Obesity is a condition in which there is an excessive accumulation of fat, and it is defined when the Body Mass Index (BMI) is greater or equal to 95 percent for subject's age and gender. Severe obesity is defined as the body mass index greater than 99 percent for the subject's age and gender; furthermore, overweight is defined as a body mass index greater or equal to 85 percent but lower than 95 for the subject's age and gender. Impaired fasting glycaemia is defined as central glycaemia equal or greater than 100mg/dL but lower than 125mg/dL in a fasting state of at least 12h. Carbohydrate intolerance is defined as central glycaemia equal or greater than 140mg/dL but lower than 200mg/dL in a sample taken 2h after a load of 75g (or 1.8g×kg) of anhydrous glucose.
Diabetes mellitus is defined as one of the following four criteria:
- 1.
Glycaemia greater than or equal to 125mg/dL in 2 determinations in a fasting state of at least 6h.
- 2.
Glycaemia greater or equal to 200mg/dL in 1 determination at any moment, along with hyperglycemia symptoms.
- 3.
Glycaemia greater or equal to 200mg/dL 2h after a 75-gram load (1.8 grams per kilogram) of anhydrous glucose.
- 4.
Glycosylated hemoglobin (HbA1c) greater than 6.5%
The HOMA Index is defined as the insulin resistance index, obtained from the multiplication of glucose×insulin/405 and used to determine insulin resistance. Insulin resistance is defined as a HOMA index greater than or equal to 2.5. Hypercholesterolemia is defined as total cholesterol greater than 200mg/dL or LDL greater than 130mg/dL after fasting for at least 12h. Hypertriglyceridemia is defined as triglycerides greater than 100mg/dL in children younger than 10 years, and less than 130mg/dL in children 10 to 19 years old after fasting for at least 12h. The typical combined dyslipidemia secondary to childhood obesity consists of elevated triglycerides with low HDL cholesterol and normal to slightly elevated levels of LDL cholesterol. Hepatic steatosis is defined as hypertransaminasemia corroborated by hepatic ultrasound. Abdominal circumference is the measurement around the waist taken at the midpoint between the anterosuperior iliac crest and the costal ridge.
The metabolic syndrome is defined as the patient presenting 3 of the following 5 criteria: (1) Central obesity, which refers to an abdominal circumference greater than the 90th percentile for their age. (2) Glucose greater than 100mg/dL. (3) Triglycerides greater than 150mg/dL. (4) HDL less than 45. (5) Blood pressure greater than the 90th percentile for their age and sex.
EpidemiologyObesity has tripled in the world over the past 30 years. In the United States, 16% of children and 17% of adolescents are classified as obese, and alarmingly, the levels of obesity in Hispanic children and adolescents are much higher. At present, 48.6 million Mexicans are obese. According to the National Health Survey (ENSANUT 2012), 9.7% of preschool children, 34.4% of schoolchildren and 35.8% of Mexican adolescents are overweight or obese, equivalent to 5.54 million children in our country. The incidence of obesity worldwide is higher in the major cities (24% versus 5% in rural areas), children of higher income parents (22% vs. 7%) and children of better educated parents (20%). Also with parents who finished university against 4% in children of parents who only finished primary school). This is important, since obesity patients in childhood and adolescence have a mortality rate up to 12 times higher between 20 and 30 years of age, and spend up to 34% of their family income on complications related to obesity.
EtiologyObesity is a condition of multifactorial origin. It has a strong genetic load since if one of the parents is obese, the children have a 33% to 64% risk of being obese compared to a child of parents with a normal body mass index. Humans have genes to keep fat and reduce energy consumption during prolonged periods of fasting, but it becomes obsolete in our society, where there is a constant abundance of food. In addition to the genetic factors, environmental factors are added, which correspond to an unhealthy lifestyle, which leads to an energy imbalance. This unhealthy lifestyle includes poor nutrition and poor physical activity.
The causes of poor nutrition are the low availability of healthy foods, poor preparation time, excess processed food and advertising. Causes of poor physical activity include unsupported urban development, lack of infrastructure, little free time to complete (full-time schools, parental work), and insecurity. Lifestyle changes such as overeating and non-exercise, formula feeding or mixed breastfeeding and early ablation have higher rates of obesity than breastfed infants and late ablation. Other harmful habits are fast foods, omission of breakfast, midnight snacks, video games, buying food at school and missing meals were noted as risk factors for the presentation of obesity in children. All these factors result in the accumulation of visceral fat, with consequent hyperinsulinemia and hypertension.
There are genetic syndromes that predispose one to obesity, such as Prader-Willi syndrome, hormonal and drug intake. However, these account for less than 5% of obese patients.
Risk factorsThere are risks for obesity which have to do with prenatal and perinatal metabolism programming. Patients at a higher risk of developing obesity in the schooling and adolescent stages are children born preterm, with low weight for their gestational age due to intrauterine growth retardation (IUGR), children of mothers with hypertension and preeclampsia. Also, children of mothers with malnutrition, since these patients are malnourished in utero and, as a consequence, they are born with a fat-producing, fat-burning metabolic program. Other patients with similar risks are the children of diabetic mothers and patients with a large weight for their gestational age (PGEG) as they undergo malnutrition in utero. These should be considered risk groups for obesity, and receive aggressive and timely preventive treatment.
The most important prevention of cardiovascular disease is to start treating overweight infants. Other patients at risk of obesity are patients who received less than 6 months of exclusive breastfeeding and patients who were fed whole milk and/or gluten before they were one year old.
Perinatal risk factors for the metabolic syndrome are as follows: (1) Prematurity. (2) Low weight for gestational age and/or intrauterine growth retardation. (3) Children of mothers with preeclampsia. (4) Sons of mothers with diabetes mellitus, pre-existing or gestational. (5) Macrosomic and/or large weight for gestational age. (6) Malnutrition or maternal malnutrition.
