Introduction
Diabetes mellitus is notably increasing in the world and even more in underdeveloped countries. The number of patients with diabetes is expected to be 228 million by the year 2025, and of this number, 75% will live in under-developed country.1
In 1995, there were 3.5 million patients with diabetes in Mexico, making it ninth among the ten countries with the greatest number of diabetics. Each year 180 000 new cases of diabetes are diagnosed, with more than 36 000 deaths. Each year there are more than 50 000 amputations and more than half are related to diabetes mellitus.2
Traditional treatment for diabetic foot includes metabolic control, debridement of the affected area, use of a suitable antibiotic, and sometimes vessel graft placement to revascularize the extremity. If this treatment fails, it can result in amputation, and the level will depend on the affected area.3
Since the 90's, negative pressure has been used as an aid for healing wounds of the lower limbs with pressures between -50 and -125 mmHg. Pressure is applied continuously to the affected area in patients without problems in tissue blood flow; in these patients, results have been good.4,5 Treating a patient with diabetic foot is a challenge because its etiology is complex. Some patients have neuropathy, others ischemia, and the majority have a combination of both.3 The results obtained with the application of negative pressure in patients with ischemia have not been favorable. Some authors even reject it as a therapeutic alternative in patients with vascular ischemia and diabetes.6 This is why the application of negative pressure in patients with diabetic foot should have different characteristics. First, it must be applied to the entire lower limb to force distal tissue perfusion. It should also be intermittent to allow venous return.
From a hemodynamic point of view, when the limb is sealed in its upper portion and a vacuum is applied, arterial as well as venous blood is forced distally. Afterwards, for a few seconds, the upper seal is loosened, which allows venous blood to return to the heart. This process is performed intermittently. We used the clinical experience with local negative pressure devices reported in the literature to determine how much negative pressure to use.5
Taking the aforementioned into consideration, we designed a negative pressure device (DPN-JAT 2003) that produces a pressure of -125 mmHg. This pressure is maintained for 14 seconds. Afterwards the pressure is released, which allows venous return for another 14 seconds with the cycle starting again when it ends. The intervals imitate the sequence of the breathing cycle. The session lasts 15 minutes at first and is gradually increased to 30 minutes. When the session starts, patients can feel discomfort in the area when the chamber is inflated; this is why we begin with 15 minutes and increase the time gradually. The feeling is that of a blood pressure device when it is being filled to record blood pressure.
We have experience with the use of such a device in patients with pain at rest and in ischemic diabetic ulcers. We have seen that it is very effective in treating pain at rest. It has also shown usefulness with ulcers, although there is very little experience, 7 but the results have motivated the development of this study.
Our objective was to prove the effectiveness of the negative pressure device for healing diabetic foot ulcers with a focus on comparing healing time and the level of amputation with and without the device.
Methods
We carried out an experimental clinical study with 22 patients that attend the General Surgery clinic of a tertiary care hospital that diagnoses diabetic foot. The patients were divided into two groups with 11 patients each; Group 1 was the control group and Group 2, the experimental group.
Patients with diabetic foot, Wagner classification I, II, III, IV, 8 older than 35 and less than 70 years of age and metabolically stable were included. Patients with a Wagner classification V were excluded because amputation is the only treatment. Patients with a diagnosis of autoimmune or neoplastic disease, in dialysis treatment, programmed for revascularization, with a history of active smoking, and with an ankle-arm index <0 5 were also excluded
The groups were randomized and both groups, after metabolic control, received the best treatment available for diabetic foot: antibiotics, wound cleansing with neutral soap three times a day, and debridement of necrotic tissue every other day. The experimental group also received negative pressure treatment. The size of the ulcer, the healing time, and the amputation level were recorded. Resolution of the ulcer in a period of months was considered wound healing, and failure was considered when there was no healing after six months of treatment.
The procedure consisted of placing the limb in a metal cylinder sealed at one end. The limb is introduced into the open end up to the thigh, which is also sealed inside the inflatable chamber together with the limb (Figure 1). Once the limb is completely sealed inside the open end of the cylinder, a vacuum is produced with a pump.
Figure 1. Diagram of the negative pressure device, which consists of a metal tube that is sealed at one end; on the upper end there is a chamber that adjusts to the diameter of the leg. Once adjusted, the vacuum begins, which is intermittent. The chamber is then inflated to produce a seal. A vacuum of -125 mmHg is immediately produced, causing blood to circulate distally.
