Benign intracranial hypertension (BIH) is a neurological syndrome of diverse etiology and obscure pathogenesis. It is also called Cerebral Pseudo-tumor, serous meningitis or otitic hydrocephalus 1. Diagnosis can be established only after other intracranial hypertension causes have been excluded, such as intracranial infection, encephalopathy or a tumor-related injury. The syndrome implies a clinical state where there are no focal neurological symptoms and the patient's state of mind is unaltered. The exact treatment is not established in a definite form, sequelae of this illness are not frequent and the prognosis is generally good.
A large variety of nosologic entities have been found in association with this syndrome. Obesity has been recognized in 14 to 59% of the reported patients in different series 4. It has been observed to be accompanied by some endocrinological states including pregnancy, irregular menstruation with galactorrhea, premenstrual edema, hypoparathyroidism, adrenal insufficiency and therapy with corticosteroids 8–10,13. This same syndrome has been attributed to vitamin A intoxication 14. It has been observed in patients with Sydenhan chorea and in adolescent women with microcytic and hypochromic anemia. Benign intracranial hypertension pathogenesis in these patients has not been explained.
In patients with middle ear or inner ear infection, thrombosis of the lateral sinus has been considered the cause of intracranial hypertension, hence the term “otitis hydrocephalus”. Thrombosis of the lateral sinus in those cases was identified during mastoidectomy and by carotid angiography with a venous phase study.
Amongst other probable Benign Intracranial Hypertension Syndrome etiologies are aseptic cavernous sinus thrombosis and intracranial veins. The latter lesion has been reported subsequent to a closed traumatic head injury 7, a simple skull fracture and related to pregnancy, as well as in systemic disorders which predispose intracranial venous thrombosis like congestive venous heart failure, cachexia, hyperpyrexia, dehydration and the post-partum state. However, in these patients intracranial hypertension was not benign, with a universally fatal evolution. Intracranial venous and sinus thrombosis in said cases frequently lead to cerebral infarction, with concomitant neurological focal signs and seizures, instead of benign intracranial hypertension syndrome.
Furthermore, this diagnosis is questionable in infants with high intracranial pressure syndrome which is attributable to acute vitamin A intoxication; to therapy with tetracycline and chlortetracycline, or to sudden exanthema. In this last situation, the presence of fever and the resolution of hypertension signs and symptoms after diagnostic spinal tap, suggest the term “meningismus”. Meningismus is thought to be caused by a fast dilution of the blood at the onset of fever, making it hypotonic in relation to the cerebrospinal fluid. As a result of this osmotic difference, the CSF volume may increase and temporarily raise intracranial pressure 15.
In one patient, the syndrome was believed to have occurred as a result of an allergic or hypersensitivity process, due to the close relationship between the exacerbation of headache after the ingestion of allergic medications and the improvement of symptoms within a period of 12hours after the institution of antihistaminic medications 11. However, in this particular case there was a history of pneumococcal meningitis, which casts doubts on the meaning of the probable allergic process.
For a better understanding of this syndrome, the experience is presented with 102 patients studied at The Neurological Institute of New York and the University of Florida.
Patient selectionUsing the following criteria, a selection of 102 patients was made, 15 of them seen personally:
- 1.
Rise of intracranial pressure manifested by papilledema and confirmed by measurement of cerebrospinal fluid pressure with a water manometer. CSF pressure was not registered in 30 patients who underwent neurosurgical procedures (ventriculography, subtemporal decompression, and craniotomy) but the subsequent disappearance of papilledema confirmed the impression of intracranial hypertension. The absence of alterations to the visual function excluded the presence of optical neuritis in these 30 patients.
- 2.
Exclusion of the possibility of an intracranial space-occupying lesion, infection of the central nervous system, toxic encephalopathy (lead poisoning), hypertensive vascular disease and obstructive hydrocephalus, through the use of proper neurodiagnostic methods.
- 3.
A normal state of mental functions.
- 4.
Absence of seizures and focal neurological symptoms.
- 5.
Normal CFS glucose and CSF cell count. This data was necessary to exclude, as much as possible, patients with viral infections of the nervous system or those who were sick where the use of antibiotic therapy raised doubts about a possible abscess formation or the presence of partially-treated bacterial meningitis.
Of the total group, 64 were women and 38 men; ages ranged between 25 and 56 years; 39 patients were admitted directly to the private neurosurgical service and the diagnostic and therapeutic use of these patients was often guided by the personal experience of the neurosurgeon on duty rather than by any specific difference in the signs and symptoms of those patients treated medically.
The 102 patients were divided into 6 categories, taking into account two common factors in their clinical evolution and physical examination. The categories were (Table 1):
Thirteen children, ranging from 3 to 13 years of age, suffered from BIH linked to an active middle and inner ear infection. They all displayed the same signs and symptoms of an otic pathology during the month previous to their admission. Only one child with a history of 5 years of intermittent otorrhea was able to be considered as a case of chronic otitis; 5 of them had been treated with antibiotics at the onset of the infection, but the duration of the treatment was always less than 5 days.
They were all admitted within the first week of the first symptoms of intracranial hypertension: headache, nausea, vomiting, dizziness and diplopia. Only 3 children displayed fever at the time of admission (37.5° to 38.5° C). None of them had clinical data of dehydration. Middle ear infection (right ear) was observed during the ostocopic examination of 11 children and in the left ear in two of them. Five children presented sensitivity to pressure in the mastoid region. 13 children presented papilledema and 9 presented external oculomotor paresis. Regarding the injured ear, paresis of the cranial nerve VI was ipsilateral in 3 patients, contralateral in 1 and bilateral in 5. There was no other cranial nerve altered nor was there evidence of thrombosis in the cavernous sinus.
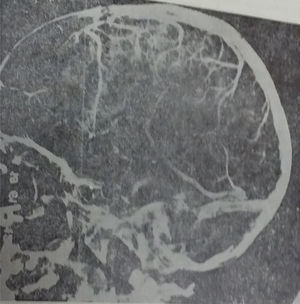
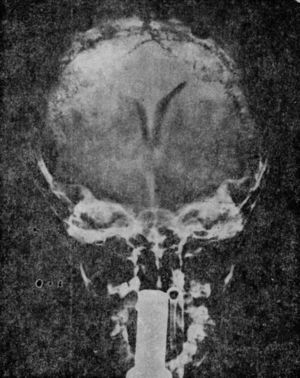
The electroencephalogram (EEG) showed a mild focal bradyarrhythmia in the temporal or occipital ipsilateral derivations in 5 of the patients. Three children presented moderate leukocytes (13,000 to 20,000) and accelerated ESG. Radiological data of mastoiditis was found in 11 out of the 13 children. All these patients presented an increase in CSF demonstrated by a lumbar puncture (of 220 to 600mm of water). Carotid pneumoencephalography and angiography were performed in 10 cases. The venous phase of the arteriogram showed obstruction of the lateral venous sinus ipsilateral to the affected ear in two patients and established the presence of ventricles of normal size. Pneumoencephalography in the rest of the patient was normal (Figure 1).
Other relevant findings included the presence of normal or “low” values in CSF proteins. An elevated Ayala index was found in 6 out of the 8 patients who were measured.* The elevated index in these 6 patients remained this way when measuring repeatedly for 2 weeks to 6 months. By this time the children were asymptomatic and the papilledema had decreased or disappeared. However, CSF pressure remained above 200mm of water, which is compatible with an increase in volume, just as an increased Ayala index suggests.