PhysiopathologyBody fat is accumulated by hyperplasia and hypertrophy of adipose cells. The first is found most commonly in preschool and school children, and the second in adolescents and adults.
HypertensionIt has been shown that in predisposed patients, the severity of arterial hypertension and resistance to medical treatment increase with the degree of obesity. The best treatment is weight loss and change of habits.
Diabetes mellitusDiabetes mellitus occurs more frequently in overweight patients, with clinical data of insulin resistance and a positive family history. The majority of cases are type 2 diabetes mellitus (75–85%). In children, this disease progresses from relative deficiency to absolute insulin resistance, and then to chronic complications much faster than in adult patients. Good glycemic control is very difficult if weight is not controlled.
HyperuricemiaTwenty percent of pediatric patients with obesity present hyperglycemia and clinical data on gout.
Fatty liver or hepatic steatosisThis makes up 20–25% of overweight and obese patients. It presents a histology similar to that of non-alcoholic fatty liver and, in case of not controlling the weight, progresses rapidly to non-alcoholic hepatitis and liver failure.
Acanthosis nigricansAcanthosis nigricans is produced by an overestimation of melanocytes, and is the clinical characteristic of insulin resistance. Its severity does not always correlate with the degree of resistance.
Musculoskeletal and otherOther disorders associated with obesity include leg pain, joint pain, stretch marks, reprimands, precocious puberty, and gastroesophageal reflux disease.
PsychologicalA little addressed branch is the psychological symptoms. Most obese patients have symptoms of anxiety, leading to a vicious circle that leads to being overweight. Some psychosomatic symptoms presented by patients with obesity are nervous coughs, frequent urination, irritable bowel, trichophagia and nervous vomiting. Depression, bullying, low self-esteem and social isolation also occur in these patients. 42% of children with obesity suffer from depression, and 40% have anxiety, according to DSM-IV criteria, in addition to a direct correlation between BMI and low self-esteem.
Treatment and conclusionsThe main treatment for children is diet and exercise, that is, changing the risk environment, and it must be a priority. Lifestyle should be improved before treatment. Frequent measurements are beneficial for patients and their parents to be aware of the level of adiposity of their children, so they follow the treatment. The percentage of body fat per impedance measurement is acceptable and almost equivalent to tomography measurements. Childhood obesity appears with a powerful array of cardiovascular risk factors, including combined dyslipidemia, insulin resistance, hypertension, and accelerated atherosclerosis has been demonstrated in this age group. It is clear that atherosclerosis begins from childhood and, according to some researchers, from the prenatal stage.
The diseases manifested by obesity are rare in infancy, but risky habits for atherosclerosis and other diseases related to obesity begin from childhood, and treatment of them can delay the progression of the disease.
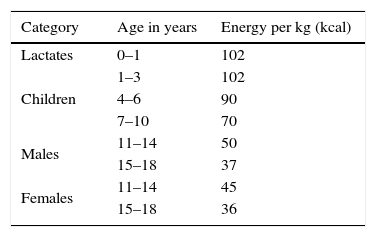
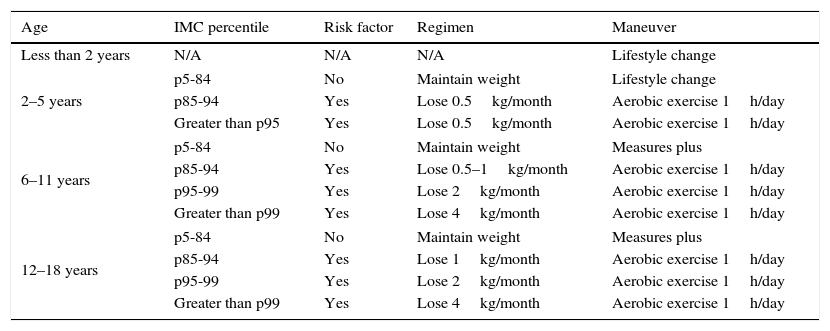
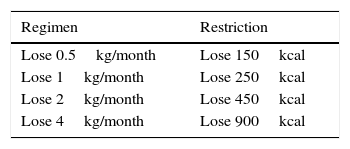
The nutritional regimen for childhood obesity should be managed by a competent nutritionist according to the daily requirements by age and Tanner stage. Table 1 shows the daily nutrition requirements according to age. Tables 2 and 3 may be helpful to establish an individualized nutritional regiment.
Nutritional treatment by BMI and age.
| Age | IMC percentile | Risk factor | Regimen | Maneuver |
|---|---|---|---|---|
| Less than 2 years | N/A | N/A | N/A | Lifestyle change |
| 2–5 years | p5-84 | No | Maintain weight | Lifestyle change |
| p85-94 | Yes | Lose 0.5kg/month | Aerobic exercise 1h/day | |
| Greater than p95 | Yes | Lose 0.5kg/month | Aerobic exercise 1h/day | |
| 6–11 years | p5-84 | No | Maintain weight | Measures plus |
| p85-94 | Yes | Lose 0.5–1kg/month | Aerobic exercise 1h/day | |
| p95-99 | Yes | Lose 2kg/month | Aerobic exercise 1h/day | |
| Greater than p99 | Yes | Lose 4kg/month | Aerobic exercise 1h/day | |
| 12–18 years | p5-84 | No | Maintain weight | Measures plus |
| p85-94 | Yes | Lose 1kg/month | Aerobic exercise 1h/day | |
| p95-99 | Yes | Lose 2kg/month | Aerobic exercise 1h/day | |
| Greater than p99 | Yes | Lose 4kg/month | Aerobic exercise 1h/day | |
The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNo financial support was provided.