The following variables were considered: demographic data such as gender, marital status, occupation, and educational level, years of evolution with diabetes or hypertension, mean arterial pressure, hemoglobin, hematocrit, glycemic level, Wagner classification, superficial and deep neuropathy, area of the ulcer, pulses in both limbs (femoral, popliteal, posterior tibial, pedial) and ankle-arm index.
The protocol was approved by the Ethics, Research and Biosafety Committee of the UANL University Hospital. Participants provided informed consent.
Clinical procedure: The patient was hospitalized for two days in the general surgery ward. During the patient's stay a metabolic assessment was carried out and the blood glucose level was stabilized below 150 mg/dL. The area of the ulcer was measured with thick cotton string. This was placed around the perimeter of the ulcer and the area was measured by placing the circle over graph paper where square centimeters and square millimeters were measured manually. Superficial and deep sensitivity was also documented. Superficial sensitivity was measured with a Semmes-Weinstein monofilament and deep sensitivity with a 128 Hertz tuning fork. The monofilament was placed over the ten points described for the foot and the tuning fork on bone prominences.
Culture of the lesion and the first wound cleansing with soap and water were performed to clean the wound and debride necrotic tissue. Finally, hyperoxidized water was sprayed on the wound and honey applied together with a soft bandage. Medical students and family members were instructed to carry out three dressings a day and use the negative pressure device, if indicated. Also, once a week, a medical student was asked to debride the wound, supervise dressings, and assure that negative pressure was correctly applied by photographing the foot and measuring the area of the ulcer.
Statistical analysis: Data were collected and analyzed with SPSS version 11 for Windows. Univariate analyses were used for categorical variables with percentages and frequency, and medians and ranges for numerical values. Inferential statistics. For categorical variable cross tabulation was carried out using the Chi square or Fisher´s exact test. Evolution of ulcer healing was compared using parametric tests (t test for independent groups) with a p value <0 05 p
Sample size: The sample size was calculated using a formula for experimental studies with an n = 11 for each group. A small difference between the experimental and control group was considered (70% vs. 10%).
Results
Both the experimental and the control group were composed of eleven patients each. Most of the patients in the experimental group were men (81.8%), which was slightly higher than the control group, although there was no statistically significant difference. With regard to patient occupation, the experimental group had more workers and small business owners than the control group, 27.3% and 36.4% vs. 9.1% and 27.3%, respectively. There was no statistically significant difference (Table 1).
Average age for both groups was very similar (58.7 years for the experimental group and 60.5 years for the control group). The years since diagnosis of diabetes mellitus in both groups was almost identical (16.3 ± 9.8 years in the experimental group and 16.5 ± 9.1 years in the control group). Glucose blood levels at the beginning of the study were similar in both groups with an average of 144.4 mg/dL in the experimental group vs.156.7 mg/dL in the control group. An important difference was found between both groups with regard to years since diagnosis of hypertension with an average of 13 years for the experimental group, and 7.5 years in the control group (Table 2). Deep neuropathy was present in 100% of the patients and superficial neuropathy in 90.9% in both groups (data not shown). Ulcer staging according to Wagner´s classification had no statistically significant difference, as also occurred with the presence of pulses (data not shown).
With regard to the bacteria found in culture, the most frequent were: Coagulase-negative Staphylococcus sp. in 23% followed by Staphylococcus aureus and Enterococcus faecalis with 9% each. Thirty-six percent of the cultures were negative, which can be explained by the fact that when the patients entered the protocol, they were metabolically stable and under antibiotic treatment.
