Cytokine storm syndrome (CSS) is a serious complication of COVID-19 patients. Treatment is tocilizumab. The use of glucocorticoids (GC) is controversial. In other very similar CSS, such as macrophage activation syndrome (MAS) and hemophagocytic syndrome (HFS), the main treatment are corticosteroids. Our objective is to evaluate the efficacy of GC in the CSS by COVID-19.
PatientsWe included 92 patients with CSS associated to COVID-19 who received GC, GC, and tocilizumab and only tocilizumab. We determine CSS markers. We evaluated mortality, intubation, and a combined variable.
ResultsIn all cases the percentages of events were lower in the group of patients with GC was administered. The hazard ratio of the final variables with GC versus the group in which only tocilizumab was administered was lower as CGs were considered, with statistical significance for survival.
DiscussionThe early use of GC pulses could control SLC, with a lower requirement to use tocilizumab and a decrease in events such as intubation and death.
El síndrome de liberación de citocinas (SLC) es una complicación grave de los pacientes COVID-19. La base del tratamiento es tocilizumab. El uso de glucocorticoides (GC) es controvertido. En otros SLC muy parecidos, como son el síndrome de activación macrofágica (SAM) y el síndrome hemofagocítico (SHF) el tratamiento con los corticoides es fundamental. Nuestro objetivo es evaluar la eficacia de los GC en el SLC por COVID-19.
PacientesIncluimos 92 pacientes con SLC por COVID-19 que recibieron GC, GC y tocilizumab y sólo tocilizumab. Determinamos marcadores de SLC. Evaluamos mortalidad, intubación y una variable combinada.
ResultadosEn todos los casos los porcentajes de eventos fueron menores en el grupo de pacientes en los que se administraron GC. Las razones de riesgo de las variables finales de los grupos con GC frente al grupo en el que se administró sólo tocilizumab fue menor conforme se consideraron los GC, con significación estadística para la supervivencia.
DiscusiónEl uso precoz de pulsos de GC puede controlar el SLC, con un menor requerimiento de uso de tocilizumab y una disminución de eventos como la intubación y muerte.
Cytokine release syndrome (CRS) is a serious complication of SARS-CoV-2 disease (COVID-19).1,2 The basis of its treatment is essentially tocilizumab, an anti-IL-6 agent.3 The use of glucocorticoids (GC) is controversial.4–6 However, in the hyperinflammation phase, they could be very beneficial, as in other diseases in which there is a cytokine storm similar to the one that occurs in COVID-19, like macrophage activation syndrome (MAS) or hemophagocytic syndrome (HPS).7,8
The objective of this study is to evaluate the efficacy of the administration of GC pulses in patients who have an CRS due to COVID-19.
Patients and methodsRetrospective observational study in the internal and intensive medicine departments. Patients admitted for SARS-CoV-2 infection confirmed by PCR and who met CRS criteria defined by elevation of IL-6 > 40 pg/ml and/or 2 of the following: ferritin > 300 µg/l, d-dimers > 1 mg/l and/or triglycerides > 300 mg/dl were included. We classified patients into 3 groups: (1) those who received only GC pulses; (2) GC pulses and tocilizumab simultaneously, and (3) exclusively tocilizumab. Pulses were classified into 2 mg/kg/day for 3 days, 250 mg/day for 3 days and 500 mg/day for 3 days. Serum levels of ferritin, CRP and d-dimers before administration and during follow-up, with intervals of 24–72 h following routine practice. Survival, the need for intubation and a combined variable of the latter 2 were established as endpoints. All patients gave their consent for treatment.
The main variables of the study were described according to the frequency distribution and the basic measurements of numerical summary, mean, standard deviation and range. The analysis of the time until each of the response variables occurred was made by calculating the survival curves using the Kaplan–Meier method and the estimates of the risk ratios were made using the Cox proportional hazards model. Comparisons between treatments and within treatments between intervals were analysed using a mixed linear model with pairwise comparisons when it was significant. Stata v.14.1 software was used.
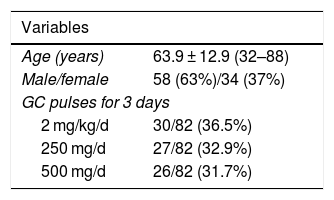
ResultsA total of 92 patients were included. The baseline characteristics are shown in Table 1.
Of the 92 patients, 60 (65.2%) received GC pulses alone, 23 (25%) pulses combined with tocilizumab and 9 (9.8%) tocilizumab alone. There were 7 (7.6%) deaths and 5 (5.6%) intubations; one of the patients requiring intubation died. The combined intubation/death variable occurred in 11 (12.4%) cases. The median follow-up of the patients was 11 days.
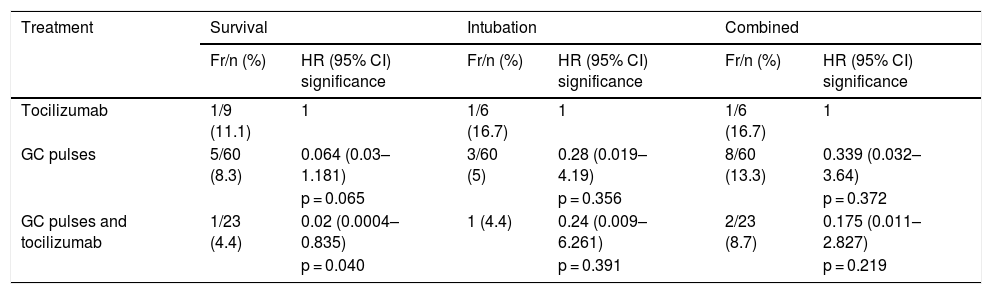
Table 2 shows the percentages, per treatment, of presentation of each of the endpoints considered, as well as the risk ratio of the treatments compared to the treatment in which CG is not included. In all cases, the percentages of events were lower in the group of patients in whom GC was administered, with the combined treatment group being the one with the lowest percentage of events.
