SARS-CoV-2 infection results in a constellation of symptoms that generally tend to resolve within a few weeks; however, in up to 20% of cases, symptoms persist for several weeks or months after microbiological evidence of active infection is negative. This state embodies the concept of long COVID-19 disease. Symptoms of neurological interest include cognitive impairment -mental fog- and exhausting fatigue.1 Currently, there is no effective treatment for these symptoms and their persistence diminishes the quality of life of patients.
Mitochondrial energy dysfunction has been shown in chronic fatigue syndrome (CFS) and fibromyalgia, and this same pathophysiological basis has been involved in the fatigue of long COVID-19 disease. Based on this working hypothesis and given the beneficial effect that hyperbaric oxygen therapy (HBOT) has demonstrated metabolically, improving mitochondrial function and reducing oxidative stress,2 our research group has proposed a study, based on HBOT, to assess the efficacy on cognitive symptoms and chronic fatigue in patients with long COVID-19.
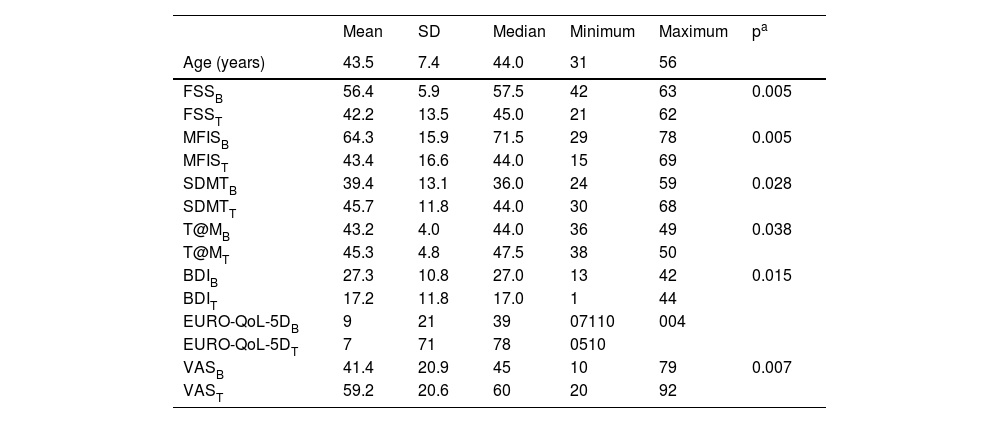
Ten patients (7 F:3 M) with a diagnosis of long COVID-19, whose infection was confirmed by PCR and who had a course of fatigue symptoms and cognitive complaints (impaired memory/attentional deficit) exceeding 12 weeks, were studied. Patients received 40 treatment sessions with HBOT at a pressure of 2.6–2.8 ATA. Patients were assessed with cognitive, fatigue and quality of life scores before entry into the hyperbaric chamber and one month after the last HBOT session. Table 1 summarises the baseline and post-treatment measures of dispersion of the variables analysed with hyperbaric oxygen. Patients improved significantly in the main study variables, fatigue and cognitive impairment, and, in addition, depressive symptoms and quality of life also improved with HBOT.
Measures of dispersion of the variables analysed in the study.
| Mean | SD | Median | Minimum | Maximum | pa | |
|---|---|---|---|---|---|---|
| Age (years) | 43.5 | 7.4 | 44.0 | 31 | 56 | |
| FSSB | 56.4 | 5.9 | 57.5 | 42 | 63 | 0.005 |
| FSST | 42.2 | 13.5 | 45.0 | 21 | 62 | |
| MFISB | 64.3 | 15.9 | 71.5 | 29 | 78 | 0.005 |
| MFIST | 43.4 | 16.6 | 44.0 | 15 | 69 | |
| SDMTB | 39.4 | 13.1 | 36.0 | 24 | 59 | 0.028 |
| SDMTT | 45.7 | 11.8 | 44.0 | 30 | 68 | |
| T@MB | 43.2 | 4.0 | 44.0 | 36 | 49 | 0.038 |
| T@MT | 45.3 | 4.8 | 47.5 | 38 | 50 | |
| BDIB | 27.3 | 10.8 | 27.0 | 13 | 42 | 0.015 |
| BDIT | 17.2 | 11.8 | 17.0 | 1 | 44 | |
| EURO-QoL-5DB | 9 | 21 | 39 | 07110 | 004 | |
| EURO-QoL-5DT | 7 | 71 | 78 | 0510 | ||
| VASB | 41.4 | 20.9 | 45 | 10 | 79 | 0.007 |
| VAST | 59.2 | 20.6 | 60 | 20 | 92 |
B, baseline; BDI, Beck Depression Inventory; EURO-Qol-5D, quality of life scale; FSS, fatigue severity scale; MFIS, modified fatigue scale; SDMT, symbol digit modalities test; T, post-treatment; T@M,memory impairment test; VAS, visual analogue scale of health status.
Concurrently with our study, results have been published on patients with long COVID-19 who have shown improvement in fatigue, cognitive impairment and depressive symptoms with HBOT.3 A clinical study with functional neuroimaging and diffusion tensor imaging provides evidence that the observed cognitive and psychological improvements in patients with long COVID are due to the ability of HTO to induce brain neuroplasticity.4
CFS has a classic definition and is characterised by disabling fatigue lasting at least 6 months, which the patient experiences as exhausting, and which is accompanied by concentration and short-term memory problems. A hallmark feature of CFS is post-exertional malaise, which is a physical or mental worsening with exercise, occurring 12–48 h after exercise, and requiring a prolonged recovery period. Although the aetiology of CFS is considered unknown, it is well known that symptoms may start after a viral infection, usually herpesvirus, and this could be the case for the persistence of symptoms after coronavirus infection. Within the pathophysiology of CFS, a dysregulation of the immune system has been postulated, resulting in a prevalence of inflammatory biomarkers in serum; in addition, metabolic dysfunction has been found, so that CFS is associated on the one hand with a hypometabolic state and, on the other hand, mitochondrial energy generation disorders have been observed.5
Our study has shown that HBOT contributes to a decrease in fatigue in patients with long COVID-19, which could be explained by an energy-metabolic and mitochondrial function improvement due to increased tissue oxygenation. The cognitive improvement in information processing speed, which is assessed by SDMT, would be supported by the increase in blood hyperoxygenation with an increase in cerebral blood flow, a decrease in the presence of oxygen free radicals and various biomarkers of inflammation, and brain neuroplasticity induced by HBOT.2,4
Ethical and legal responsibilitiesThis study has been approved by the Health Care Ethics Committee and the Medical Direction of the COSAGA clinic in Ourense. Patients gave written informed consent for treatment with hyperbaric oxygen therapy and for access to clinical data.
Conflict of interestNone.
FundingThe study was fully funded by the COSAGA clinic in Ourense.