Introduction
The therapeutic options for patients with multivessel coronary artery disease, consist of pharmacological treatment, percutaneous coronary intervention and coronary artery bypass graft surgery.1 The pharmacological treatment must be used in all cases, either as the only treatment or before and after the percutaneous intervention or coronary bypass surgery.2 Percutaneous intervention with the use of stents is preferred when there is severe disease of only one vessel that does not involve the proximal left anterior descending artery (LAD) or the left coronary artery.2 Recently developed drug-eluting stents were expected to decrease some of the limitations of percutaneous coronary intervention using metallic stents; however, recent publications question the clinical and cost-benefit outcomes of medicated stents in coronary artery disease.3,4
This has renewed interest in the medium- and long-term outcomes of coronary bypass surgery. Coronary bypass surgery is indicated in patients with significant stenosis of the left coronary artery, stenosis of 70% of the proximal LAD and of the circumflex artery and in patients with three or more diseased vessels.1,2,5 The ultimate goal of this surgery is to achieve complete revascularization with conduits that remain permeable for the remainder of the patient's life.1
Some of the conduits used in this type of surgery are the great saphenous vein, the internal thoracic artery, the radial artery5 and the ulnar artery.6 For a vascular conduit to be selected as a coronary revascularization graft, it must exhibit the following characteristics: sufficient length, lumen diameter and thickness of the vessel wall. It must also have minimal in situ ischemic consequences and an acceptable permeability over time of the conduit.6
Internal Thoracic Artery (ITA)
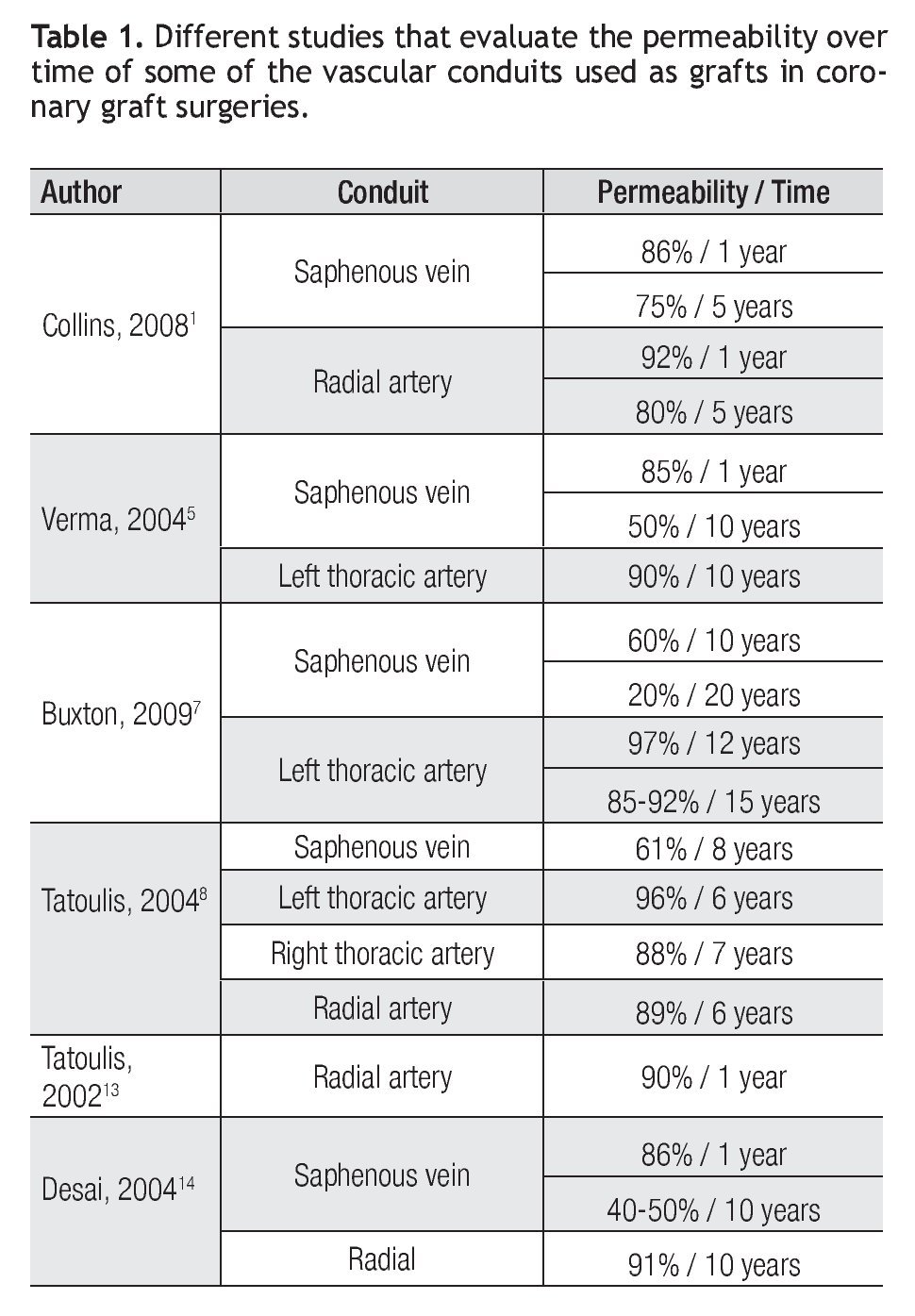
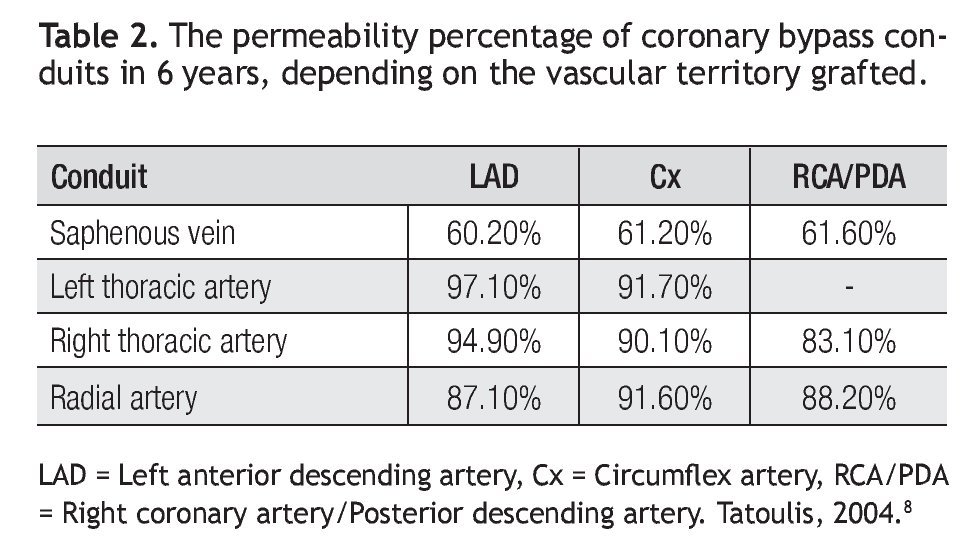
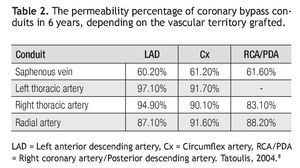
In 1980, the long-term survival benefit was demonstrated convincingly with a pedicle graft from the left internal thoracic artery (ITA) to the LAD. This benefit results from increased graft permeability over time compared with the GSV graft.9 The permeability over time for the left ITA graft is 96.4% and for the right ITA is 88.3% (Table 1).7 The coronary territory that is grafted via this conduit modifies its permeability over time, making it 99%, 97% and 93% at five, 10 and 15 years, respectively, for the left ITA to the LAD8 and 97%, 92% and 89% at five, eight and 10 years, respectively, for the circumflex artery.8 For a graft from the right ITA to the LAD, the life expectancy is 95%; to the circumflex artery, it is 90%; and to the right coronary/posterior descending artery, it is 83% (Table 2).8
Since then, coronary bypass surgery using the ITA as a pedicle graft on the LAD has been considered the standard;9 the ITA is recognized by cardiothoracic surgeons and cardiologists as the most effective and reliable coronary revascularization conduit.10
