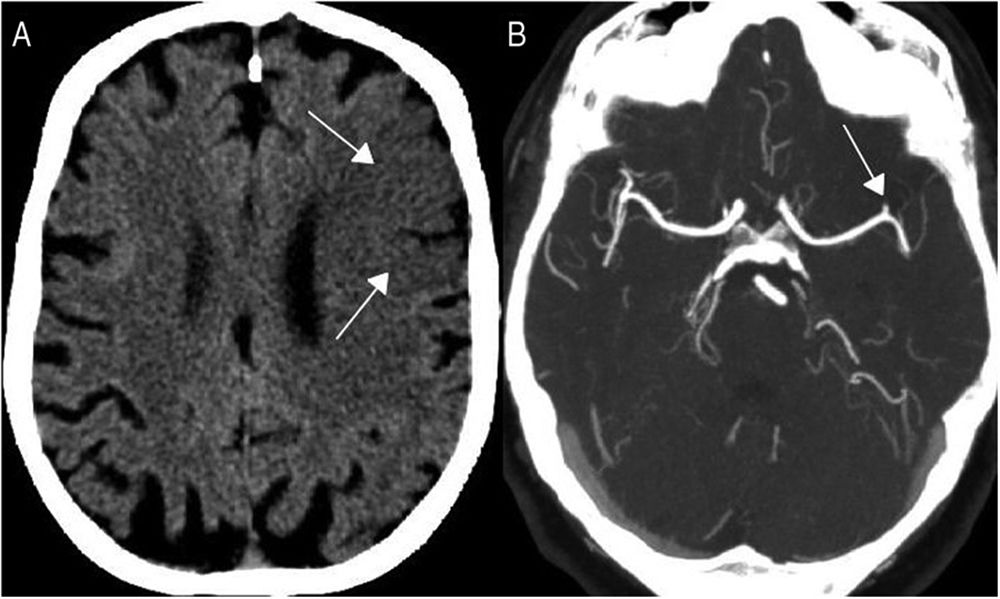
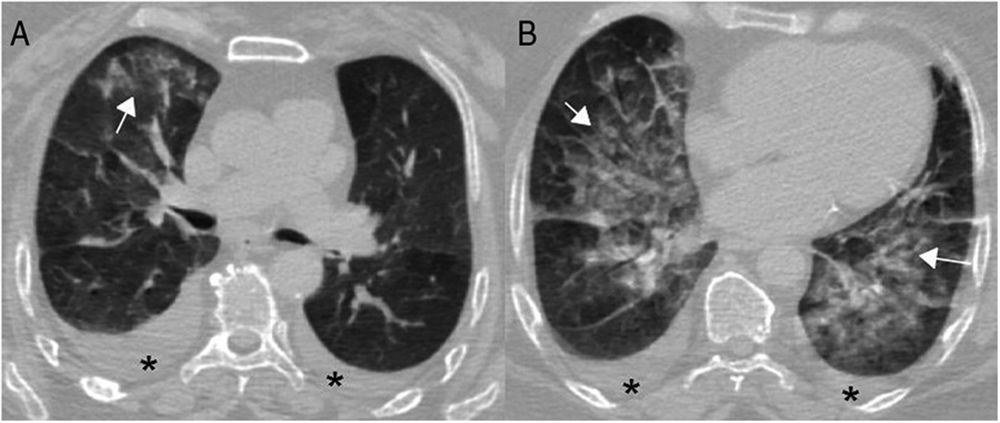
A 64-year-old woman, with no cardiovascular risk factors, previously asymptomatic, transferred to the Emergency Department due to motor aphasia, evident increased breathing effort and signs of cardiogenic shock. The lab tests showed severe coagulopathy. On cranial CT we observed early signs of left frontal infarction, consisting of slight hypodensity, loss of cortico-subcortical differentiation, and early-stage sulcal effacement (Fig. 1, arrows in Fig. 1A, Fig. 1). CT angiography revealed a thrombus in the left M2 segment (Fig. 1 arrow in Fig. 1B). Opacities with alveolar characteristics in the periphery of both lung parenchyma (Fig. 2 arrow in Fig. 2A Fig. 2) were observed in the chest CT, compatible with atypical bilateral pneumonia due to COVID-19 in the context of a pandemic. Bilateral pleural effusion was also seen (Fig. 2 asterisks in Fig. 2) and an extensive diffuse bilateral parahilar alveolar-interstitial pattern (Fig. 2 arrows in Fig. 2B), compatible with acute lung oedema due to acute heart failure. The ECG and the transoesophageal ultrasound showed signs of an advanced inferior posterior myocardial infarction. The patient died 10h after ICU admission despite therapeutic efforts. The radiological diagnosis was supported by laboratory data and positive PCR for COVID-19 in nasopharyngeal swab. The coagulopathy that some patients with severe COVID-19 develop, as in our case, is associated with a high mortality rate.
Please cite this article as: García Espinosa J, Moya Sánchez E, Martínez Martínez A. COVID-19 grave con inicio como neumonía bilateral, ictus isquémico e infarto de miocardio. Med Clin (Barc). 2020;155:188.