Frequencies of the 3 outcome measures according to treatments and HR for the Cox regression models of time up to the event.
| Treatment | Survival | Intubation | Combined | |||
|---|---|---|---|---|---|---|
| Fr/n (%) | HR (95% CI) significance | Fr/n (%) | HR (95% CI) significance | Fr/n (%) | HR (95% CI) significance | |
| Tocilizumab | 1/9 (11.1) | 1 | 1/6 (16.7) | 1 | 1/6 (16.7) | 1 |
| GC pulses | 5/60 (8.3) | 0.064 (0.03–1.181) | 3/60 (5) | 0.28 (0.019–4.19) | 8/60 (13.3) | 0.339 (0.032–3.64) |
| p = 0.065 | p = 0.356 | p = 0.372 | ||||
| GC pulses and tocilizumab | 1/23 (4.4) | 0.02 (0.0004–0.835) | 1 (4.4) | 0.24 (0.009–6.261) | 2/23 (8.7) | 0.175 (0.011–2.827) |
| p = 0.040 | p = 0.391 | p = 0.219 | ||||
Fr/n: frequencies by outcome; GC: glucocorticoids; HR: hazard ratio (risk ratio) estimated using the Cox proportional hazards model; CI: confidence interval.
Regarding the risk ratios of the different outcome variables of the groups with GC versus the group in which only tocilizumab was administered, it was observed that the risk of each of the events was lower as treatment with GC was considered, reaching statistical significance in the case of survival and a trend, although without reaching significance, both for intubation and for the combined variable.
In the Kaplan–Meier survival curves, there was a trend towards less need for intubation, death, and the combined variable. It was clear that there was no increase in deaths in the group of patients receiving GC.
The evolution of biochemical markers was highly variable. The initial mean ferritin levels were 1238 µg/l in the GC and tocilizumab group, 832 µg/l in GC and 1024 µg/l in that of tocilizumab, without observing a significant decrease in any of the groups at the end of the follow-up. A significant decrease in CRP was observed already in the first determination after treatment, which was maintained until the end of the follow-up in the 3 groups. d-dimers remained high without significant decreases.
DiscussionThe results of this study show that, in patients with COVID-19-induced CRS, the combination of GC pulses seems to be associated with a better prognosis of the disease, with a clear tendency towards lower mortality and lower need for intubation.
The role of GCs in COVID-19 patients is not well established. In the review carried out by Russell et al.4 on lung injury induced by different viruses including SARS and MERS and in the study by Wang et al.5 no beneficial effect was observed; they were even associated to a probable increase in mortality. Therefore, the use of GC has not been recommended. Recently, Wu et al.6 demonstrated a decreased risk of mortality in patients with respiratory distress who received methylprednisolone.
The objective of our work has been to evaluate the efficacy of GC in another serious complication of SARS-CoV-2 such as CRS. Increased levels of CRP and ferritin are 2 characteristic and key data for its diagnosis. Unlike HPS, which has a diagnostic criteria7 and a scoring system that helps to estimate the probability of suffering from it, called HScore,9 there are no well-established criteria for the definition of CRS. The presence of elevated IL-6 and/or the combination of 2 or more laboratory anomalies, mainly increased levels of ferritin suggests the presence of CRS. All the included patients met the criteria, with remarkably high ferritin levels. Treatment of HPS, often associated with infectious processes,7 and others with different systemic autoimmune diseases, in this case called MAS,8 is based on 2 pillars: on the one hand, the etiological treatment, if any, and on the other, the treatment of the cytokine storm.10 In all cases, high-dose and mainly pulsed GCs are the basis of treatment. In the case of SARS-CoV-2-induced CRS, the recommended treatment has been tocilizumab,2,3 an expensive drug and difficult to access for all patients. The fact that GCs have been effective in a large number of patients may allow it to be administered as a second option for non-respondents.
In our study we decided to assess the response to treatment by means of 2 high impact clinical variables such as the need for intubation and mortality; therefore, we only included deceased patients who had received some of the treatment arms, and excluded those who were admitted due to requiring intubation. We observed that in the patients who received GC pulses, either alone or in combination with tocilizumab, there was a tendency to decrease in the events of death, intubation, and the combination of both, being higher in cases of combination of both drugs. We did not find differences between the different doses used, therefore, probably the lowest dose of 2 mg/kg/day for 3 days is the most recommended dose.
The interest of our study is based on the administration of GC pulses, an effective treatment for other diseases similar to SARS-CoV-2-induced CRS, more economical and accessible to other experimental treatments used in this disease such as tocilizumab, and which for different reasons it has been discouraged, demonstrating its objective clinical benefit. The limitations of the study are its retrospective nature, the sample size, the reduced number of clinical events and the short follow-up period, so the results must be confirmed with a clinical trial with a larger sample size and a longer follow-up.
We conclude that early identification of CRS is essential in patients with COVID-19 and that, in case of onset, the early use of GC pulses can control it, probably with a lower requirement to use tocilizumab and with a decrease in events such as intubation and death.
Conflict of interestsThe authors declare no conflict of interest.
Please cite this article as: Callejas Rubio JL, Luna del Castillo JD, de la Hera Fernández J, Guirao Arrabal E, Colmenero Ruiz M, Ortego Centeno N. Eficacia de los pulsos de corticoides en pacientes con síndrome de liberación de citocinas inducido por infección por SARS-CoV-2. Med Clin (Barc). 2020;155:159–161.