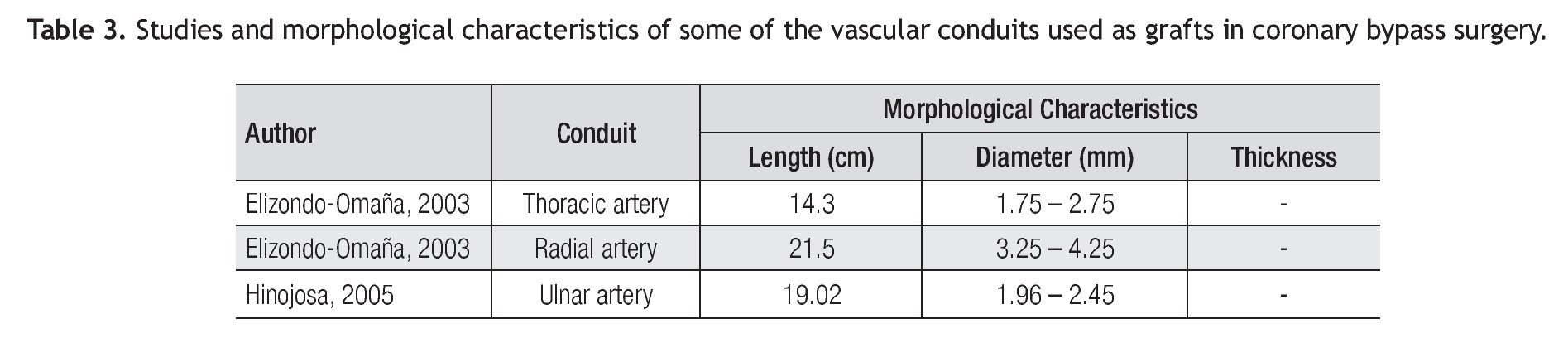
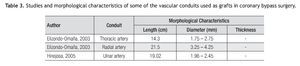
The ITA is a conduit that has a length of 14.3 cm and a diameter that varies from 1.75 mm to 2.75 mm (Table 3).11 The thickness of the arterial wall has not been studied morphologically. The clinical consequences of its extraction are minimal, except when there is a bilateral use of these arteries.2,13
Bilateral use of the Internal Thoracic Artery
The benefits of using a second ITA are not clear, despite the amount of literature on the subject.7 After an adjustment for risks, it was concluded that there is a benefit to the survival and less chance of re-intervention with the use of both internal thoracic arteries.7 However, the long duration of the operation is of concern, as well as the increased risks of morbidity in patients who are elderly, obese, diabetic or who have chronic respiratory disease. These patients have an increased risk of sternal wound infection, which represents a relative contraindication to the bilateral use of the ITAs.12,13 Furthermore, the right ITA occasionally does not reach the territories of the circumflex and posterior descending arteries.13
Great Saphenous Vein (GSV)
In 1968, Favaloro reported the first successful coronary artery bypass surgery using the saphenous vein as a graft.5 The high incidence of failure of saphenous vein grafts has led to an extensive use of arterial conduits.7,8 The overall permeability over time is 61% between five and 10 years (Table 1), and is not affected by the vascular territory grafted (Table 2).8
Radial Artery (RA)
In 1992, Acar and colleagues revived the use of the radial artery (RA) as a graft conduit for myocardial revascularization by publishing a study of 104 patients who had received a radial artery graft since 1989.5,7,13 The study showed that the RA represents a reasonable alternative to other conduits that complement the left ITA.5 The radial artery has been rapidly gaining popularity because of its diameter, length, safety and ease of extraction, in addition to presenting good results in the medium- and long-term.12 Currently, it is considered the second-choice conduit, following the left ITA and coming before the right ITA.8,12
The permeability over time in the medium- and long-term for the RA as a graft conduit for myocardial revascularization varies from 87.5% to 96.5%10 (Table 1), and seems not to be affected by the vascular territory grafted. The permeability over time for the LAD is 87% (significantly lower than the ITA); for the circumflex, 92% (similar to ITA); and for the right coronary/posterior descending artery, 88%, longer than for the right ITA (Table 2).8 All have been shown to be superior to the GSV.1,5,7-9,13,14 The RA is commonly anastomosed