To evaluate the basic knowledge of transfusion medicine of medical residents who prescribe blood product transfusion.
Material and methodsWe evaluated medical residents’ knowledge of transfusion medicine using multiple-choice questions.
ResultsWe evaluated a total of 186 residents from different departments. The mean score was 47.2 (0–100). The department with the highest score was Hematology (61.5). First-year residents achieved a score of 48.4, a score that was greater than those of subsequent years (44.7). Those who had read a practical guide on transfusion medicine obtained a better mean score than those who had not (55.4 vs. 44.6). No association was found between the mean score and the hours of transfusion medicine classes received during undergraduate training. The topic with the lowest score was related to red blood cell transfusion and fresh frozen plasma in emergency situations (7.5).
ConclusionThe results of this study show a general lack of knowledge on transfusion medicine; therefore, we believe it is important to increase the number of topics related to this subject in undergraduate and graduate classes.
Transfusion therapy is one of the greatest achievements of modern medicine. The benefits of blood transfusion are real and the lives of patients with various disorders depend on its use to reduce mortality, prolong life, and improve quality of life.1
Blood transfusion is one of the five most excessively used medical procedures.2 It has become a routine therapeutic procedure despite the availability of cheaper and safer alternatives.3 However, inadequate use of transfusion in hospital settings has been frequently reported. This could be a reflection of a low level of knowledge on transfusion medicine.4
In Mexico, 74.4% of red blood cell transfusions, which is the most frequently used blood product, are unjustified.5 On the other hand, studies carried out in the United States report that academic programs in medical schools related to transfusion medicine are insufficient. Similar findings have been reported with regard to residencies of different medical specialties.4 In other words, medical curriculums do not include transfusion medicine as a learning unit. This is because it is felt that the knowledge necessary to perform transfusions can be acquired from clinical experience instead of programmed education.6
Medical residents’ knowledge of transfusion medicine in hospitals has been determined using multiple choice exams that include essential topics of transfusion medicine.7 In the “Dr. José Eleuterio González” University Hospital, this evaluation has not been carried out. It is necessary to apply an objective tool that demonstrates the knowledge of transfusion medicine in graduate students. Our objective was to evaluate the basic knowledge of transfusion medicine of medical residents who prescribe blood products.
Material and methodsWe carried out a descriptive observational cross-sectional study at the “Dr. José Eleuterio González” University Hospital in Monterrey, Mexico to evaluate the knowledge of transfusion medicine using multicenter studies performed in the United States as a reference.8,9 A 26-item multiple-choice questionnaire was used for this evaluation. Also, demographic data of the participants was collected. The instrument used was reviewed by clinical pathology professors who are members of the Blood Transfusion Committee. Calculations were based on a score of 100, obtained from 26 items, which was the maximum number of questions (3.85 points for each correct answer).
Residents were distributed according to specialty program and postgraduate year; subsequently, departments were chosen according to the use of transfusion in adult patients. Before applying the instrument, approval in writing was obtained from each department. Residents from different areas who prescribe blood transfusions in adult patients were included. Residents who perform blood transfusions in pediatric patients, who do not prescribe transfusions, who were not rotating in the hospital, and who did not want to participate were excluded. In order to reduce the bias in the study, clinical pathology residents were excluded because of their participation in the application of the evaluations. Information regarding the department where they worked, the postgraduate year, previous knowledge of a practical guide of transfusion medicine, the degree of perception of knowledge in the area, and hours of learning related to the topic during undergraduate and graduate classes was also collected.
Statistical analysisThe information obtained was analyzed using SPSS version 20 for Windows. Descriptive statistics were used for numerical variables as a measure of central tendencies and dispersions. Percentages and frequencies were calculated for categorical variables to describe the demographic characteristics of the participants. Means were calculated for each participant, service, year, and topic; ANOVA was used to calculate the statistical differences of these variables. A P value less than 0.05 was considered statistically significant.
ResultsOf the 17 services invited to participate in the study, 14 authorized application of the questionnaire. A total of 186 residents from clinical and surgical areas were evaluated. The greatest number of residents was from first and second speciality years, 31.2% in each of these groups; third speciality year was 23.7% and fourth year or higher was 14%.
When asked if they had previous knowledge of a practical guide in blood product transfusion, only 55.4% answered affirmatively. With regard to self-perception of knowledge of transfusion medicine, 69.2% classified it as intermediate. The rest described it as scarce and advanced at 20.5% and 10.3%, respectively.
Regarding hours of transfusion medicine classes in medical school, 46.2% mentioned having received 3–4h of classes, 45.7% reported 1–2h, and the rest 0h. Regarding hours of transfusion medicine classes during residency, 30.6% mentioned having received 3–4h of classes, 39.2% reported 1–2h, and the rest 0h.