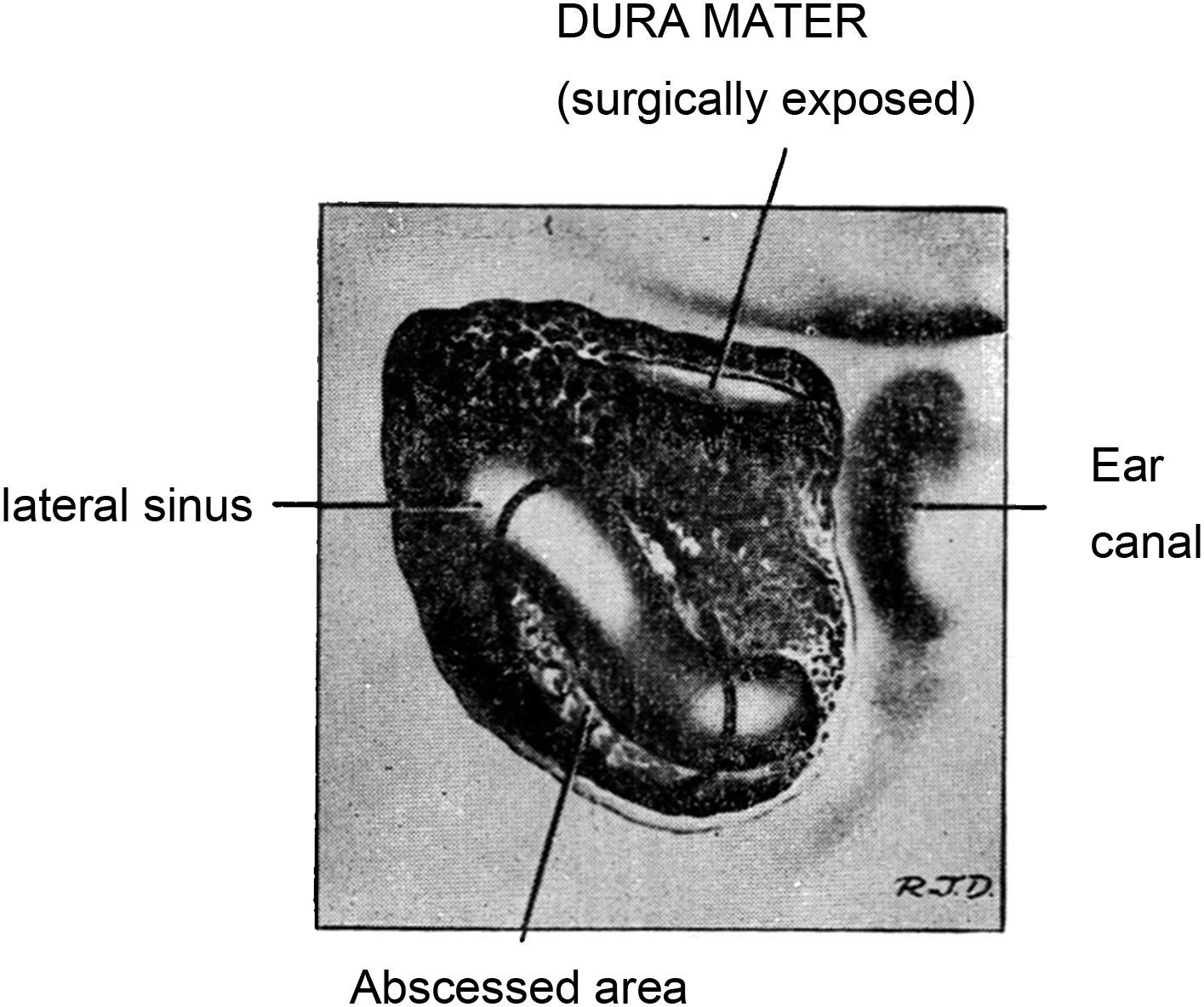
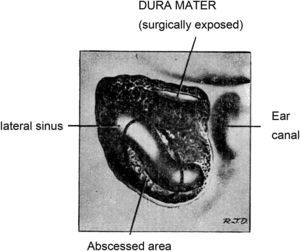
Treatment included mastidectomy, antibiotics, subtemporal or suboccipital decompression, repeated lumbar punctures and anticoagulants. During the mastoidectomy the presence of purulent and necrotic material covering the lateral sinuses and sigmoid was observed in every patient. (Figure 2) After palpation and needle aspiration it was concluded that 2 patients had lateral sinus thrombosis; compression of the lateral sinus and sigmoid was detected in the remaining 8. After the extraction of the necrotic material, the sinuses were filled and patents appeared during the course of 8 years. In one of the two patients with possible thrombosis, the internal jugular vein was tied off at the jugular bulb level. In the other patient the necrotic material covering the venous sinus was removed and therapeutic with anticoagulants was instituted.
Right subtemporal or sub-occipital decompression was performed in 4 patients. This was the only therapeutic measure in 3 of the patients. In the fourth patient a mastoidectomy, a repeated lumbar puncture and therapy with anticoagulants were also performed. In this particular patient, at the moment of decompression, the brain herniated through the incision of the dura mater, making a lobectomy necessary. With the exception of this patient, whose papilledema and intracranial hypertension symptoms did not respond to other therapeutic forms, the decision of performing a surgical decompression in the other 3 patients was made without previous treatment or observation.
At the time of ventriculography or surgery it was concluded that the subarachnoid space was “dilated” in 5 children. With the influence of the arachnoid, CSF flowed out with pressure and the brain, in normal appearance, seemed to re-introduce itself into the cranial cavity. After mastoidectomy, and because of the persistence of papilledema or intracranial hypertension symptoms, 3 lumbar punctures were required. A considerable amount of CSF was extracted with this procedure, large enough (10 to 30 cc.) to reduce the tension levels to normal (80 to 140mm of water). The inadequacy of this procedure was evident when a subsequent lumbar puncture, performed 24 to 48hours later, revealed a CSF pressure equal or higher than the original level. One child who underwent a mastoidectomy and 3 lumbar punctures was discharged 2½ weeks after his admission, as soon as he was asymptomatic and the edema had disappeared. However, this patient was re-admitted to the hospital a week later as a result of a headache and progressive papilledema. He was administered a total of 38 lumbar punctures in a period of 6 months.
Subsequent neurological exams were normal in 7 patients who were monitored for a period of 1 to 5 years and 6 patients who were monitored for a year.
Light “closed” head traumaNine male patients, with ages ranging from 25 to 45 years, suffered a light closed head trauma, a day to 2 weeks before the onset of intracranial hypertension symptoms. The period of time between the onset of the symptoms and its admission with BIH fluctuated between 2 days and 10 months. The trauma caused a momentary loss of consciousness in some patients; it was associated with nausea and occasional vomiting; even when there wasn’t a skull fracture, seizures or any other neurological symptom.
In three patients, a significant symptom and one of early onset was blurry vision; one of said patients suffered from this symptom for a period of 10 months. At the time of admission the patient presented optical atrophy. The rest of them presented papilledema. In the radiological study, one of the children presented suture separation in the skull, without finding any other alterations. The EED was normal in all patients. CSF pressures varied between 200 and 600mm of water in 6 patients. CSF was not registered in the other 3 patients, instead they underwent a pneumoencephalography. The protein content in the CSF was normal in all patients (less than 15mg. % in some) and the Ayala index was elevated in 4 patients for whom pressure measurements and CSF volume were obtained.
The pneumoencephalography was normal in all patients and the carotid arteriography was also normal in two of them.
Two patients with visual acuity alteration received right subtemporal decompression without any improvement in the visual alteration. The patients treated conservatively were observed without using any other type of therapy.
After studying this group of patients during different periods ranging from 6 months to 3 years, it was noted that the neurological exams repeated were normal in all patients, except for 2 cases which had a permanent visual acuity alteration; although this was not progressive.