to the circumflex artery, the right coronary artery or the posterior descending artery;7,8,12,13 the Roux-en-Y anastomosis is recommended (from an ITA graft to the coronary) on the aorto-coronary anastomosis, with the goal of avoiding manipulation of the aorta during surgery with the heart beating,7,12 in addition to enabling greater conduit length.12 Some of the advantages that the RA graft offers are an adequate length to anastomose, including distal portions of obtuse marginal arteries; its lumen is comparable to those of coronary arteries; its thicker wall enables anastomosis, both proximal and distal, which is less demanding for the surgeon.5,13,15 In addition, the vasa vasorum of the RA do not penetrate the tunica media, so it is assumed that they are not necessary for arterial nourishment, making the RA an ideal conduit to use as a free graft.15 Compared to the right ITA, the RA is larger and easier to manipulate; easier to prepare; can be extracted at the same time as the left ITA, which reduces surgery time; is better able to revascularize more remote branches than the pedicle of the right ITA; and avoids the risk of sternal infections caused by bilateral dissections of the ITAs.5,9 The RA has proved to be an extremely versatile conduit and its use has been associated with extremely satisfactory clinical and angiographic results.13
The disadvantages of using the RA include the contraindications, which are poor collateral circulation, atheromatous plaques, damage by trauma or canalization, arteriovenous fistula for hemodialysis, vasculitis and Raynaud's syndrome.5 There is also a risk of sensory and motor dysfunction in the hand.5,13,16-20 The biggest disadvantage, which affects long-term performance, is the propensity for the RA to suffer spasms5,13-15 resulting from decreased or challenged blood flow.14,15 This is due to the great thickness of the arterial wall and the density and organization of myocytes in the tunica media.8,12,14,15
The use of the RA is based on the assumption that there is adequate collateral blood flow to the hand by the ulnar artery.21 The reason for this is a conviction based on classical anatomy that indicates that the ulnar artery is the dominant artery of the forearm and sacrificing the RA is safe.21,22
The RA is a conduit 21.5 cm in length, with an average proximal diameter of 4.25 mm and a distal diameter of 3.25 mm.11 The thickness of the arterial wall has not been determined (Table 3). The clinical consequences of extraction of this conduit are rare and include paresthesia and general weakness of the hand, in addition to a reported case of acute ischemia of the hand.5,13,16-20
Ulnar Artery (UA)