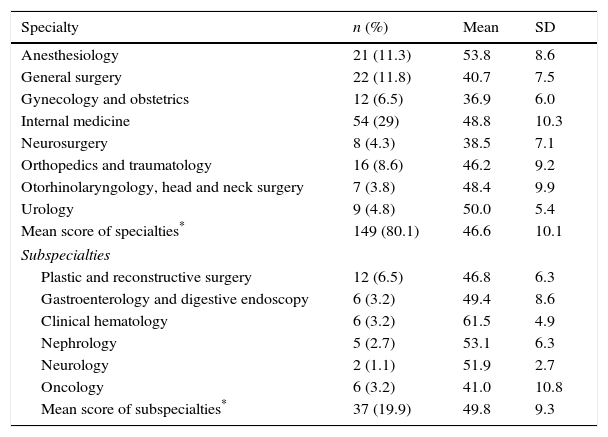
Assessment resultsThe mean global score was 47.2, with a standard deviation of 10. Inter-individual scores ranged from 19.2 to 73.1. Scores ≤42.3 were found in the 25th percentile, scores from 42.4 to 53.7 were found in the 50th percentile, and scores ≥53.8 were found in the 75th percentile. According to department, the highest scores were those of hematology (61.5), anesthesiology (53.8), and nephrology (53.1), (Table 1). The highest individual scores were those of residents from anesthesiology (73.1), hematology (69.2), and internal medicine (69.2). The mean of subspecialties was higher (49.8) than that of specialties (46.6), although this was not statistically significant (P=0.08). Regarding scores according to postgraduate year, residents from the first, second, and third year obtained scores of 48.4, 47.2, and 47.1, respectively. First-year residents did better than subsequent years (Table 2). This downward trend in the mean score in subsequent years of practice was not statistically significant (P=0.476).
Mean assessment score by department (n=186).
| Specialty | n (%) | Mean | SD |
|---|---|---|---|
| Anesthesiology | 21 (11.3) | 53.8 | 8.6 |
| General surgery | 22 (11.8) | 40.7 | 7.5 |
| Gynecology and obstetrics | 12 (6.5) | 36.9 | 6.0 |
| Internal medicine | 54 (29) | 48.8 | 10.3 |
| Neurosurgery | 8 (4.3) | 38.5 | 7.1 |
| Orthopedics and traumatology | 16 (8.6) | 46.2 | 9.2 |
| Otorhinolaryngology, head and neck surgery | 7 (3.8) | 48.4 | 9.9 |
| Urology | 9 (4.8) | 50.0 | 5.4 |
| Mean score of specialties* | 149 (80.1) | 46.6 | 10.1 |
| Subspecialties | |||
| Plastic and reconstructive surgery | 12 (6.5) | 46.8 | 6.3 |
| Gastroenterology and digestive endoscopy | 6 (3.2) | 49.4 | 8.6 |
| Clinical hematology | 6 (3.2) | 61.5 | 4.9 |
| Nephrology | 5 (2.7) | 53.1 | 6.3 |
| Neurology | 2 (1.1) | 51.9 | 2.7 |
| Oncology | 6 (3.2) | 41.0 | 10.8 |
| Mean score of subspecialties* | 37 (19.9) | 49.8 | 9.3 |
SD: standard deviation.
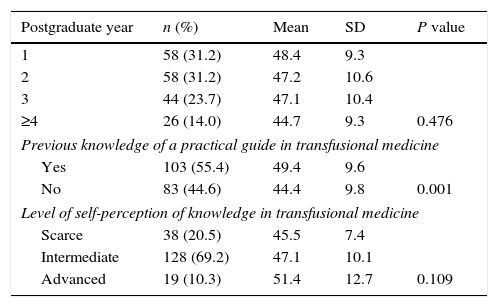
Correlation between survey results and mean assessment scores (n=186).
| Postgraduate year | n (%) | Mean | SD | P value |
|---|---|---|---|---|
| 1 | 58 (31.2) | 48.4 | 9.3 | |
| 2 | 58 (31.2) | 47.2 | 10.6 | |
| 3 | 44 (23.7) | 47.1 | 10.4 | |
| ≥4 | 26 (14.0) | 44.7 | 9.3 | 0.476 |
| Previous knowledge of a practical guide in transfusional medicine | ||||
| Yes | 103 (55.4) | 49.4 | 9.6 | |
| No | 83 (44.6) | 44.4 | 9.8 | 0.001 |
| Level of self-perception of knowledge in transfusional medicine | ||||
| Scarce | 38 (20.5) | 45.5 | 7.4 | |
| Intermediate | 128 (69.2) | 47.1 | 10.1 | |
| Advanced | 19 (10.3) | 51.4 | 12.7 | 0.109 |
SD: standard deviation.