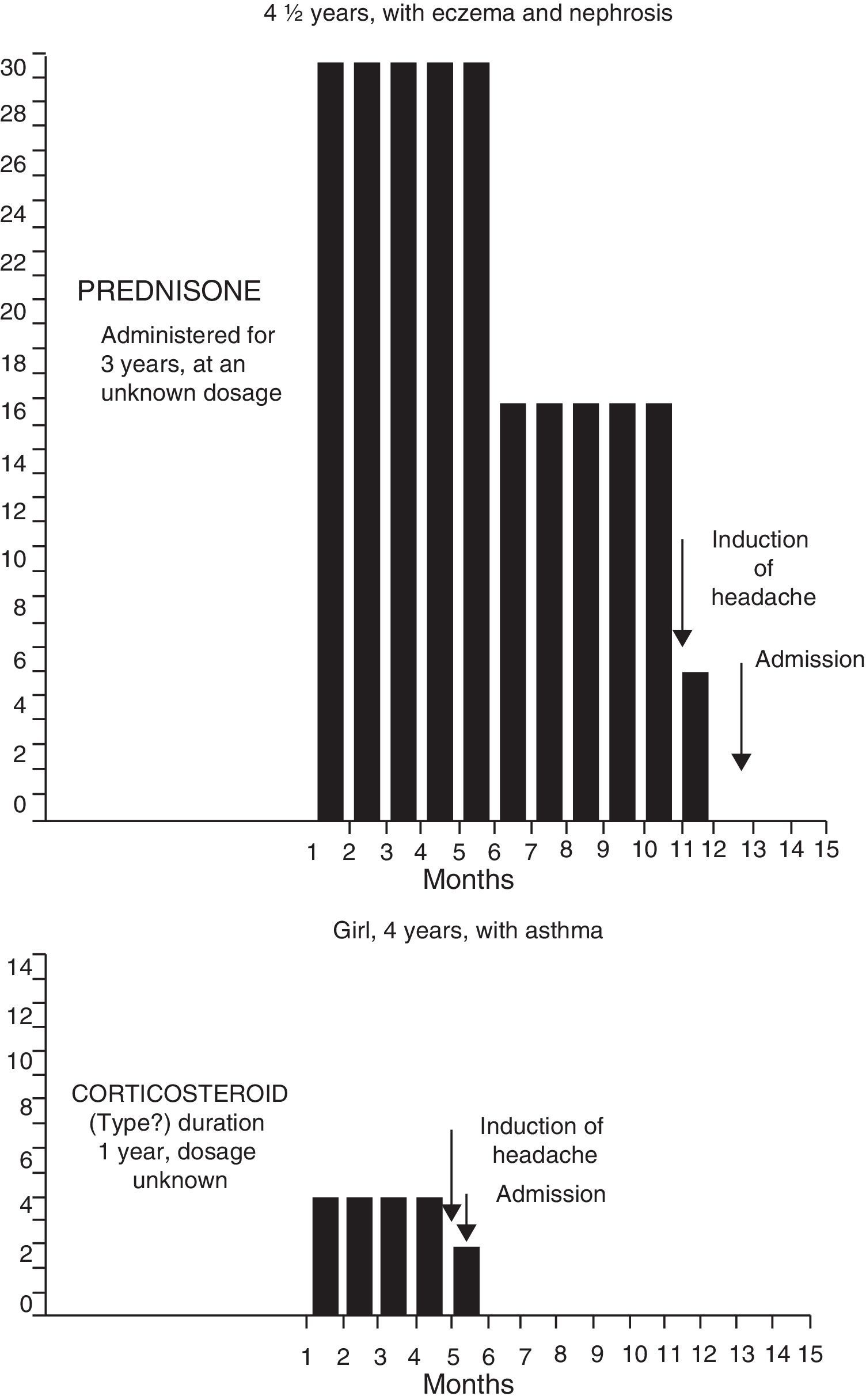
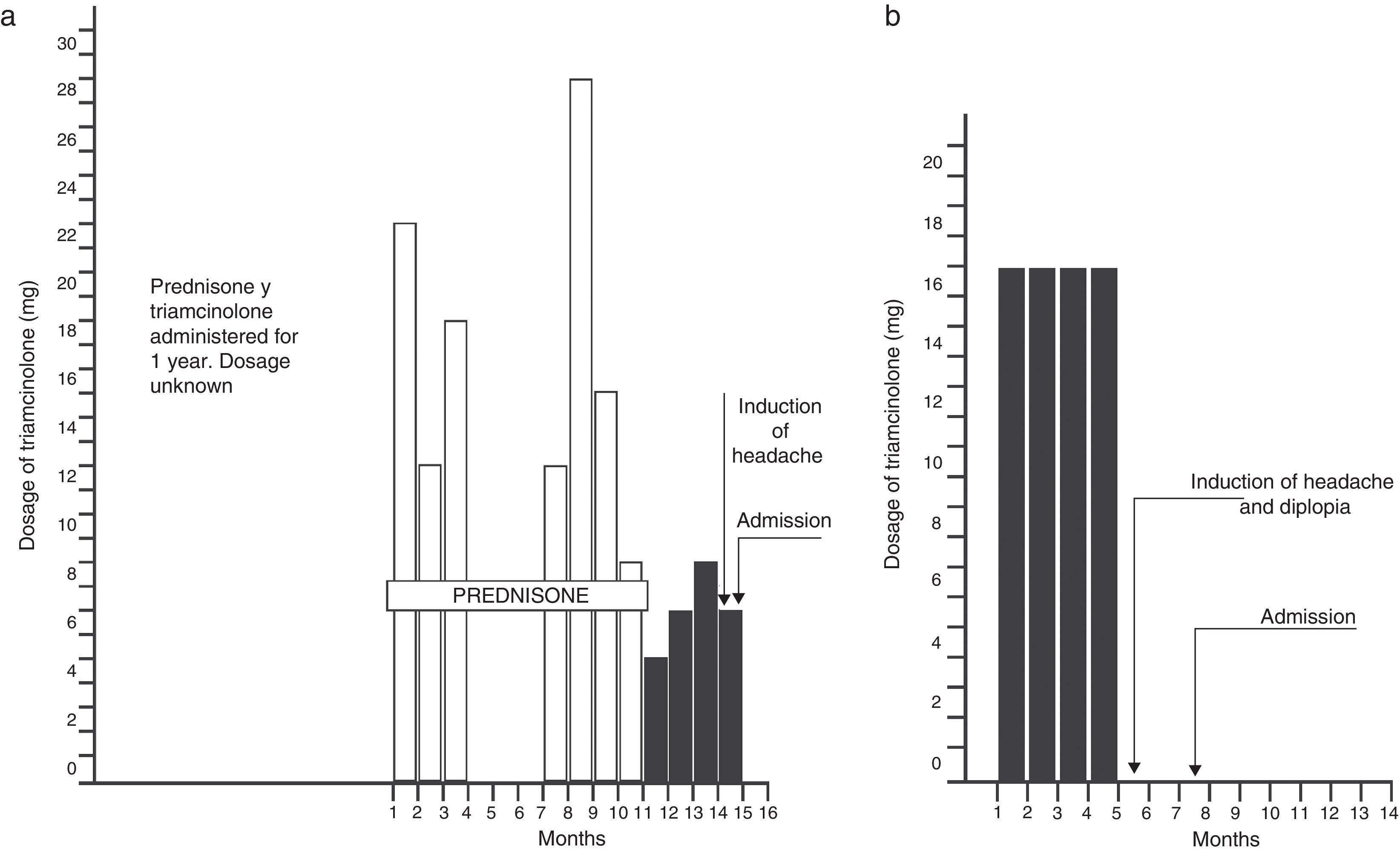
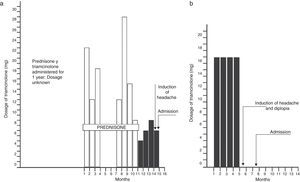
Corticosteroid therapyFour children, between 4 and 6 years of age, received treatment with corticosteroids during variable periods between 5 months and 3 years before the onset of the symptoms of raised intracranial pressure. The conditions under which corticosteroids were administered were the following: eczema in one and eczema and nephrosis in the other, asthma in the third and rheumatic polyarthropathy in the fourth. The medication dosage had been reduced, practically discontinued from 1 to 6 weeks prior to the onset of symptoms. Although 3 of the patients received other types of corticosteroid medications during the course of the conditions mentioned above, triamcinolone was the last preparation given to 4 children during variable lapses of several months to a year. (Figs. 3 and 4).
