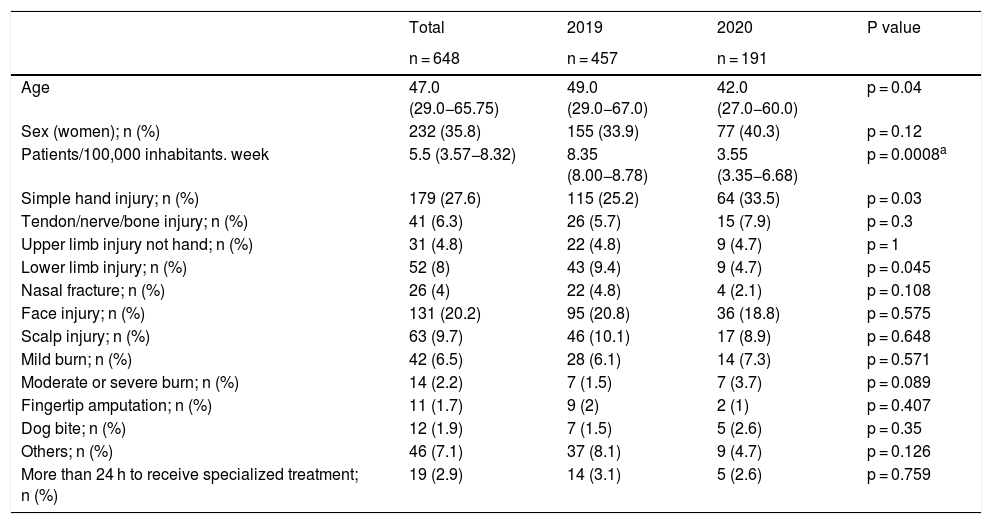
With the aim of knowing the impact of lockdown during the COVID-19 epidemic in plastic surgery emergencies, we have designed a cross-sectional descriptive observational study. The data were collected by 3 plastic surgery department surgeons from the Diraya database for patients treated for plastic surgery in the emergency department (tertiary referral hospital for 921,000 people) from 16th March to 26th April 2020 (6 weeks of lockdown) so as to compare them with the patients seen on the same dates in 2019. The period from 18 March to 28 April 2019 was considered for comparison of calendar weeks. Pediatric patients were excluded. The variables age, sex, reason for consultation (Table 1), requirement of specialized procedure (admission/intervention) and time to receive it (< 24 ho> 24 h) were collected. Regarding reasons for consultation: less than 5 patients were classified as «other».
Statistical results.
| Total | 2019 | 2020 | P value | |
|---|---|---|---|---|
| n = 648 | n = 457 | n = 191 | ||
| Age | 47.0 (29.0−65.75) | 49.0 (29.0−67.0) | 42.0 (27.0−60.0) | p = 0.04 |
| Sex (women); n (%) | 232 (35.8) | 155 (33.9) | 77 (40.3) | p = 0.12 |
| Patients/100,000 inhabitants. week | 5.5 (3.57−8.32) | 8.35 (8.00−8.78) | 3.55 (3.35−6.68) | p = 0.0008a |
| Simple hand injury; n (%) | 179 (27.6) | 115 (25.2) | 64 (33.5) | p = 0.03 |
| Tendon/nerve/bone injury; n (%) | 41 (6.3) | 26 (5.7) | 15 (7.9) | p = 0.3 |
| Upper limb injury not hand; n (%) | 31 (4.8) | 22 (4.8) | 9 (4.7) | p = 1 |
| Lower limb injury; n (%) | 52 (8) | 43 (9.4) | 9 (4.7) | p = 0.045 |
| Nasal fracture; n (%) | 26 (4) | 22 (4.8) | 4 (2.1) | p = 0.108 |
| Face injury; n (%) | 131 (20.2) | 95 (20.8) | 36 (18.8) | p = 0.575 |
| Scalp injury; n (%) | 63 (9.7) | 46 (10.1) | 17 (8.9) | p = 0.648 |
| Mild burn; n (%) | 42 (6.5) | 28 (6.1) | 14 (7.3) | p = 0.571 |
| Moderate or severe burn; n (%) | 14 (2.2) | 7 (1.5) | 7 (3.7) | p = 0.089 |
| Fingertip amputation; n (%) | 11 (1.7) | 9 (2) | 2 (1) | p = 0.407 |
| Dog bite; n (%) | 12 (1.9) | 7 (1.5) | 5 (2.6) | p = 0.35 |
| Others; n (%) | 46 (7.1) | 37 (8.1) | 9 (4.7) | p = 0.126 |
| More than 24 h to receive specialized treatment; n (%) | 19 (2.9) | 14 (3.1) | 5 (2.6) | p = 0.759 |
The quantitative variables were expressed as median (25th–75th percentile) and the qualitative variables by absolute number and percentage. The Mann–Whitney U test has been used to compare quantitative variables and the Chi-square for qualitative variables. To analyse frequency, the daily data in 6 weeks of 2019 and their corresponding in 2020 have been grouped and a generalized Poisson model has been used to compare the weekly incidence between periods. To facilitate interpretation, we have transformed the coefficients in terms of risk together with their confidence intervals. The statistical program «R» with the application «Rcmdr» was used for the statistical analysis. A p value = 0.05 was considered statistically significant.