≥4: 4th, 5th and 6th year residents.
A relationship between the score and previous knowledge of a practical guide of transfusion medicine was seen. Those who had previously read the guide had a mean score of 49.4, while those who had not had a mean of 44.4 (P=0.001). There was also a correlation between the main and self-perception of knowledge of transfusion medicine. Those who described it as scarce had a mean of 45.5, those who considered themselves intermediate had a score of 47.1 and those who felt they had advanced knowledge had a score of 51.4; however, this was not statistically significant (P=0.109).
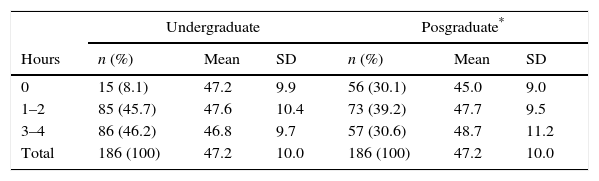
No association was found between the mean score and hours of transfusion medicine classes received during undergraduate training (Table 3). In contrast with hours of transfusion medicine classes during residency, those who reported not having received any type of training in this area had a mean that was lower than those who reported 3–4h (45 vs. 48.7); this was not statistically significant (P=0.08).
Score according to hours of class in transfusional medicine during undergradute and posgraduate education.
| Undergraduate | Posgraduate* | |||||
|---|---|---|---|---|---|---|
| Hours | n (%) | Mean | SD | n (%) | Mean | SD |
| 0 | 15 (8.1) | 47.2 | 9.9 | 56 (30.1) | 45.0 | 9.0 |
| 1–2 | 85 (45.7) | 47.6 | 10.4 | 73 (39.2) | 47.7 | 9.5 |
| 3–4 | 86 (46.2) | 46.8 | 9.7 | 57 (30.6) | 48.7 | 11.2 |
| Total | 186 (100) | 47.2 | 10.0 | 186 (100) | 47.2 | 10.0 |
SD: standard deviation.
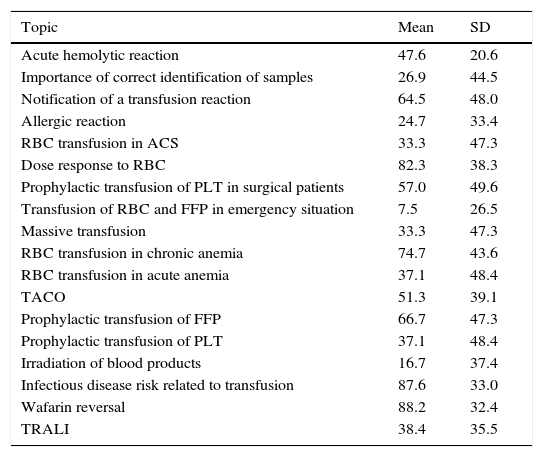
The topics that had the highest averages were warfarin reversal, infectious disease risk related to transfusion, and dose–response to red blood cell transfusion. The topics with the lowest scores were those regarding transfusion of red blood cells and fresh frozen plasma in emergency situations, indications for irradiation of blood products and diagnosis and management of an allergic reaction (Table 4).
Score according to topic.
| Topic | Mean | SD |
|---|---|---|
| Acute hemolytic reaction | 47.6 | 20.6 |
| Importance of correct identification of samples | 26.9 | 44.5 |
| Notification of a transfusion reaction | 64.5 | 48.0 |
| Allergic reaction | 24.7 | 33.4 |
| RBC transfusion in ACS | 33.3 | 47.3 |
| Dose response to RBC | 82.3 | 38.3 |
| Prophylactic transfusion of PLT in surgical patients | 57.0 | 49.6 |
| Transfusion of RBC and FFP in emergency situation | 7.5 | 26.5 |
| Massive transfusion | 33.3 | 47.3 |
| RBC transfusion in chronic anemia | 74.7 | 43.6 |
| RBC transfusion in acute anemia | 37.1 | 48.4 |
| TACO | 51.3 | 39.1 |
| Prophylactic transfusion of FFP | 66.7 | 47.3 |
| Prophylactic transfusion of PLT | 37.1 | 48.4 |
| Irradiation of blood products | 16.7 | 37.4 |
| Infectious disease risk related to transfusion | 87.6 | 33.0 |
| Wafarin reversal | 88.2 | 32.4 |
| TRALI | 38.4 | 35.5 |
*Total score based on a scale of 100.
SD: standard deviation; RBC: red blood cells; ACS: acute coronary syndrome; PLT: platelet concentrates; FFP: fresh frozen plasma; TACO: transfusion-associated circulatory overload; TRALI: transfusion-related acute lung injury.