The patients did not display clinical signs of hypo or hyperadrenalism. Two patients displayed light atopic eczema. All 4 had papilledema and 3 of them had diplopia and bilateral VI-nerve palsy. Cranial radiographies were normal in all cases. There was electroencephalographic alteration in only one patient, conscious in slow activity, moderate and diffuse, without special characters. Visual acuity was 20/200 in the child with polyarthropathy, as well as in those who presented intracranial hypertension symptoms for 6 weeks prior to their admission. Six weeks after their hospital discharge, their vision returned to normal.
The adrenal function studies were normal in one patient (these included determinations of 17-ketosteroids and 17-ketogenic steroids in urine and determination of corticosteroids in plasma before and after the administration of intravenous ACTH). CSF pressures at lumbar puncture varied from 240 to 375mm of water and proteins in CSF were normal.
The pneumoencephalogram was normal in all patients. In one patient the ventriculogram revealed a decrease in the transversal diameter of the lateral ventricles (Fig. 5).
Benign intracranial hypertension. Ventriculography of a 4-and-a-half year old boy with benign intracranial hypertension, which occurred during treatment with steroids. The diminishment of the bodies of the lateral ventricles can be noted in their transverse diameter in the anteroposterior projection, with the forehead facing up.
An empirical treatment was set in 2 out of 4 children with decreasing doses of hydrocortisone acetate (starting with doses of 25 to 50mg respectively) for 3 weeks; Subtemporal decompression was performed in one of the patients treated in this manner. The other 2 patients were observed without an established specific treatment. All the patients were asymptomatic at the time of their discharge; their papilledema had disappeared. It wasn’t possible to obtain any conclusion in relation to the established therapy's effect. All children were normal at their follow up a year or two later. One child received intermittent prednisone during this period due to the recurrence of asthma, but did not show neurological signs or symptoms.
PregnancyEight women, whose ages ranged between 16 and 37 years of age, were in the first semester of pregnancy at the time of the onset of BIH. At the time of their admission they were less than 5½ months pregnant. None of the 5 multiparous women suffered similar symptoms during their previous pregnancies.
Out of the 8 women, 4 were obese, having suffered this alteration for at least 3 years prior to their time of admission. Despite the fact that the initial symptom was the headache in all patients, 7 of them complained mainly about intermittent blurry vision or escotoma. There was no evidence of toxemia or peripheral thrombophlebitis. One patient had mild periorbital and pretibial edema. Papilledema was found in all 8 patients and one of them additionally presented bilateral paralysis of the external oculomotor nerve.
Cranial radiographies and EEGs were normal in all patients. In 6 out of the 8 patients, CSF pressure at lumbar puncture varied between 230 and 430mm of water after surgery. The remaining 2 patients reported normal CSF pressure. CSF protein values were normal (less than 15mg% in 3 cases). The pneumoencephalography was normal in 5 patients, from which one displayed a normal carotid arteriogram. In 3 patients, a lumbar puncture was the only diagnostic procedure performed.
Three patients, including two with altered visual acuity, received surgical intervention (Subtemporal decompression). In one of these patients, visual acuity returned to normal values 3 weeks after the surgery, and remained unaltered (20/70) in the other.
Among other forms of treatment, there was the use of a hypo-caloric diet for the 4 patients with obesity. One of the obese patients lost 3.157kg during her hospital stay; however, after abandoning her diet, re-gained 3.608kg in a period of 12 days and was readmitted to the hospital with recurrent papilledema and headache.
All pregnancies (except for one) were completed without obstetric or post-partum complications. One patient suffered a miscarriage a week after the onset of BIH symptoms. 12 patients were in their 3rd trimester of pregnancy (approximately). After an examination of the patients about 6 to 18 months after their hospitalization, they were all asymptomatic and normal from a neurological point of view.
Probable endocrine or metabolic alterationsThirty nine women, between the ages of 11 and 49 years of age, had BIH associated with what could be considered an endocrine or metabolic alteration.
- A)
MENARCHE. Seven children between 11 and 13 years of age began developing secondary sex characteristics at the time of the onset of intercranial hypertension symptoms. Only one of them had menstruated, (menarche 1 month before her admission). Another girl had been taking 150,000 units of vitamin A for a period of 2 weeks prior to her admission. There were no dermatological signs of intoxication caused by vitamin A and the levels of said substance in serum were normal, (determined 3 days after the drug had been suspended). One girl was obese.
- B)
MENOPAUSE. Six women, all between 40 and 49 years of age, were beginning their climacteric period and had had occasional periods of amenorrhea during the course of the previous year prior to their admission. In addition to the intracranial pressure increase symptoms which these patients presented, there were manifestations of the vasomotor type, such as “hot flashes”, sudden increases in sweating, intermittent flushing, etc. A seventh patient, a 35-year-old woman, was going through menopause after the surgical removal of her polycystic ovaries, which had been performed approximately a year before her admission to the hospital. Two out of the six patients were obese.
- C)
MENSTRUAL DISORDERS. A different group of 7 women, agers ranging from 20 to 36 years of age, presented major irregularities in their menstruation during variable periods between 3 months and 3 years previous to the onset of intracranial hypertension symptoms. Two of these women suffered frequent episodes of intermenstrual bleeding; during hospitalization a dysgerminoma was found and removed in one of them. The most common disorder was amenorrhea; 5 patients presented it intermittently for periods of 3 to 5 months at a time. All of them were going through a period of amenorrhea at the time the noticed the BIH symptoms. 2 of the 5 patients presented hirsutism and galactorrhea. One of these two patients began lactating spontaneously when the menstrual flow reappeared 2 days after having a right subtemporal decompression performed. The adrenal and thyroid function studies were normal, as well as the excretion of the follicle-stimulating hormone. The other patient, a 23-year-old obese woman, complained of intermittent lactation and amenorrhea for a period of a year and a half prior to her hospitalization. Neither of the two patients was pregnant.
- D)
OBESITY. The remaining 19 patients of the group of 39 were between the ages of 15 to 45 and obese. These patients, in addition to the 4 women noted in this category, had been overweight for at least 2 years prior to their admission (body weight ranging between 75.600 and 105.300kg). There were slight menstrual irregularities in 7 out of the 19 obese patients, for a period of 2 to 3 years, including intermenstrual bleeding and occasional episodes of amenorrhea.
In 24 out of the 39 patients the first and most alarming symptom was visual acuity alteration. In one patient, visual acuity was reduced to the perception of light with one eye, and was less than 20/70 in another 6. Special attention was given to 3 patients with hemianopsia (their clinical course is described later).
There were radiological symptoms of intracranial hypertension in 6 of the 39 patients (erosion of the sella turcica or posterior clinoids); the size of the sella was normal in all cases. There was minimum and diffuse slow activity in the EEGs of 5 patients; the EEGs of the remaining 34 patients were normal. Adrenal cortical function tests were normal in the 6 patients studied and the simultaneous measure of serum osmolarity and CSF were normal in 4 women.
Cerebrospinal fluid lumbar pressure fluctuated between 240 and 600mm of water in 25 out of 27 patients. Normal pressures were recorded in two patients after surgery (Subtemporal decompression). CSF proteins were normal in all patients (less than 15mg % in 8). In 6 patients the Ayala index remained elevated for periods of up to 3 to 6 months after hospitalization, where they performed repeated lumbar punctures during asymptomatic periods.
The pneumoencephalogram was normal in all patients, and in 8 cases the carotid arteriogram was also normal. Subtemporal decompression was performed in 26 of the patients, including 3 whose decompression was preceded by an exploratory frontal craniotomy (practiced based on suggestive clinical symptoms and radiological findings). Another obese patient underwent a suboccipital craniotomy which resulted in the death of the patient after an uncontrollable infratentorial bleed. The autopsy revealed, in addition to the hemorrhage, the presence of a small acidophilic adenoma of the hipofisis that did not erode nor enlarge the sella turcica. No endocronogical studies were performed.
