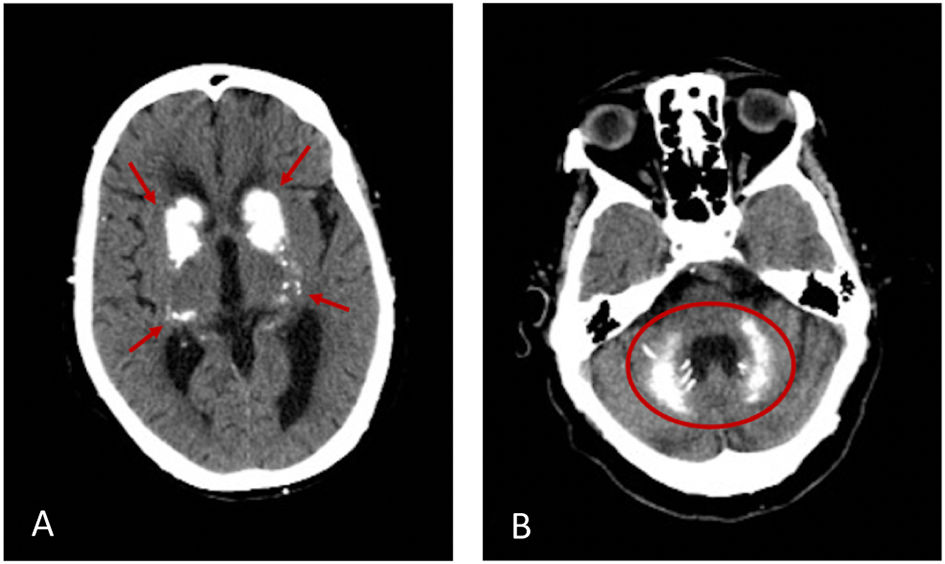
A 72-year-old woman with a past medical history of hypertension, dyslipidaemia, auricular fibrillation, heart failure and epilepsy for the last 3 years and partial thyroidectomy as of 20 years ago presented with a 9-month history of seizures and psychosis and was admitted for investigation. The physical examination showed neglect. Laboratory testing revealed hypocalcaemia 7.2 mg/dl (normal value, <8.8) with hyperphosphatemia 6.9 mg/dl (normal value, <4.5) and hypoparathyroidism with a PTH value of 3.7 pg/ml (normal value, <10). Vitamin D, magnesium, albumin, and thyroid functioning testing came back normal. The brain computer tomography (CT) revealed bilateral basal ganglia calcifications (Fig. 1A, arrows, and B circle). Considering her past medical history, clinical and physical findings, and subsequent investigation exams, Fahr's syndrome was diagnosed. The aetiology assumed was secondary to hypoparathyroidism related to her prior thyroidectomy. She started treatment with calcium and calcitriol with improvement. By using this particular case, authors aim at alerting that in the presence of neuropsychiatric symptoms and basal ganglia calcifications, Fahr's syndrome should be considered even if rare, especially after thyroidectomy. The treatment should be direct to the relief of symptoms and pointed to the underlying cause. Prompt treatment can prevent brain calcifications and neurophysiological disorders.
Información de la revista
Images in medicine
Open Access
Seizures and bilateral basal ganglia calcifications due to hypoparathyroidism after thyroidectomy
Convulsiones y Calcificaciones Bilaterales en los Ganglios basales por Hipoparatiroidismo tras Tiroidectomía
Visitas
489
Ana Sofia Alves
, Ana Maria Carvalho, André Ribeiro, Fernando Salvador
Autor para correspondencia
Department of Internal Medicine, Trás-os-Montes and Alto Douro Hospital Centre, Chaves, Portugal
Este artículo ha recibido
Recibido 28 Junio 2022. Aceptado 14 Julio 2022
Información del artículo
Texto completo
Copyright © 2022. The Author(s)