The “Dr. José Eleuterio González” University Hospital is part of the School of Medicine and has both undergraduate and postgraduate areas. The undergraduate area has an academic program in Clinical Pathology and Internal Medicine, where basic topics in transfusion medicine are reviewed. However, not all the residents in the hospital are graduates of our School of Medicine. Consequently, we have no complete knowledge of their curriculum. This study was carried out to assess medical residents’ basic knowledge of transfusion medicine.
According to the departments that participated in the study, the Hematology Service had the highest score, a finding that is similar to a previous study.10 This could be because physicians from this service receive additional training in transfusion medicine and most of their activities are related to transfusion. On the other hand, the department that scored the lowest was Gynecology, this could be related to limited use of transfusion as a therapeutic option, since it represents approximately 6% of all transfusions in this center, according to a study conducted at “Dr. José Eleuterio González” University Hospital.11
Regarding the score and the year of residency, it is important to point out that knowledge decreased in subsequent years, similar to reports published in the literature. Residents in subsequent years had lower scores than those in the first, second, and third year.8,10,12 This could be because these physicians enter areas that have less contact with transfusion medicine as they advance in their academic training.
In a literature search, we did not find publications that correlate scores and previous knowledge of a practical guide of transfusion medicine. In this study, the mean score obtained by those who had read such a practical guide was greater than those who had not. Furthermore, we observed an association between the score and the degree of self-perception of transfusion medicine knowledge. Those who described their knowledge as advanced had a higher mean score than those who reported very little or intermediate knowledge, similar to that reported by Haspel et al.8
In contrast with previous publications that found better results among those who took classes in transfusion medicine during undergraduate education, there was no association between scores and hours of classes on this topic during medical school in this study. According to the scores obtained with regard to hours of transfusion medicine classes during residency, 30.1% responded that they had no training in this area and 11.7% mentioned receiving 3–4h of classes; these residents had a score of 45 and 48.7, respectively. The correlation between performance on the assessment and a formal education of 3–4h in transfusion medicine during residency was greater than those who did not receive any type of training. This is similar to a previous report.8
Regarding topics in transfusion medicine, the highest scores were in warfarin reversal (88.2), risk of infectious diseases due to transfusion (87.6), and dose–response to red blood cells transfusion (82.3).6 Topics with the lowest scores were transfusion of packed red blood cells and fresh frozen plasma in emergency situations (7.5), indications for irradiation of blood products (16.7), and diagnosis and management of an allergic reaction (24.7), findings similar to that of previous publications.6,8 These areas of knowledge should be considered important for intervention.
The results of this study reinforce previous publications that suggest the need for a greater number of programs on transfusion medicine for medical students, graduates, residents, and those involved in decision-making.6–14 Some studies have implemented a variety of educational interventions, such as Kaur et al., who evaluated physicians’ basic knowledge of the practice of transfusion medicine. Participants in this study received training in addition to a pre- and post-training questionnaire. As a result, there was an increase in the mean score after training. In a similar manner, Rebel et al. published the results of a structured clinical rotation in hematology and transfusion medicine for anesthesiology residents where participants were evaluated pre- and post-rotation. A better performance was found in the post-rotation evaluation.14 However, the effects of these interventions could be short-lived, which is why a combination of strategies is probably more effective, especially if they are performed continuously.
In this study, there was no comparison of transfusion medicine knowledge among attending physicians and residents, because a situational diagnostic is required in order to identify areas of opportunity in the current curricular plan, so it is suggested to consider the affiliated physicians’ evaluation in posterior phases.
A limitation of this study is that the instrument applied was not validated. However, the selection of topics was based on previous literature and each question had a bibliographic basis. Also, the instrument was reviewed by faculty from the Clinical Pathology Department who are members of a blood transfusion committee. We also took into consideration the study carried out in our country that reported a high rate of unjustified transfusions.5
Physicians who prescribe blood transfusions to pediatric patients were not included in the present report since the indications, threshold, and clinical data differ from adults and different questions would have to be made for this population. In order to reduce bias in the study, Clinical Pathology residents were excluded because of their participation in the application of the evaluations.
ConclusionTo ensure transfusion safety for the receptor, adequate knowledge of blood product transfusion, identification and adverse reactions by the physician is essential. The results of the study show that there is a generalized deficit in transfusion medicine knowledge and it suggests the need for educational interventions for residents who prescribe blood transfusion. Emphasis should be placed on areas with more deficits, such as use of packed red blood cells and frozen fresh plasma in emergency situations, indications for blood product irradiation and massive transfusion.