In 1998, Buxton documented reports in the literature of use of the ulnar artery (UA) as a myocardial revascularization conduit,21 and it has been used by other surgeons.23 The use of the UA in this procedure is possible, albeit not very popular, even when there has been low morbidity reported at the donor site.6,22 No evidence of myocardial ischemia that would suggest graft failure in coronary arteries has been reported.21
The UA originates from the bifurcation of the brachial artery in the elbow crease, where it is considered dominant; however, it issues ulnar recurrent branches and the common interosseous artery (CIA), distal to where the UA reduces its caliber.6,21,22,24 It has been reported that the RA is the main artery in the irrigation of the hand.6,23,24 This distal zone at the origin of the CIA and proximal to the wrist is selected, thus conserving the collateral circulation to the hand via the CIA by its anastomosis with carpal and palmer arches.6,21
The major concerns with the use of the UA for surgeons are its proximity to the ulnar nerve and the fact that they are incorporated in the same sheath; nevertheless, no evidence has been reported of neurological dysfunction resulting from the manipulation of the ulnar nerve or the section of the vasa nervorum from the UA.21 Until now, no anatomical or hemodynamic reasons have been found to prefer the use of the RA over the UA.6,22
The UA is a conduit 19.01 cm in length, with a proximal diameter of 2.45 mm and a distal diameter of 1.96 mm.6 The thickness of the UA wall has not been studied (Table 3). There have been no reports of clinical consequences at the extraction site with the use of this artery; nevertheless, there are fears of ulnar nerve damage.6,21
The Importance of Morphological Studies
Documenting the anatomical characteristics of the blood vessels used as graft conduits in coronary bypass surgery for myocardial revascularization can contribute to advances in surgical techniques6,21,25 and the selection of the best conduit.6,11
In our Department of Human Anatomy, several morphological studies that concern the myocardial revascularization conduits have been done.6,11,25 In a comparative study between ITA and RA morphology, the length of the vessels were found to be 14.3 cm and 21.5 cm, respectively,11 clearly showing the convenience of the RA in the revascularization of the more distal arteries, especially when used as a composite graft to be anastomosed with the left ITA.5,7,12,13,15 The average diameters of the proximal ends of the arteries were 2.75 mm and 4.25 mm, respectively, and those of the distal ends were 1.75 mm and 3.25 mm,11 showing that the RA has almost twice the diameter of the ITA.
In a morphological study to characterize the UA, its diameter was found to be 2.45 mm in the region distal to the origin of the CIA and 1.96 mm at the level of the wrist.6 The diameter at the level of the wrist is similar to what was found in the morphological study of palmar arches, which is 1.87 mm.25 Comparing these diameters with those found for the RA by Elizondo-Omaña (proximal: 4.25 mm, distal: 3.25 mm), it was observed that both RA diameters are greater than those from the UA, including at the level of the wrist,6,10 supporting the theory that the RA is the main artery that irrigates the hand.6,22,24 However, there are no studies that morphologically compare these two arteries in the same corpse.