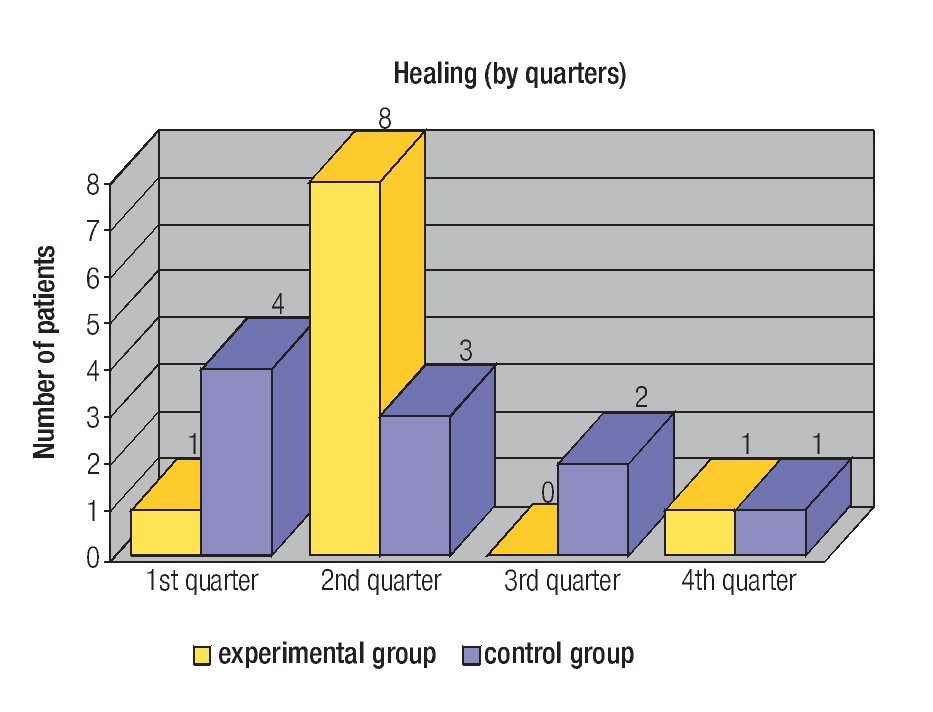
In a comparative analysis of ulcer evolution carried out month by month in both groups, it was found that ulcers at the start of the study in the control group were larger than those of the experimental group; however, at the end there was no statistically significant difference between the groups (Table 3). The experimental group had a more rapid healing curve during the first semester, since nine patients in this group had complete healing of their ulcers in comparison with seven from the control group (Figure 2).
Figure 2. Quarterly healing of ulcers in the experimental and control groups.
Discussion
There was no significant difference between the use of the DPN-JAT 2003 and conventional treatment in the healing of diabetic foot. Although at first there was more healing with the use of the device, this was not statistically significant and at the end, healing was equal in both groups. This study is different from those published in the literature in two aspects: first, the DPN-JAT 2003 is not like other devices, since it produces negative pressure with a tourniquet. The pressure is exerted on the whole limb, while in devices previously described it is exerted only on the affected area. Second, the selection of patients in this study included ulcers from one to 72 cm, with a Wagner classification of I to III and also with decreased pulses. The variables in both groups were homogeneous . There were patients that took up to 12 months to heal. For all practical purposes, we cannot assure that the DPN-JAT 2003 speeds up healing. However, in the results published in the literature with the VAC device, which is the most representative of all, in the best study there was only 112 days of follow up and patients did not have decreased pulses. Healing in this period of time was 56% in the experimental group vs. 39% in the control group with a p <0 04 systematic reviews of the literature carried out with vac device did not conclude that it was useful in healing diabetic foot 8-10
Definitely, more studies are necessary to determine the usefulness of all negative pressure devices, especially the DPN-JAT 2003. It is important to know why there is no improvement in patients treated with the DPN-JAT 2003. It could be related to the type of patients; for example, patients with a certain degree of evolution of the ulcer and with good pulses.
Also it is necessary to consider Error Type II11 since the size of sample is small, taking into account that DPN-JAT 2003 besides the conventional treatment was compared against the control group just with conventional treatment and not against no treatment at all, which is not possible for ethical reasons. This determines that the power of the test to detect the difference is very low. Therefore, statistics explain the absence of significance. Another study with greater sample size and a single type of skin ulcer's patients might be the next step.
It may be necessary to modify the device to obtain better results, since the principle of a beneficial effect for tissue perfusion with negative pressure is theoretically well established.12,13
The number of patients with this problem in Mexico warrants more studies to solve it. It should also be part of the research carried out in health organizations.
Acknowledgements
We thank Dr. Sergio Lozano-Rodriguez of the Scientific Publications Support Office of the Office of the Vice-Dean of Research, Hospital Universitario UANL for his help in translating and reviewing the manuscript.
Dr. Eloy Cárdenas Estrada.
Mr. Aaron Guajardo Lozano.
And the following medical students:
Abraham Izais Gómez, Mauricio Padilla Chávez, Cesar Ernesto Tamez Garza, Eduardo Pérez Contreras, Verónica Elisa Tamez Tamez, Yesenia Isabel Cárdenas Vázquez, Karen Alicia Rodríguez Mireles, Eduardo Zapata Flores.
Corresponding author: Dr. Juan Antonio Tamez del Bosque.
Ave. Francisco I. Madero y Ave Gonzalitos s/n, Colonia Mitras Centro Monterrey, Nuevo León, C.P. 64460, México.
Telephone: (+52 81) 8348 3303.
E mail: juanantoniotamez@yahoo.com.mx
Recibido: marzo, 2010
Aceptado: octubre, 2010