We recommend increasing the number of topics related to transfusion medicine in undergraduate and postgraduate academic programs and suggest extending these studies in other hospitals to evaluate the use of blood products. Also, the Transfusion Committee at the hospital should increase its periodical audits on transfusion practices and implement feedback strategies to improve blood transfusion surveillance.
FundingNo financial support was provided.
Conflict of interestThe authors have no conflicts of interest to declare.
A 27 year old male patient is referred to County Hospital for stab wound in the left lower limb. Vital signs on admission: blood pressure (BP) 90/60mmHg, heart rate (HR) 120 x′, respiratory rate (RR) 21 x′, temperature (T) 37°C. Surgical repair is performed, also in an urgent manner it gets transfused 2 units of red blood cells (RBC) O, RhD positive. Following this the patient reported pain at the infusion site, dyspnoea, decrease BP 70/40mmHg, which it is why is referred to this hospital. On physical examination he was confused and lethargic. BP 70/40mmHg; HR 132 x′, RR 28 x′, T 38.5°C, normal aspect on thorax, breath sounds are perfect, rhythmic heart sounds. Foley catheter is placed to measure urine output and brown urine is observed.
- 1.
Mention your suspected diagnosis:
- a)
Acute hemolytic reaction
- b)
Febrile non-haemolytic reaction
- c)
Bacterial contamination
- d)
TRALI (Transfusion-related acute lung injury)
- a)
- 2.
In the previous patient, what laboratory result will you expect according to the established diagnosis?
- a)
Group O, RhD positive, direct antiglobulin test (DAT) positive, very low serum haptoglobin and free hemoglobin on increased plasma
- b)
Group O, RhD positive and DAT negative
- c)
Group O, RhD positive, DAT negative, normal serumhaptoglobin, arterial blood gas (ABG) with metabolic acidosis data, central venous pressure increased and positive blood culture
- d)
Group O, RhD positive, DAT positive, chest X-ray with bilateral infiltrate
- a)
- 3.
What would be the appropriate treatment for this patient?
- a)
IV fluids, furosemide 40–80mg IV, physical means
- b)
IV fluids, clorphenamine 10mg IV, physical means
- c)
IV fluids, metamizole 1g IV, start broad-spectrum IV antibiotics, physical means
- d)
IV fluids, ventilatory support
- a)
- 4.
To avoid this kind of immediate transfusion reaction is important:
- a)
Leukoreduction
- b)
Correct identification of blood samples from receiver and donor
- c)
Un-cross-matched blood
- d)
Avoid multiparous donors
- a)
- 5.
Any transfusion reaction must report mandatorily to:
- a)
Blood Transfusion Committee
- b)
Hematology
- c)
Blood Bank
- d)
Head of Medical Unit Department
- a)
A 20 year old female patient with no medical history of importance. Go to the emergency room for alteration of consciousness (time and space disoriented). Family reports that three days ago had multiple petechiae in upper and lower limbs. At entry was irritable and restless. On physical examination: BP 100/70mmHg; HR 108 x′; RR 21 x′; T 37.5°C. Jaundiced skin and mucous membranes, slightly dehydrated; thorax and abdomen with multiple petechiae, which do not disappear with digital pressure; normal heart and breath sounds. Lab tests show hemoglobin (Hb) 6g/dL; white blood cells (WBC) 14.2k/μL; platelets (PLT) 20k/μL; peripheral-blood smear shows fragmented red cells (schistocytes) 15/field; 5.1% reticulocytes; DAT negative; group B, RhD positive; lactate dehydrogenase (DHL) 1200IU/L; total bilirubin 5.6mg/dL; indirect 4.5mg/dL; serum creatinine 1.8mg/dL; blood urea nitrogen (BUN) 27.8mg/dL; urinary sediment (30 erythrocytes/field). Proteinuria 300mg/dL in sample isolation. Diagnostic impression: purple thrombotic thrombocytopenic which is why it start plasmatic replacement therapy (PRT) on fresh frozen plasma (FFP) base.
Vital signs during blood products infusion: BP 100/70mmHg, HR 79 x′, RR 16 x′, T 36.5°C. The patient develops skin rash located in some territories as face and trunk, and itching sensation accompanied by breathlessness.
- 6.
What type of transfusion reaction is the patient having?
- a)
Acute hemolytic reaction
- b)
Bacterial contamination
- c)
Allergic reaction
- d)
Anaphylactic reaction
- a)
- 7.
What treatment would you give to that patient?
