Diffuse idiopathic skeletal hyperostosis (DISH) and abdominal aortic calcification (AAC) are related to an increased cardiovascular risk. The aim of this study was to analyze a possible relationship between both entities and also the association between metabolic disorders and DISH.
Patients and methodAnalytic cross-sectional study in a population-based cohort. DISH (with Resnick-Niwayama criteria) and AAC (with AAC-24 scale) were assessed on plain X-ray images. Interaction terms between DISH and forty clinical covariates were also investigated, through correlation analysis and multivariate regression.
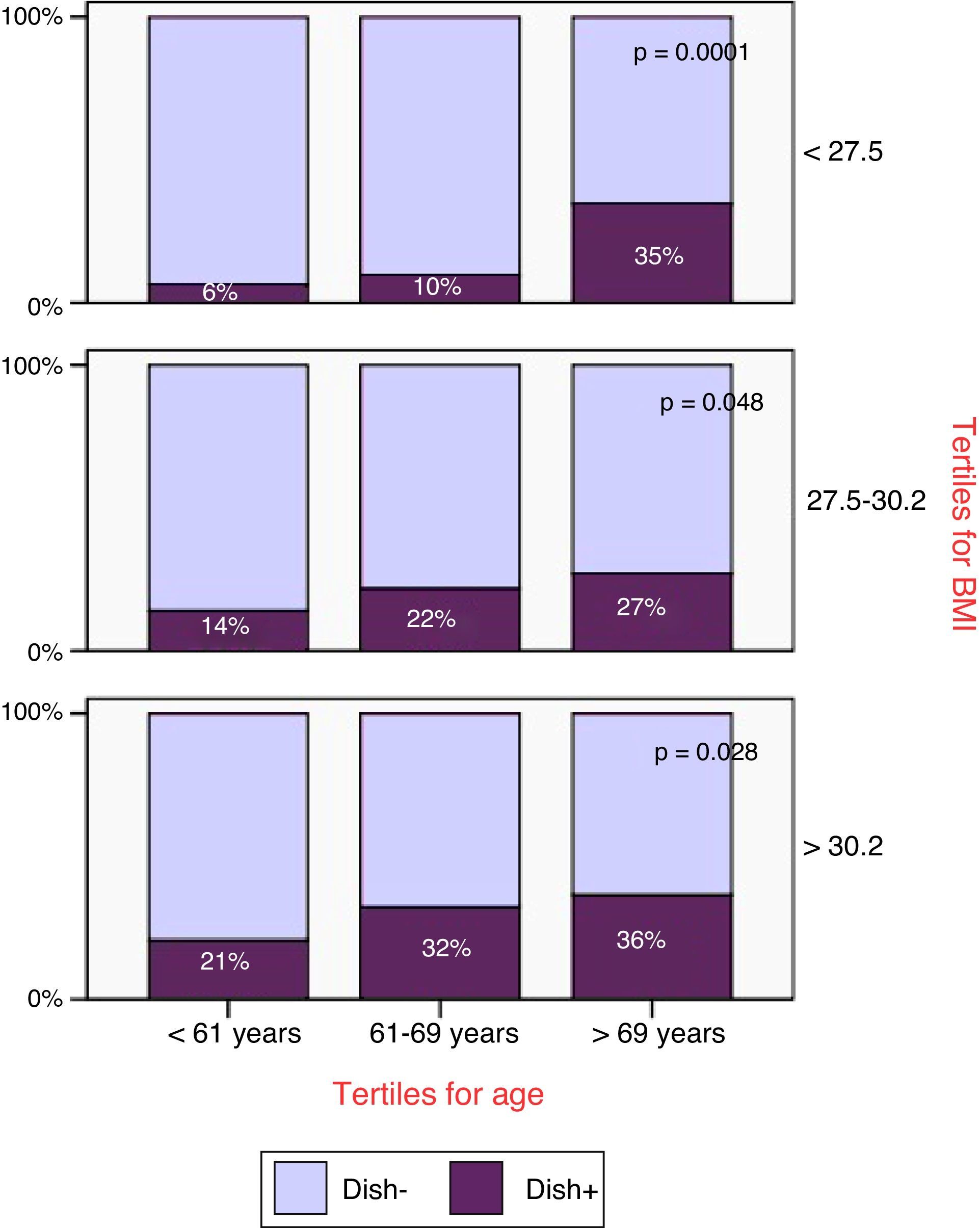
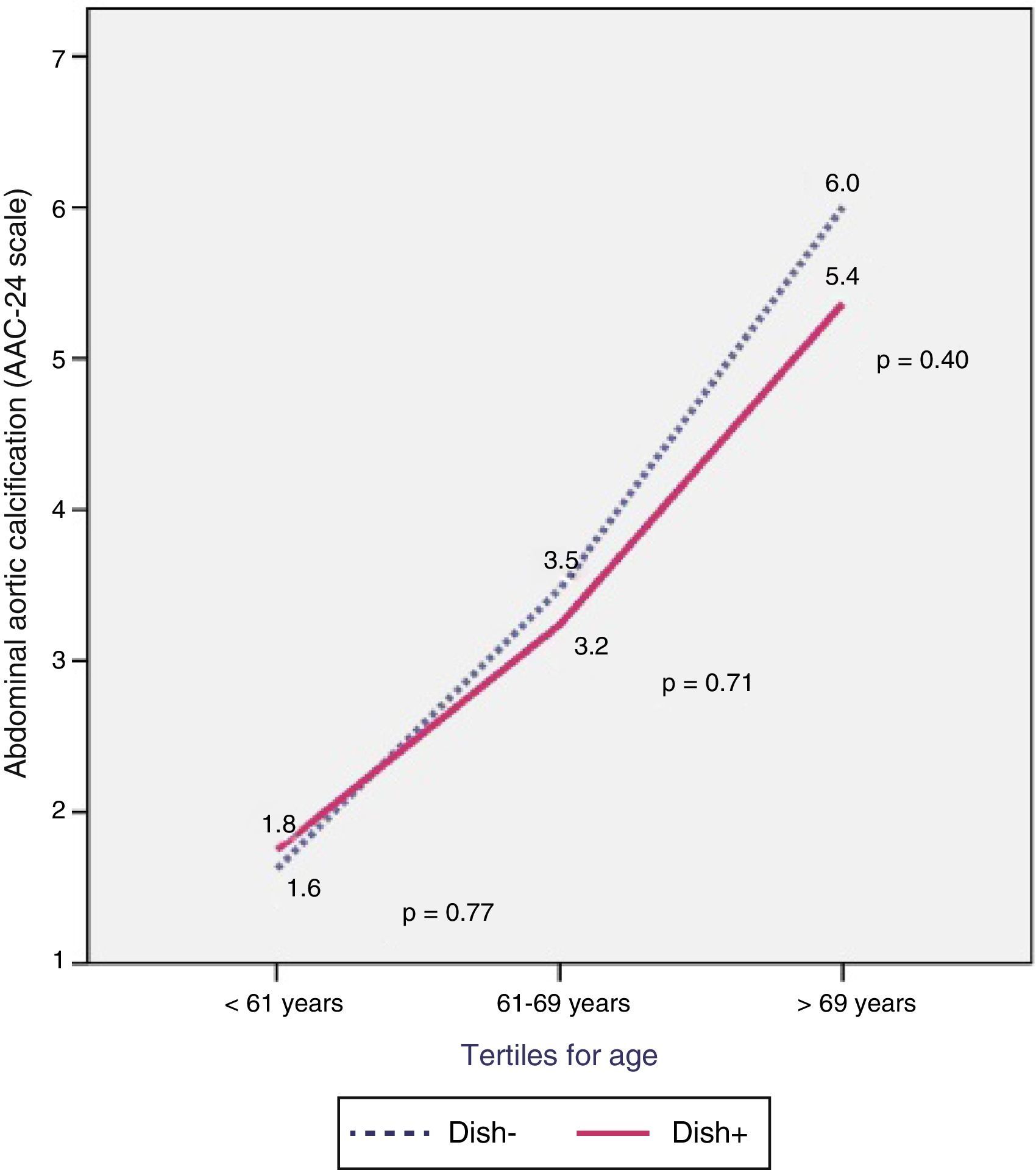
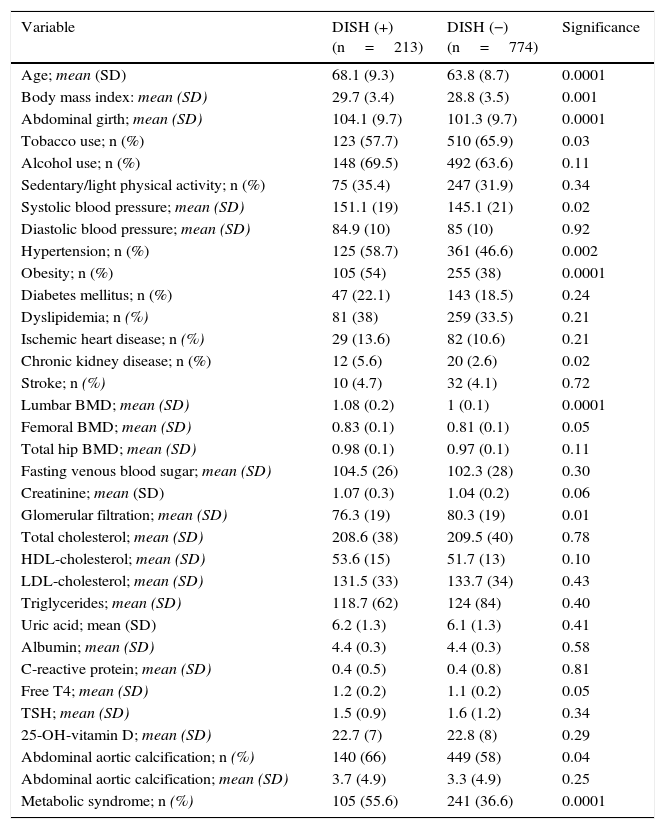
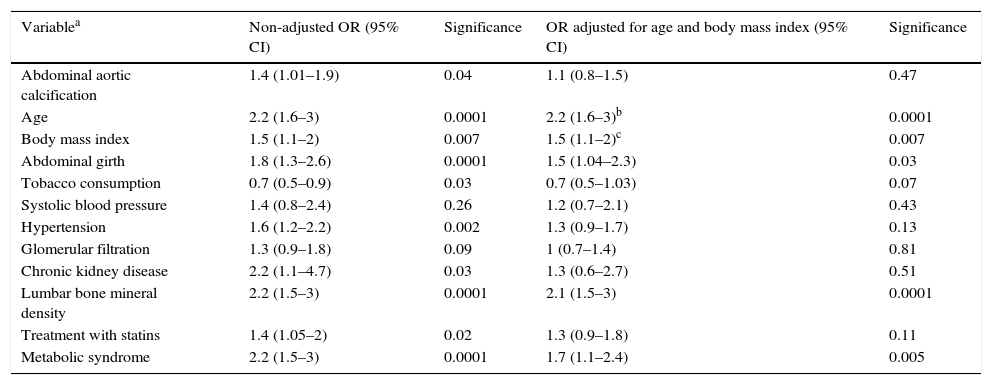
ResultsNine hundred eighty-seven males aged ≥50 years, with a mean age=65.5±9 years, were evaluated. Prevalence rates of DISH and AAC were 21.6% and 58.7%, respectively. DISH+ subjects were older (68.1±9 vs. 63.8±9 years; p=0.0001) and more likely to be affected by metabolic syndrome (MS) (55.6% vs. 36.6%; p=0.0001). In DISH+ subjects, the AAC was 3.7±5 points, whereas in DISH− subjects it was 3.3±5 (p=0.25). AAC was associated with an increased risk of prevalent DISH (unadjusted OR=1.4 [95% CI: 1.01–1.9]; p=0.04), that