Out of the 12 patients who underwent subtemporal decompression due to visual alteration, 7 presented improvement in the visual function after surgery. This includes 2 patients with homonym hemianopsia, where subsequent studies showed the complete disappearance of this inexplicable finding. The remaining 5 patients with visual abnormalities who received surgical treatment did not show improvement of the visual function.
Out of the 26 patients treated surgically, 12 were admitted directly to the Neurosurgery Service, where the management of the patients was decided by the corresponding neurosurgeon. Complications after the surgery included focal seizures (contralateral, to decompression) in 2 patients, and transitory worsening of visual acuity in another 2.
Subarachnoid space was found “distended” in 18 of the operated patients. Cortical biopsies in 3 patients did not reveal abnormalities. In another 4 patients the brain seemed to protrude through the dura mater.
Serial lumbar punctures were performed in 12 patients for periods of 1 to 6 months. Improvement was noted in the visual function in 4 out of the 5 patients who were not treated surgically. CSF pressure at the last lumbar puncture was still above 200mm of water in 9 of the 11 asymptomatic patients whose papilledema had disappeared; however, the elevation of CSF pressure was always lower than the pressure originally recorded.
A hypocaloric diet with or without dehydrators (i.e Manitol at 20%) was utilized as a therapeutic measure in 24 women in the group who were obese. This was the only form of treatment in 8 patients after the diagnostic procedures were performed. All 8 patients were discharged in less than 3 weeks and were normal when studied 1 to 3 years later.
Therefore, 47 of the 102 patients of this series were women who were pregnant or presented signs and symptoms of some endocrine or metabolic change; however, it is certainly suggestive that a hormonal alteration may be linked to the development of intracranial hypertension; it is not possible to obtain definite proof of this link within this study.
Non-related and miscelaneousThe remaining 29 patients constitute the heterogeneous group of 14 men and 15 women, with ages ranging from 8 to 58 years of age. There were no common clinical facts that could separate them in defined etiological categories. However, 13 patients suffered from mild extracranial inflammatory diseases such as: paranasal sinuses infection (5), purulent conjunctivitis (3), tooth abscesses (21) and another 3 patients suffered from recent infections of the upper respiratory tract. There are no clinical or para-clinical data (CSF test) of intracranial generalization in these conditions.
As observed in previous groups, visual alterations were the most significant manifestations in 18 out of the 29 patients.
Radiological tests of intracranial hypertension (erosion of the sella turcica) were found in 3 patients; ethmoid sinusitis in the first, maxillary sinusitis in the second and frontal in the third. There were slight encephalographic alterations in 4 of the 29 patients, translated fundamentally by the diffuse slow activity. There were no abnormalities in the rest of the patients. The studies of cortical adrenal and thyroid functions were normal in 4 of the women.
CSF lumbar pressures were between 200 and 600 of H2O in 17 patients; there was no CSF registered for the other 12 patients surgically treated; CSF proteins were normal (less than 15mg% in 4 cases).
Patients treated conservatively who had a binocular vision of 20/70 improved to 20/20 after repeated lumbar punctures. Nine patients did not receive specific therapy and were asymptomatic at the time of discharge, 2 to 4 weeks after ventriculography; all of the patients were fine 6 months to 3 years later.
Twelve out of twenty nine patients checked after their hospital discharge (between 1 and 17 years later) were normal from the neurological point of view, as well as the other 17 who were checked for a period shorter than 1 year.
Duration of symptomsThe duration of intracranial hypertension symptoms was, in general, shorter in children with otic infection (average of 6 days). In other patients the symptomatic period fluctuated, usually between 3 weeks and 2 months; however, it was difficult to evaluate the starting date of the symptoms in many patients due to the ambiguity of their clinical manifestations. In fact, 10 patients experienced chronic headaches and intermittent blurry vision for periods between 6 to 18 months prior to their admission. With the exception of 9 patients who were readmitted more than 2 months after their hospital discharge, the duration of their symptoms, without taking their treatment into account, varied between 2 to 7 weeks after their admission.
DiscussionPathogenesisIntracranial pressure depends on a) the volume or density of the brain and spinal cord, b) CSF volume and c) brain blood flow and intracranial blood volume inside the craniospinal vault. An increase in one of these factors results in an increase in the pressure inside this vault, unless there is a compensatory descent of one of the two remaining factors. The inadequacy of these compensatory mechanisms in many pathological states results in an increase in intracranial pressure.
Acute and important fluctuations of blood pressure, alterations in CO2 concentrations and, to a lesser degree, the content of oxygen and blood Ph., are factors that affect the brain blood flow and result in intracranial pressure changes. In the series of patients presented, none of the alterations mentioned above manifested.
Based on clinical or neuropathological grounds, there are insufficient data to attribute this syndrome to an increment in brain tissue mass. Signs of mental dysfunction are commonly found in other neurological states where there is diffuse cerebral edema, such as alcoholic or hypertensive encephalopathy. In fact, if the diffuse cerebral edema existed in BIH, its severity would not be enough to raise intracranial pressure and at the same time preserve mental state. Despite this, cerebral edema cannot be totally excluded as the physiopathological base of this problem. At the moment of surgery, 9 patients of this series presented bulging of the brain after dural incision. One of them was a child with lateral venous sinus occlusion. Due to the lack of retention of CO2 during anesthesia, this finding suggested the presence of “cerebral swelling”. The pneumoencephalographic finding of small ventricles in some of these patients suggested this alteration as well.
With the exception of the rare cases of autopsies in patients with intracranial venous sinuses thrombosis and otic infection, where the brain was found to be normal, the main source of pathological material in BIH patients comes from brain biopsies. Changes of said specimens have been described as “consistent with cerebral edema affecting gray matter as well as white, including intracellular and interstical zones”. However, these findings have been considered contrived. In this series, cerebral biopsies were performed in 5 patients, none of whom displayed cerebral bulging during surgery and gray and white matter were found to have normal characteristics in the routine histological exam; the brain of the obese woman who died as a result of technical operative difficulties was normal, except for the iatrogenic hemorrhage of the posterior fossa, and the small pituitary acidophil tumor. There is no report of electronic microscopic studies or biochemical determinations in the studied tissue in different reports of medical literature.
The pathogenesis of this syndrome can also be related to the increase in CSF volume; the amount of CSF represents a balance between the degree of production and absorption. An imbalance in this dynamic state (over-production or low absorption) without proper compensator changes in the blood volume and cerebral blood flow or cerebral tissue, would result in a rise of intracranial pressure.
Unfortunately, there are no reliable methods which can measure CSF volume in human beings in a precise way; however, the findings in the present series favor the hypothesis that, at least in some BIH patients, there was an increase in CSF. In 46 patients, at the time of ventriculography or decompressive surgery, it was noted that there was an “enlargement” of the subarachnoid space with CSF as tension. By affecting the arachnoid, the liquid flowed towards the outside and the normal brain or “wetbrain” seemed to reintegrate within the limits of the cranial cavity. This rare finding of a dilated subarachnoid space, with a normal or “small” ventricular system, has been found repeatedly in different reports in the literature. Foley has referred to this finding as contrived and it has been named a part of the general edematous process by Sahs and Joynt. Symmonds considers it to be the result of an alteration in the function of arachnoid granulations, and as a possible manifestation of some physiological defect in the absorption of CSF, according to Silverstone. This apparent CSF “enlargement” was greater than normal. According to certain authors, such Foley, Sahs, Solis and Sweet, if this were correct, the ventricles would be bigger than normal, and since small or normal ventricles have been found in this syndrome, this possibility has been discarded.