- a)
IV fluids, hydrocortisone 100mg IV, continue transfusion, continuous monitoring of vital signs
- b)
IV fluids, dexamethasone 8mg IV, maintain permeable airway, suspend the transfusion, continuous monitoring of vital signs
- c)
Continue transfusion, first generation antihistamines, maintain airway, continuous monitoring of vital signs
- d)
IV fluids, acetaminophen 1g IV, maintain permeable airway, suspend transfusion, continuous monitoring of vital signs
- a)
A 72 year old male patient with a history of hypertension of a 15th evolution, treated with captopril 25mg every 12h, with little following of the treatment. Go to the emergency room for chest pain of the oppressive type, high intensity, with irradiation at cervical region and jaw, which start when at rest. On physical examination, the patient is observed with facies pain and anxiety, cooperator, BP 100/60mmHg, HR 85 x′, RR 28 x′, T 36.5°C. Engorgement jugular neck, chest auscultation that crackles with basal predominance. The electrocardiographic study has elevation on the S–T segment in V1, V2 and V3. Laboratory test report the following: Hb 10g/dL; WBC 9.6k/μL; PLT 154k/μL; glucose 355mg/dL; creatine kinase (CK) 411.3IU/L; CK-MB 38.6U/L; troponin I: 0.4ng/mL.
- 8.
What hemoglobin level is recommended for RBC transfusion thresholds in patients with acute coronary syndrome (ACS)?
- a)
≤10g/dL
- b)
≤9g/dL
- c)
≤8g/dL
- d)
≤7g/dL
- a)
- 9.
Mention how much increase would you expect in the laboratory tests after RBC transfusions?
- a)
Increase of 1g/dL on Hb
- b)
Increase of 8% on hematocrit
- c)
Increase of 12% on hematocrit
- d)
Increase of 3g/dL on Hb
- a)
- 10.
Which is the prophylactic PLT transfusion threshold for invasive or surgical procedures?
- a)
≤10k/μL
- b)
≤20k/μL
- c)
≤50k/μL
- d)
≤100k/μL
- a)
A 22 year old male patient is brought to the emergency department for participating in a car accident. On admission he was in a altered state of consciousness, On physical examination BP 90/50mmHg, HR 151 x′, RR 11 x′, T 35.9°C. He had contusion in right temporal region is evident. Thorax with multiple abrasions, increased rhythm of frequency heart sounds, hypoventilated lung fields. Abdomen muscle stiffness. Pale and cold extremities, capillary refill ≥2s. Neurological examination: ocular response (pain), verbal response (emits incompressible sounds), motor response (extension); Glasgow Coma Scale (ECG) 6 points.
Skull TAC shows depressed fracture in the right temporal area, plus epidural hematoma, which is why is transferred to the operating room for a craniectomy. The patient went into hypovolemic shock and it is decided to start massive transfusion protocol.
- 11.
According to the prevalence in Mexican population. What kind of blood components will transfuse when the blood type of the patient is unknown on an emergency?
- a)
Transfuse RBC O, RhD positive; FFP AB; PLT
- b)
Transfuse RBC O, RhD negative; FFP A; PLT
- c)
Transfuse RBC O, RhD negative FFP O; PLT
- d)
Transfuse RBC O, RhD positive; FFP A; PLT
- a)
- 12.
Mention the recommended proportion of FFP:PLT:RBC for massive transfusion:
- a)
1:1:1
- b)
1:1:2
- c)
1:1:3
- d)
2:1:1
- a)
A 65 year old female patient with a history of type 2 diabetes currently treated with NPH insulin 0.5IU/kg/day, and chronic renal failure in peritoneal dialysis. It is entered to hyperglycemia control, it's currently asymptomatic. Physical examination: BP 130/90mmHg, HR 88 x′, RR 15 x′, T 36.9°C, SaO2 97%. BMI 30kg/m2. She was conscious, cooperative, apparent age equal to chronological age. Head and neck: without pathological data. Thorax: well-ventilated lung fields, rhythmic heart sounds without aggregates. Abdomen inflated at the expense of adipose tissue, peristalsis present without hepatosplenomegaly. Lower extremity with edema, peripheral pulses (left pedal decreased), rest is unchanged. Within her lab studies reports: Hb 7.5g/dL; VCM: 69fL; HCM: 21pg; WBC 6.5k/μL; PLT 451k/μL; glucose 535mg/dL; BUN 28mg/dL; creatinine 1.8mg/dL HbA1c 9%.
- 13.