Six hundred and forty-eight patients were included in the study (35.8% female, 47.0 [29.0−65.75] years of age). Four hundred and fifty-seven were treated in the period of 2019 and 191 in that of 2020. The patients seen in 2020 were younger (42.0 [27.0−60.0] years; p = 0.04). There were no differences related to sex (Table 1). The relative frequency of upper and lower limb injuries varied during lockdown (Table 1). No significant differences were obtained in "requirement for admission/surgical intervention" (16 vs. 17.3%) or in delay times (Table 1). The number of patients treated during lockdown was 3.55 (3.35–6.6) patients/week per 100,000 inhabitants per 8.35 (8.00−8.78) in the period of 2019 (p = 0.008) with relative risk (RR) = 0.42 (0.25−0.68).
One of the possible explanations for the significant decrease in the number of patients seen per week is a reduction in the causal mechanisms due to restricted mobility. Another possible explanation is fear of infection. However, we found no differences in the proportion of patients requiring admission/surgery, which suggests that there has not been an increase in the severity threshold for emergency department visits as evidenced in other specialties.3 In reference to the age of the patients there is a statistically significant decrease during the pandemic, and it cannot be ruled out that older patients have sought less medical attention for fear of infection.
During lockdown, the percentage of hand injuries increased in relative terms and the percentage of lower limb injuries and nasal fractures decreased. The findings could be justified by increased exposure to domestic accidents4 and a decrease in traffic and sports accidents.5
Not finding any differences in the percentage of patients who received specialised care or delays in such care, suggests that no delays in specialised care derived from the protocols developed for the pandemic were identified in our centre.
As limitations of the study, it should be noted that the data were collected from an area with an average COVID seroprevalence, although much of it may be generalizable, others will vary with the prevalence of the infection.
In summary, the COVID-19 has had an impact on the number of emergencies handled by the plastic surgery department, decreasing to less than half. These data can be important for planning emergency care in possible future outbreaks, or in countries where the pandemic has not yet erupted.
Ethical responsibilitiesAll the authors have confirmed the preservation of confidentiality and respect for patients’ rights.
FundingThe authors declare the non-existence of funding in relation to the article.
Conflict of interestsThe authors declare the non-existence of conflicts of interest in relation to the article.
Please cite this article as: Cases-Perera O, Losilla-Rodríguez J, Rivera-Lopez R. Impacto del confinamiento por la COVID-19 en la actividad asistencial de cirugía plástica en el servicio de urgencias. Med Clin (Barc). 2021;156:139–140.