In the present series, the Ayala index, which can be considered a gross assessment of CSF volume, was elevated in 34 out of 41 patients. There is much criticism about the validity of this procedure; despite this, in absence of a more reliable technique to measure the amount of CSF, an elevated Ayala index suggests that the fluid volume was greater than normal. The presence in many patients of low proteins in CSF, as well as those cases reported in medical literature, would have to sustain this idea of an increase of CSF volume, considering there is a dilution in its level of proteins.
The degree of CSF formation has been calculated based on two different techniques, in 15 cc. and 450 cc. a day. There hasn’t been an estimation of CSF formation in pathological states. Sweet et. al. reported that the concentration of Na 24 in the ventricles of BIH patients was between 61 and 88% of the plasmatic levels an hour. These results were comparable to those obtained in a normal control. However, due to the fact that it is not possible to directly relate the degree of sodium entrance to the presence of intracranial hypertension, it is not possible to make an interpretation of the fluid exchange dynamic. In this report, CSF and serum osmolarity were the same in 4 patients. This seems to exclude the possibility that there is an increase in CSF volume due to the differences of osmotic pressure. The obstruction of the drainage routes should be considered as a possible cause of CSF increase. In clinical situations where there are basilar arachnoiditis (i.e. tuberculous meningitis) or a frank dilation of the ventricles, impeding CSF flow, it is possible to observe dilation of the ventricles in the pneumoencephalographic study and not the normal or “small” ventricular system as seen in this syndrome. Although, if the point of obstruction were located in the arachnoid villi, it is to be accepted that instead of ventricular dilation, there would be an increase in CSF volume that would be evenly distributed in the whole craniospinal subarachnoid space, as well as in the ventricles, and it would be manifested only by a distended subarachnoid space. Welch and Friedman have demonstrated that subarachnoid villi function as valves or a flow route for CSF towards the venous sinuses. However, these structures have not been studied in this syndrome.
The pathogenesis of BIH in patients with otic infection is related to the obstruction of intracranial venous flow through the lateral venous sinus. In the present series, a compression of the lateral venous sinus was observed (with or without thrombosis) at the moment of mastoidectomy and it was demonstrated by carotid arteriography. The main pathway for intracerebral venous drainage is the upper longitudinal sinus, which normally drains directly towards the right lateral sinus. The right lateral sinus is larger than the left. This can explain the higher frequency of affection of the right side in BIH syndrome (11 out of 13 cases).
In 2 patients with obstruction of the left lateral sinus, it was possible to suggest that this was the crucial drainage pathway, or that the thrombus originated within the lateral sinus and spread until it occluded the torcular herophili, thus interfering with the total drainage. A sustained elevation of intracranial venous pressure produces a chronic rise in CSF pressure. It is presumed that the inadequacy of antibiotic therapy prior to the patient's admission, the immaturity of the middle ear and the proximity of the lateral sinus to the underdeveloped mastoid air cells, are factors resulting in the sinus pathology observed in BIH in children. The preponderance of male over female remains unexplained (12:1).
Sinus thrombosis may be invoked in patients with closed cranial trauma, where the lesion of a venous sinus with major drainage, or the extension of an incidental venous thrombosis towards a vital drainage zone, may have compromised the pressure system. Nevertheless, the absence of cranial fracture in all 9 patients and the negativity of the carotid angiographic study tend to discard this theory.
In the syndrome associated with the administration of corticosteroids, pregnancy and the alteration of the metabolic or endocrine function, BIH pathogenesis cannot be based in venous sinus thrombosis, which is stressed by the negativity of the angiographic study in 8 patients, where no obstruction of the venous sinus was observed in the arteriogram.
In the 4 children who received therapy with corticosteroids shortly before their admission, or in those who had reduced the medication dosage, intracranial hypertension could have been related to “relative” adrenocortical insufficiency. There are no lab data to base this hypothesis on and these patients did not show clinical manifestations of this problem. Children who were taken off the corticosteroids after taking the medication for either a long or a short period of time, demonstrated states of relative adrenal insufficiency substantiated by the decrease of excretion of corticosteroids. In fact, there was a report of 2 children with BIH and adrenal insufficiency; these children had been previously administered corticosteroids. The association of Addison's disease with the increase of intracranial pressure in 2 patients has been reported. At the time of surgery these patients were considered to have cerebral edema. If this was in fact cerebral edema, a biochemical alteration could be expected in this tissue, similar to the salt and H2O increase observed in the edematous tissue (white substance) adjacent to brain tumors. Davenport found normal salt and water content in the brain of adrenalectomized rats. On the other hand, studies with radioactive isotopes in adrenalectomized animals have revealed cerebral potassium and sodium exchange alterations, suggesting that, in suprarenal insufficiency, there is an abnormality in the dynamic of intracranial fluids and in the mechanisms of ion exchange. However, this data tells us little about the effects of steroids in the brain. In view of the large number of patients receiving corticosteroid therapy and the apparent rarity of BIH in said patients after discontinuing the medication, one must assume that there are additional factors which must play an important part in the pathogenesis of this syndrome. Even though it is thought that there is a certain hormone imbalance in women with alterations in their metabolic or endocrine functions, there is no convincing information which suggests which hormone may be responsible for this syndrome. In fact, normal studies of adrenal and thyroid functions in 10 patients studied in the present series tend to eliminate the concept of hormone imbalance. Nowadays, consequently, with the exception of patients with mastoiditis and lateral sinus obstruction, BIH pathogenesis is purely speculative.
TreatmentEven though the BIH diagnosis is often established only after the encephalography and/or the angiography have excluded the possibility of a tumor lesion, the syndrome may be suspected in some patients, and diagnosed correctly and treated definitively based on history and clinical findings.
The otoscopic examination, mastoid radiographies and carotid arteriogram (venous phase) are the most efficient elements for the diagnosis of a patient with obstruction of the lateral sinus secondary to otic infection. The angiogram helps to exclude the presence of brain abscess or ventricular dilation, which can be caused by a silent mass in the mid-line or posterior fossa. The specific recommended treatment is mastoidectomy, with the extraction of infectious and necrotic material which covers the sigmoid and lateral venous sinuses, as well as antibiotic therapy. There are no established criteria for the indication of thrombectomy. CSF must be examined, looking for the presence of blood or signs of infection. In general, the use of anticoagulants is not desirable, due to the possibility of a hemorrhagic infarction which accompanies cerebral venous thrombosis. The use of dehydrator agents (intravenous urea) is theoretically contraindicated in view of the presence of a thrombosed venous system. The resulting dehydration will certainly facilitate the formation or spreading of venous and sinus thrombosis. In addition to the drop in CSF pressure with osmotic diuretics, administered in parenteral form, it is a temporal effect (less than 24hours) and it may be followed by a “rebound” effect. The continuous use of said agents in order to maintain a low CSF pressure would be dangerous for the brain as well as for other organs. There are very few rational bases for the use of any oral dehydrator agent (liquid glycerin). However, other dehydrator agents have been used, such as Manitol at 20%, with better results, wide tolerance and practically without the “rebound” effect.
The precedent of administration of corticosteroids, particularly when the dosage of the medication has been reduced or discontinued, suggests that the syndrome is a result of adrenal insufficiency, and that the specific therapy is hormone replacement. Even though 2 of the 4 patients in this series were treated with hydrocortisone, the need of a substitutive hormone therapy may be questioned, in view of the asymptomatic clinical state of the patients (In the rest of their apparatus and systems), the lack of confirming laboratory data and the experience with the other 2 patients who were not administered specific therapy.
In the past, in order to establish a BIH diagnosis, the diagnostic procedure of choice was a ventriculography. However, there is a certain reluctance to practice ventriculography in the presence of a normal or “small” ventricular system. As an alternative, one may suggest bilateral carotid arteriography followed by a pneumoencephalography, if the test with contrast does not indicate ventricular dilation. In the presented series, the danger of ventriculography was confirmed in 4 patients who developed sudden worsening of vision or deterioration of vital signs after this diagnostic procedure.