disappeared when it was adjusted for age (adjusted OR=1.1 [95% CI: 0.8–1.5]; p=0.47). No association was found between DISH and hypertension, diabetes or dyslipidemia; however, age (OR=2.2 [95% CI: 1.6–3]; p=0.0001), BMI (OR=1.5 [95% CI: 1.1–2]; p=0.007), waist circumference (OR=1.5 [95% CI: 1.04–2.3]; p=0.03) and MS (OR=1.7 [95% CI: 1.1–2.4]; p=0.005) showed a significant relationship with DISH after adjusting for confounders.
ConclusionsThe study was not able to demonstrate a consistent association between DISH and AAC, proving only a weak and age-dependent relationship between them. DISH proved to be significantly associated with age, BMI, waist circumference and MS.
La hiperostosis esquelética idiopática difusa (DISH, del inglés diffuse idiopathic skeletal hyperostosis) y la calcificación aórtica abdominal (CAA) se asocian a un incremento del riesgo cardiovascular. El objetivo fue analizar una posible relación entre ambas, así como las alteraciones metabólicas asociadas a la DISH.
Pacientes y métodoEstudio transversal-analítico, incluido en una cohorte poblacional. La DISH (criterios de Resnick-Niwayama) y la CAA (mediante la escala AAC-24) fueron evaluadas sobre imágenes de radiología simple. Se evaluaron asimismo otras 40 variables clínicas mediante correlaciones y regresión multivariante.