Mention the most appropriate behavior for this patient:
- a)
Adjust insulin dose, starting treatment with iron and erythropoietin and transfuse RBC until Hb is up to 8mg/dL
- b)
Adjust insulin dose, start treatment with iron and erythropoietin and transfuse 2 RBC
- c)
Adjust insulin dose, investigate the cause of anemia, if needed initiate treatment with iron and/or erythropoietin and transfuse 2 RBC or correction Hb until is up to 8mg/dL
- d)
Adjust insulin dose, investigate the cause of anemia, if needed initiate treatment with iron and/or erythropoietin and transfusion will be indicated only if the patient presenting signs of tissue hypoxia
- a)
A 65 year old female patient diagnosed with DM treated with metformin 850mg c/12h. It is brought by family due to fall from their own height, presenting severe pain and limited movement. On physical examination, the patient is conscious, cooperative, with pain facies. BP 100/60mmHg, HR 97 x′, RR 21 x′, T 36.1°C. Chest: lung fields with breath and heart sounds rhythmic with no apparent alteration; abdomen without pathological data; presence of pain on right pelvic limb, local edema, with shortening and external rotation. Radiograph shows displaced femoral neck fracture, so is subjected to hemiarthroplasty, during which it presented important trans operatory bleeding (bleeding grade IV according to the American College of Surgeons).
- 14.
According to the handling of patients with acute bleeding, mention the right choice:
- a)
RBC transfusion in acute bleeding is justified when there is an approximate 30% blood loss
- b)
RBC transfusion in acute bleeding is recommended only if the hematocrit is below 38%
- c)
RBC transfusion in acute bleeding is recommended when the loss is 750ml and unresponsive to crystalloid solution
- d)
RBC transfusion in acute bleeding is justified when there is an approximate 15% blood loss and unresponsive to crystalloid solution
- a)
- 15.
In the first 12h of hospitalization the patient received 5.5l of crystalloid solution, 1.5 of colloid, 9 RBC, 8 FFP and 1 PLT apheresis. After surgery, nurses informed presence of pink discharge from the endotracheal tube. Vital Signs: BP 170/110mmHg, HR 150 x′, RR 24 x′, T 36.3°C; SaO2 75%. Presence of jugular venous pressure, S3 gallop, in addition to lung fields with bilateral crackles. Chest X-ray shows: perihilar opacity is mainly located in the central portions of the lobes and fades toward the periphery image of “butterfly wings”, the presence of Kerley lines, costodiaphragmatic effacement breast and besides cardiomegaly. Mention your suspected diagnosis:
- a)
Anaphylactic reaction
- b)
Transfusion-associated circulatory overload (TACO)
- c)
Transfusion-related acute lung injury(TRALI)
- d)
Bacterial contamination
- a)
- 16.
Select the treatment according to the established diagnosis:
- a)
Reinstate transfusion at a slower drip once the temperature has dropped lower
- b)
Suspend transfusion, administrate furosemide 20mg IV and continue with mechanical ventilation.
- c)
Suspend transfusion, administrate methylprednisolone 30mg/kg IV and continue mechanical ventilation
- d)
Suspend transfusion and administrate broad-spectrum antibiotic
- a)
A 50 year old male patient is referred to Family Medicine Unit because of recent ascites onset. He has a history of hypertension and Type 2 DM currently in treatment with 25mg captopril daily and 1000mg metformine daily. Currently it is referred to as asymptomatic.
Physical examination: BP 130/90mmHg, HR 84 x′, RR 15 x′, T 37.1°C. Thorax: no apparent abnormalities, well-ventilated lung fields, rhythmic heart sounds without aggregates. Inflated abdomen at the expense of ascites liquid, without palpation pain neither hepatosplenomegaly, and he had edematous lower limbs. The laboratory reports: glucose 320mg/dL; albumin 1.8g/dL; creatinine 2.5mg/dL; BUN 41mg/dL; AST 121IU/L; ALT 150IU/L; ALP 136IU/L; total bilirubin 2.1mg/dL, direct 1.9mg/dL, indirect 0.2mg/d; Hb 8g/dL; WBC 10.1k/μL; Platelets 89k/μL; prothrombin time (TP) 21″ (Witness 11.8); activated partial thromboplastin time (TTP) 60″ (Witness 28). We proceed to perform paracentesis diagnosed.
- 17.
Select the right choice related to the patient treatment:
- a)
Transfuse 2 RBC
- b)
Transfuse 4×1011 PLT
- c)
Transfuse 10–20ml/kg FFP
- d)
Does not justify any blood component transfusion
- a)
A 32 year old female patient diagnosed with acute myeloid leukemia (AML) currently undergoing chemotherapy. Attend follow-up consultation finding asymptomatic and hemodynamic stable without evidence of bleeding. She had BP 120/60mmHg, HR 73 x′, RR 15 x′, T 36.7°C. Her laboratory tests: Hb 7.3g/dL; WBC 3.9k/μL; PLT 9.1k/μL; DHL 303IU/L.
- 18.
What is prophylactic PLT transfusion thresholds for oncologic patients?
- a)
≤10k/μL
- b)
≤20k/μL
- c)
≤50k/μL
- d)
≤100k/μL
- a)
- 19.