In obese patients, a therapeutic measure may be a reduction of body weight. In one patient of this group, this type of treatment would be supported by the fact that in her, intracranial hypertension signs and symptoms reappeared after she regained the lost weight. The prolonged use of oral diuretics and the restriction of salt did not offer additional benefits to the patients treated with a dietary regime. Cortisone was administered to patients with menstrual irregularities and BIH but the reasoning behind this treatment is still in doubt.
Other measures have been utilized in order to maintain a normal intracranial pressure, such as surgical decompression and repeated lumbar punctures as a supportive treatment. The threat of alteration in visual function is generally what calls for the need to apply these measures. Out of the 23 patients treated with repeated lumbar punctures, it was noted that in 5 of them, CSF pressure was as high in the second puncture as it was in the original puncture performed 24 to 48hours before. In 14 patients CSF pressure remained above 200mm of H2O at the end of the repeated lumbar punctures (up to 6 months later). Therefore the value of serial lumbar punctures is not clear. In this series, 23 patients with accentuated deficit of the visual function were surgically decompressed (subtemporal decompression); an improvement was noted in 13. Nevertheless, the fear that a permanent visual defect would emerge in 34 patients who did not have visual difficulties caused them to undergo subtemporal decompression. In patients without a major alteration in the visual function, where the efficacy of both therapeutic forms was able to be evaluated, there wasn’t a significant difference in the “degree of healing” among the 31 patients surgically treated and the 43 patients treated with repeated lumbar punctures or simply managed with a close observation. Subtemporal decompression is not a totally innocuous procedure, which is proven with the onset of post-operative focal seizures in 5 patients and transitory otorrhoea in another.
The inadequacy of both supportive treatments is made clear in this series, in which 6 surgically treated patients and 6 treated with repeated lumbar punctures were readmitted between 2 weeks and 7 years after their hospital discharge due to the reappearance of intracranial hypertension signs and symptoms.
Nineteen patients who did not receive treatment were discharged after diagnostic studies and a short observation period. This substantiates in part the fact that often, BIH is a self-limited syndrome, and in absence of a specific etiology, there may not be the need for surgical decompression or repeated lumbar punctures. Certainly, in cases where papilledema and other intracranial hypertension signs and symptoms improve or are reduced after diagnostic tests, they may require just an observation period. Nevertheless, the progression of these findings in other patients may require a more vigorous treatment in the form of decompression or serial lumbar punctures. Although a frequent and repeated exam of the visual function may serve as a useful guide to assess the need for this form of treatment, a sudden decline in the visual function may be incorrigible by surgical decompression or lumbar punctures. The elevation of CSF pressure may also indicate the need for the institution of a more direct treatment. But an abnormal CSF pressure (above 200mm of H2O) may exist months after the patient leaves the hospital, when he/she is asymptomatic and the papilledema has disappeared. The nature of the phenomenon is unexplained (Tables 2–5).
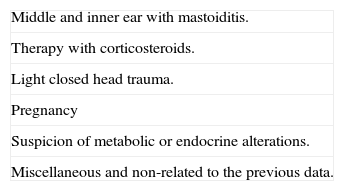
Findings in visual fields in 80 patients with benign intracranial hypertension.
| Visual fields | Etiology | ||||||
|---|---|---|---|---|---|---|---|
| Otic Infection | Cranial Trauma | Steroid Therapy | Pregnancy | Endocrine or Metabolic Alterations | Unknown | Total | |
| Normal | 0 | ||||||
| Augmented blind spot(Bilateral) | 7 | 4 | 2 | 8 | 34 | 20 | 75 |
| Reduction of visual fields(Bilateral) | 6 | 6 | |||||
| Scotoma (Unilateral) | 1 | 2 | 1 | 4 | |||
| Centrocecal scotoma (Unilateral) | 2 | 2 | |||||
| High altitude defect(Bilateral) | 1 | 2 | 3 | ||||
| Homonymous hemianopsia | 2 | 2 | |||||
| Bitemporal hemianopsia | 1 | 1 | |||||
| Temporal hemisnepsia (Unilateral) | 1 | 1 | |||||
| Cuadronopsia (Unilateral) | 1 | 1 | |||||
| Lower altitudinal blindness (Unilateral) | 1 | 1 | |||||
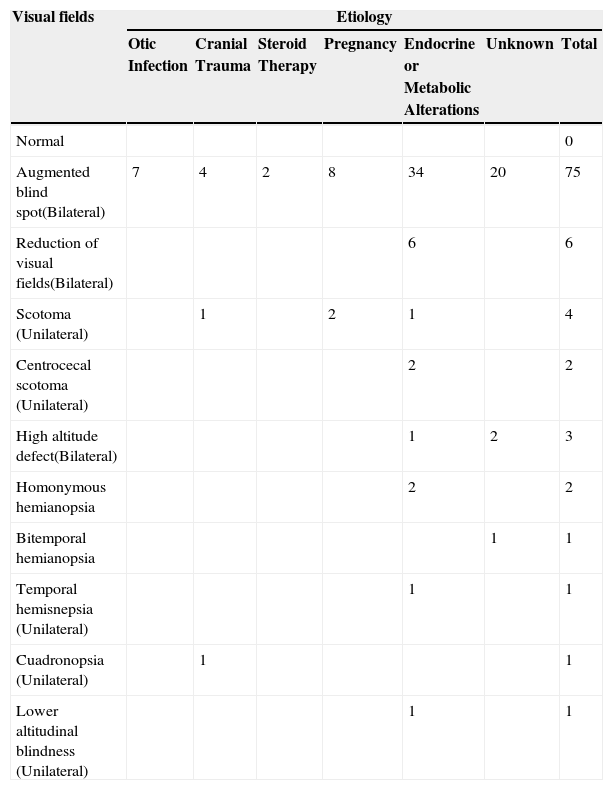
Corrected visual acuity in 80 patients with benign intracranial hypertension.
| Visual acuity | Etiology | ||||||
|---|---|---|---|---|---|---|---|
| Otitis | Cranial Trauma | Steroid Therapy | Pregnancy | Endocrine or Metabolic Alterations | Unrelated | Total | |
| Normal | 7 | 3 | 1 | 6 | 28 | 15 | 60 |
| Uniocular acuity less than 20/70 | 2 | 2 | 4 | ||||
| Binocular acuity less than 20/70 | 1 | 1 | 4 | 5 | 11 | ||
| “Finger-counting or light” Uniocular Vision | 1 | 1 | 2 | ||||
| “Finger-counting or light” Binocular Vision | 1 | 1 | 2 | ||||
| Uniocular blindness | 0 | ||||||
| Binocular blindness | 1 | 1 | |||||
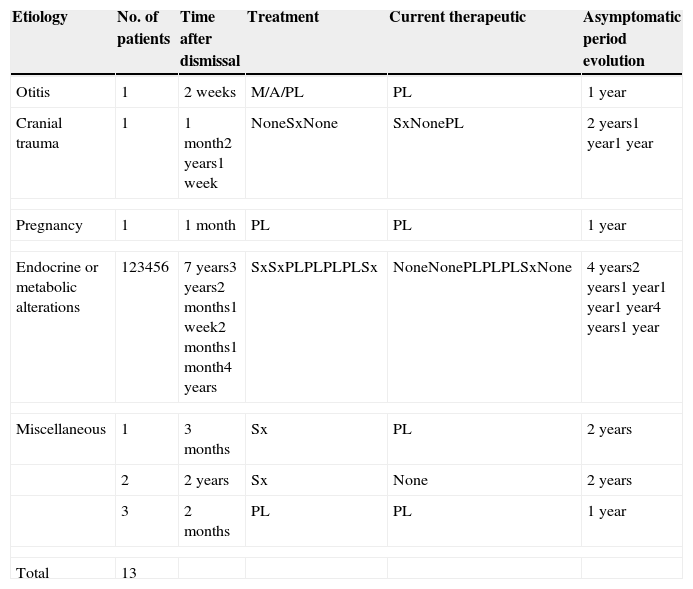
Evolution of 13 of 102 patients readmitted with benign intracranial hypertension.