It is important to note that the vascular conduits most used as grafts in coronary bypass surgery have morphological characteristics that make them different from the coronary arteries.
The Importance of Imaging Studies
Because of the existence of variations in the forearm arteries and in the anastomotic arches of both arteries at the level of the hand,6,21,25 it is mandatory to prove that the hand circulation is adequate before removing any of the arteries of the forearm. The Allen test is the most often used to prove this.6,12,25,26 However, a preoperative Allen test may result in a false negative.12,26 Other tests that are used to make the evaluation more objective are angiography, the Allen test modified by pulse oximetry,26 plethysmography with five channels, color Doppler ultrasonography22,26 and monitoring the changes in flow velocity in the ulnar artery.27
Angiography is the gold standard to demonstrate arterial permeability; however, it is only indicated in special cases because it is invasive, costly and has a risk of causing anaphylaxis. The Allen test modified by pulse oximetry makes the evaluation of collateral circulation more objective.26 With Doppler echocardiography, it is possible to measure the diameter of each artery as well as its flow by diameter and flow velocity by diameter;22,26 nevertheless, the limiting factor is that normal and abnormal parameters have not been determined for Doppler ultra-sonography.26
There is a controversy over the hemodynamic dominance of the hand arteries, because there are studies that support the ulnar artery as the dominant artery,26 while others say the radial artery is dominant.22
Currently in our department, comparative morphological studies between the coronary arteries and the conduits most frequently used in coronary bypass surgery are being developed. In addition, research on the adaptive changes and the remodeling that vascular conduits experience when exposed to a different environment than where they originated are being conducted.
In order to choose the most appropriate vascular conduit for coronary bypass surgery, it is necessary to perform comparative studies of the morphological and imaging characteristics of these conduits in the near future.
Corresponding autor: José Miguel Hinojosa-Amaya. Avenida Madero y Dr. Aguirre Pequeño s/n Col. Mitla Centro CP 64460. Phone: (81) 8329 4171. Department of Human Anatomy, UANL School of Medicine, Monterrey, Nuevo León, México.
E mail:rod_omana@yahoo.com
Received: November 2009.
Accepted: February 2010