In case the patient would receive a transfusion directed by his brother, refer to the process that must pass the apheresis platelet unit to prevent graft versus host disease:
- a)
Leukoreduction
- b)
Leucodepletion
- c)
Irradiation
- d)
Washes
- a)
- 20.
You ask for the Informed Consent for transfusions, explaining what the risks and benefits related to it are. Which of the following etiologic agents have the highest risk of infection transmission per transfused blood products unit?
- a)
Hepatitis B virus
- b)
Hepatitis C virus
- c)
Human immunodeficiency virus
- d)
Trypanosoma cruzi
- a)
A 45 year old male patient is referred because management of warfarin overdose. On admission he was conscious, cooperative, hemodynamic stable BP 100/60mmHg, HR 68 x′, RR 15 x′, T 37.1°C. He has shown gingival bleeding and epistaxis; thorax with lung fields and bilateral breath sounds, rhythmic heart sounds without murmurs; soft and depressible abdomen without tenderness and lower limbs with multiple hematomas. Laboratory findings: Hb 8g/dL; WBC 10.4k/μL; PLT 88k/μL; TP+50s (Witness 12.1); INR 6; TTP 40s (Witness 31).
- 21.
Mention the optimal treatment for this patient:
- a)
Manage 10mg IM of vitamin K and transfuse 2 units of RBC
- b)
Transfuse 8 PLT
- c)
Administer 10mg IM of vitamin K and transfuse 20ml/kg FFP
- d)
Transfuse 10U cryoprecipitate
- a)
5h after the transfusion the patient reports severe dyspnea accompanied by profuse sweating. Physical examination: BP 80/40mmHg; HR 125 x′; RR 30 x′; T 38°C; 88% SaO2. He had clammy skin and also presence of cyanosis; while exploring chest, intercostal retractions and supraclavicular are clearly observed. On auscultation bilateral crackles and heart sounds unchanged. Chest X-ray: bilateral infiltrates diffuse, with poorly defined edges, normal cardiac silhouette.
- 22.
Mention action to take in this patient:
- a)
Request complete blood count (CBC), serial blood culture and unit transfused cultivation
- b)
Request CBC and serum IgA.
- c)
Request CBC, arterial blood gas sampling, antibodies to human leukocyte antigens or human neutrophil antigens (HLA, HNA) on donor serum
- d)
Request CBC, reticulocytes, serum bilirubin, haptoglobin, DHL, urinalysis, ABO and RhD group determination, DAT, repeat cross match blood and search for irregular antibodies.
- a)
- 23.
Select the management that would be better for the patient:
- a)
Ventilatory support, IV fluids and maintain diuresis at 100ml/h the first 24h
- b)
Ventilatory support, IV fluids and transfer to intensive care unit (ICU)
- c)
IV fluids, antipyretics and physical means
- d)
Use of nasal prongs, IV fluids and 30mg IV of methylprednisolone
- a)
A 52 year old female patient diagnosed with stage IIIA cervical cancer with a history of multiple transfusions due to underlying disease. Goes to control consult and refers fatigue, weakness, dyspnea on moderate exertion, palpitations and 5 weeks of evolution headache. Physical examination: BP 110/60mmHg; HR 80 x′; RR 17 x′; T 37°C. Thorax with rhythmic heart sounds, well ventilated lung fields without other pathology added. Her laboratory reports the following: Hb 4g/dL; WBC 4.1k/μL; PLT 98k/μL; glucose 97mg/dL; DHL 321mg/dL. 1 RBC is transfused and 1 hour after, the patient reports worsening dyspnea accompanied by nausea, myalgia, chills and low back pain. Her vital signs: BP 80/50mmHg; HR 135 x′, RR 24 x′; temperature 39°C.
- 24.
Select your suspected diagnosis:
- a)
Acute hemolytic reaction
- b)
Bacterial contamination
- c)
Anaphylactic reaction
- d)
TRALI
- a)
- 25.
Laboratory tests that will be ask to confirm the diagnosis:
- a)
CBC, reticulocytes, serum bilirubin, haptoglobin, DHL, urinalysis, ABO and RhD group determination, DAT, repeat crossmatch blood and search for irregular antibodies
- b)
CBC, blood culture and culture of the unit transfused
- c)
CBC and serum IgA levels
- d)
CBC, HLA or anti-HNA antibodies in donor serum
- a)
- 26.
Therapeutic management in this patient:
- a)
Stop the transfusion, IV fluids, furosemide 40–80mg and physical means
- b)
Stop transfusion, 1g Paracetamol IV, combination of broad-spectrum antibiotics and transfer to ICU
- c)
Stop transfusion, fluids IV, diphenhydramine 50mg IV and physical means
- d)
Ventilatory support, IV fluids and transfer to ICU
- a)