| Etiology | No. of patients | Time after dismissal | Treatment | Current therapeutic | Asymptomatic period evolution |
|---|---|---|---|---|---|
| Otitis | 1 | 2 weeks | M/A/PL | PL | 1 year |
| Cranial trauma | 1 | 1 month2 years1 week | NoneSxNone | SxNonePL | 2 years1 year1 year |
| Pregnancy | 1 | 1 month | PL | PL | 1 year |
| Endocrine or metabolic alterations | 123456 | 7 years3 years2 months1 week2 months1 month4 years | SxSxPLPLPLPLSx | NoneNonePLPLPLSxNone | 4 years2 years1 year1 year1 year4 years1 year |
| Miscellaneous | 1 | 3 months | Sx | PL | 2 years |
| 2 | 2 years | Sx | None | 2 years | |
| 3 | 2 months | PL | PL | 1 year | |
| Total | 13 | ||||
Readmitted twice: M: Mastoidectomy; A: Antibiotics; Sx: Decompression; PL: Serial Lumbar Punctures.
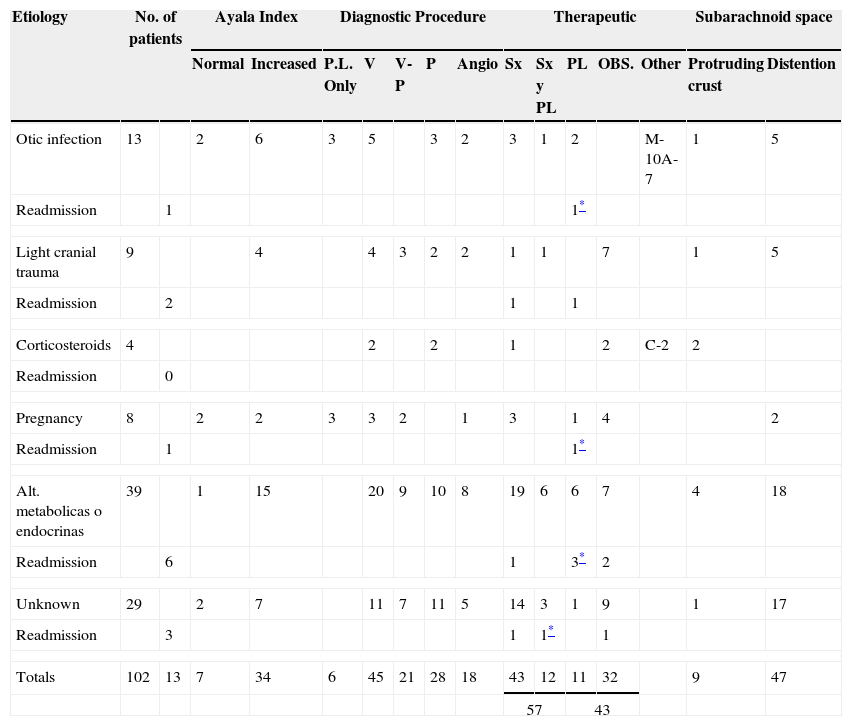
Diagnostic and therapeutic management of 102 patients with benign intracranial hypertension.
| Etiology | No. of patients | Ayala Index | Diagnostic Procedure | Therapeutic | Subarachnoid space | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Normal | Increased | P.L. Only | V | V-P | P | Angio | Sx | Sx y PL | PL | OBS. | Other | Protruding crust | Distention | |||
| Otic infection | 13 | 2 | 6 | 3 | 5 | 3 | 2 | 3 | 1 | 2 | M-10A-7 | 1 | 5 | |||
| Readmission | 1 | 1* | ||||||||||||||
| Light cranial trauma | 9 | 4 | 4 | 3 | 2 | 2 | 1 | 1 | 7 | 1 | 5 | |||||
| Readmission | 2 | 1 | 1 | |||||||||||||
| Corticosteroids | 4 | 2 | 2 | 1 | 2 | C-2 | 2 | |||||||||
| Readmission | 0 | |||||||||||||||
| Pregnancy | 8 | 2 | 2 | 3 | 3 | 2 | 1 | 3 | 1 | 4 | 2 | |||||
| Readmission | 1 | 1* | ||||||||||||||
| Alt. metabolicas o endocrinas | 39 | 1 | 15 | 20 | 9 | 10 | 8 | 19 | 6 | 6 | 7 | 4 | 18 | |||
| Readmission | 6 | 1 | 3* | 2 | ||||||||||||
| Unknown | 29 | 2 | 7 | 11 | 7 | 11 | 5 | 14 | 3 | 1 | 9 | 1 | 17 | |||
| Readmission | 3 | 1 | 1* | 1 | ||||||||||||
| Totals | 102 | 13 | 7 | 34 | 6 | 45 | 21 | 28 | 18 | 43 | 12 | 11 | 32 | 9 | 47 | |
| 57 | 43 | |||||||||||||||
V=Ventriculography; V-P=Ventriculography ineffective, Pneumoencephalography performed; P=Pneumoencephalography; ANG=Carotid angiography; Sx=Subtemporal or suboccipital decompression; Sx & PL=Serial lumbar punctures after decompression; PL=Serial lumbar punctures; M=Mastoidectomy; A=Antibiotics; C=Hydrocortisone; OBS=Clinical observation (including a reduced diet with 27 obese patients).
CORTEZA PROMINENTE = Brain protruded through incision in hard and aranoides.
Distention = The subarachnoid space appears distended.
The clinical course of 102 patients with benign intracranial hypertension has been revised. Under the bases of common events of the outbreak of physical findings, these patients may be distributed into 6 different categories: a) Otic infection (13), b) Light closed head trauma (9), c) Corticosteroids therapy (4), d) Pregnancy (8), e) Probable metabolic or endocrinal alterations (39), f) A miscellaneous group not related to the other groups (29). The etiological significance of each group is discussed.
With the exception of children with otic infection, where the cause of the syndrome seems to be the obstruction of the lateral venous sinus, the pathogenesis in the rest of the groups remains obscure. Both aspects, the exposed brain and the subarachnoid space during surgery, offer a clue towards the nature of the syndrome. During surgery, the bulging of the cerebral cortex was observed in 9 patients. This suggests cerebral edema, and the presence of normal or small ventricles would be compatible with this possibility. However, we were able to observe a distention of the subarachnoid space in 46 patients. This, in addition to the finding of a rise of persistent elevation of the Ayala index in 34 patients, would support the hypothesis of an increased CSF volume.
The specific treatment for this syndrome includes mastoidectomy and antibiotics in patients with ear infection and occlusion of the lateral venous sinus. Supportive therapy, in the form of a hypocaloric diet for the obese patient, hydrocortisone for the child admitted after having received corticosteroid therapy, subtemporal decompression and/or repeated lumbar punctures are the utilized methods. In general, all these forms of therapy have been found to be inadequate.
It is concluded that in many cases, BIH is a self-limited syndrome and, in absence of a specific etiology, the use of aggressive therapy may not be necessary. Therefore, the management of each patient in particular ought to be individualized.
This article is a reprint of the article “Benign Intracraneal Hypertension (Cerebral Pseudo-tumor)” published in MEDICINA UNIVERSITARIA, Vol. 1, No. 1, 1970 (Medicina Universitaria 1970;1(1):5-34) on the occasion of the 45th anniversary of the journal.
The Ayala Index is obtained by multiplying the final CSF pressure by the amount extracted, dividing the result by the initial pressure. Normal values range between 5.5 and 6.9, indexes below 5.5 are linked to a reduced CSF volume and those above 6.9 with an increase.3