ResultadosFueron analizados 987 varones≥50 años, con una edad media=65,5±9 años. Las prevalencias de DISH y CAA fueron del 21,6% y del 58,7%, respectivamente. El sujeto con DISH tenía mayor edad (68,1±9 vs. 63,8±9 años; p=0,0001) y con mayor frecuencia presentaba síndrome metabólico (SM) (55,6 vs. 36,6%; p=0,0001). La CAA fue de 3,7±5 puntos en sujetos con DISH frente a 3,3±5 en sujetos sin DISH (p=0,25), y se asoció a un riesgo incrementado de DISH prevalente (OR cruda=1,4 [IC95%: 1,01-1,9]; p=0,04), que desapareció al ajustar por edad (OR ajustada=1,1 [IC95%: 0,8-1,5]; p=0,47). No se observó asociación de la DISH con la hipertensión arterial, diabetes mellitus o dislipidemia, pero mantuvieron una relación significativa tras ajustar por confusores la edad (OR=2,2 [IC95%: 1,6-3]; p=0,0001), el IMC (OR=1,5 [IC95%: 1,1-2]; p=0,007), el perímetro abdominal (OR=1,5 [IC95%: 1,04-2,3]; p=0,03) y el SM (OR=1,7 [IC95%: 1,1-2,4]; p=0,005).
ConclusionesNo se ha podido demostrar una asociación consistente entre la DISH y la CAA, presentando ambas una débil relación dependiente de la edad. La DISH ha mostrado unas asociaciones significativas con la edad, el IMC, el perímetro abdominal y el SM.
Artículo
Comprando el artículo el PDF del mismo podrá ser descargado
Precio 19,34 €
Comprar ahora