During the beginning of 2020 we have witnessed a pandemic caused by the SARS-CoV-2 virus, which has confronted us with numerous questions, particularly in patients with special clinical characteristics, such as those suffering from multiple sclerosis (MS), many of whom are being treated with immunomodulatory or immunosuppressants that compromise their immune system, which could imply a higher risk of becoming ill or of developing a worse clinical course. To verify this hypothesis, a descriptive study has been designed by reviewing the medical records of all patients diagnosed with MS in the autonomous community of La Rioja, collecting clinical and epidemiological data.
At the time of the study, La Rioja has 316,798 inhabitants, 330 diagnosed with MS (1.04/1000 inhabitants), of which 12 have suffered from SARS-CoV-2 infection, (3.6%), nine diagnosed by PCR and three by serology. The typical patient is female (75%), 47.91 years (22–74), 75% with a relapsing remitting form and 25% secondary progressive. The mean value of the Expanded Disability Status Scale (EDSS) was 1.92 (0–8). 25% were not treated, two (16.66%) were treated with each of the following therapies: subcutaneous interferon beta-1a, dimethyl fumarate and teriflunomide, and one (8.33%) with fingolimod, cladribine and alemtuzumab.
A case was considered when the criteria of the Carlos III Health Institute for the general population were met, so as to be able to establish comparisons (presence of symptoms and confirmation by PCR). The criteria were met by nine patients. As of 27th May 2020, 31 PCRs had been carried out for SARS-CoV-2, which represents 93.94/1000 inhabitants, similar to the 99.81/1000 inhabitants in La Rioja. 29.03% (9/31) were positive compared to 12.79% of the general population.1 The incidence of COVID-19 cases among the population with MS was 27.27/1000 inhabitants, compared to 12.76/1000 inhabitants in La Rioja (OR 2.17; 95% CI 1.12–4.21).
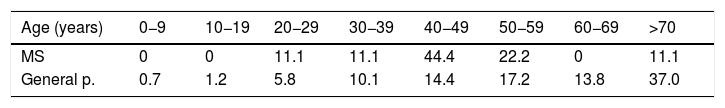
The age distribution of the cases is presented in Table 1, highlighting 66.7% among patients with MS between 40–59 years of age, and scarce among those over 60, which represents 50% of the general population.1
Distribution of MS patients diagnosed with COVID-19 and general population.3
| Age (years) | 0−9 | 10−19 | 20−29 | 30−39 | 40−49 | 50−59 | 60−69 | >70 |
|---|---|---|---|---|---|---|---|---|
| MS | 0 | 0 | 11.1 | 11.1 | 44.4 | 22.2 | 0 | 11.1 |
| General p. | 0.7 | 1.2 | 5.8 | 10.1 | 14.4 | 17.2 | 13.8 | 37.0 |
Patients with MS and COVID-19 showed an average of 3.1 (1–6) symptoms, highlighting cough and fever (66.7%), pharyngeal pain (55.6%), myalgia (44.4%), asthenia ( 33.3%), headache (22.2%), dyspnoea and anosmia (11.1%). The cumulative hospitalization rate for patients with MS was 22.2% compared to 36.63% for the overall rate in La Rioja1 (OR 0.47 CI5% 0.09–2.29).
Only one patient in our series died, a 74-year-old male, secondary progressive MS, EDSS 7 and no treatment. The case fatality rate was 11.1% (vs. 8.91 in La Rioja, without statistical significance). As there is a much higher percentage of PCR positives among those affected by MS, the mortality rate showed a greater difference, 3.03/1000 inhabitants vs. 1.14 in La Rioja, but without reaching statistical significance (OR 2.67; 95% CI 0.37–19.07).
DiscussionIt is established that patients with MS have a higher risk of infections requiring hospitalization, pointing to a possible increase in viral infections, pneumonia and influenza.2 Our results show that patients with MS have experienced a COVID-19 incidence that is more than double that of the general population and this cannot be attributed to having undergone more PCR studies.
We are aware of a study that did not show an increased risk of COVID-19 among patients with MS in China, although it was conducted through questionnaires and personal communication from patients, and the authors themselves argue that this may have left out many patients with minor symptoms or who refused communication to avoid quarantine in designated facilities.3
Among the symptoms, the most common in our series were cough and fever, with a low incidence of anosmia, similar to what was published.4 The hospitalization rate in our series is slightly lower (without statistical significance) among MS patients in the context of a lower mean age.
Finally, in terms of mortality, the rate was 11.1% among our MS patients. This figure does not differ much from the general population. In a multicenter study carried out in Italy, 57 patients with positive PCR were detected, of which five died (8.77%), all with EDSS ≥ 6.55 and in another publication with a series of eight cases in the United States, two died, with EDSS of 7.5 and 8.5,4 in line with what was observed in our study.
In conclusion, the incidence of COVID-19 cases among patients with MS in our series is double that of the general population, despite not having performed a higher number of tests.
The hospitalization and fatality rate has been similar, affecting a 74-year-old patient with high EDSS, in line with the experience reported by other groups.
Given a similar fatality rate in a context of higher infection incidence, the mortality associated with COVID-19 infection among our MS patients tends to be higher than in the general population, but without reaching statistical significance.
FundingThis study has not received any type of funding.
Conflict of interestsThe authors declare no conflict of interest.
Please cite this article as: Castillo Álvarez F, López Pérez M, Marzo Sola ME. Riesgo de infección por SARS-CoV-2 y resultados clínicos en pacientes con esclerosis múltiple en la Rioja (España). Med Clin (Barc). 2020;155:362–363.