Objetivo: Determinar la discrepancia existente entre los diagnósticos clínicos emitidos como causa de muerte, y los diagnósticos finales de las autopsias, en el Servicio de Anatomía Patológica y Citopatología de nuestro hospital, asimismo comparar los hallazgos, con lo reportado en la literatura. Los objetivos secundarios consisten en identificar los diagnósticos discordantes más frecuentes, y determinar si influye el tiempo de internamiento.
Material y métodos: Se revisaron expedientes clínicos y protocolos, de las autopsias realizadas del 2004 al 2010. Fueron clasificados de acuerdo a diagnósticos clínicos y causa de muerte, se compararon con los diagnósticos de autopsia y se identificaron las discrepancias, clasificándolas en discrepancia mayor y menor. Además, se determinó la relación con el tiempo de estancia hospitalaria.
Resultados: En un periodo de siete años (2004-2010), se realizaron 428 autopsias, lo que corresponde al 6.8% de los pacientes fallecidos intrahospitalariamente. Noventa y siete casos fueron excluidos del estudio, debido a la autolisis masiva o a la ausencia de información clínica en el expediente, quedando un total de 331 autopsias. Se encontró discrepancia diagnóstica, en el 41.4% de los casos. En un 26% de la totalidad de los casos, se identificaron discrepancias mayores y en un 15.4% discrepancias menores. Los diagnósticos discrepantes más frecuentes fueron: neumonía, seguida de sepsis y hemorragia pulmonar masiva asociado a prematurez.
Conclusiones: Los resultados de este estudio demuestran la necesidad de la autopsia, para identificar con certeza las patologías del paciente, ya que en un alto porcentaje, los diagnósticos clínicos son erróneos o incompletos, estos hallazgos concuerdan con lo reportado en la literatura.
Objective: To determine discrepancies between clinical diagnoses established as cause of death and final autopsy diagnoses made at the Anatomic Pathology and Cytopathology Service of our hospital and compare the findings with those reported in the literature. The secondary objectives of the study are to identify the most frequent discordant diagnoses overall and to determine whether length of hospitalization plays a role.
Material and methods: The medical records and protocols of the autopsies conducted from 2004 to 2010 were reviewed and classified according to clinical diagnoses and causes of death. They were compared with autopsy diagnoses and discrepancies were identified and classified as major and minor discrepancies. The relationship with length of hospitalization was also determined.
Results: Four hundred and twenty eight autopsies were carried out over a seven years period (2004-2010), which corresponds to 6.8% of the patients who died in the hospital. Ninety seven cases were excluded from the study because of massive autolysis or the absence of clinical information in the records. A total of 331 remaining autopsies were included.
Diagnostic discrepancies were found in 41.4% of cases. Major discrepancies were identified in 26% of the total number of cases and minor discrepancies were identified in 15.4% of the total number of cases. The most common divergent diagnoses were pneumonia, followed by sepsis and massive pulmonary hemorrhage associated with prematurity.
Conclusions: The results of this study show that autopsies are necessary to identify patient pathologies accurately since a high percentage of clinical diagnoses are wrong or incomplete. These findings agree with the reports in the literature.
Introduction
Since time immemorial, autopsies have constituted a fundamental element of hospital practice and now, in the 21st century, in the era of molecular biology and genomic medicine, they continue to be a source of answers to unsolved clinical enigmas.1,2 The main objectives of an autopsy are to identify the pathological conditions that caused death, to analyze the pathophysiological interaction that influenced the disease and to establish the final clinical-pathological correlation. It is therefore considered to be a world-wide indicator of the quality of the medicine practiced at a hospital.3-6 There are various studies in the medical literature which show an important discordance rate between final clinical diagnoses and anatomopathological autopsy diagnoses.7-9 In a study published by Goldman and which is used as a world-wide reference, discrepancies between clinical diagnoses and autopsy diagnoses were classified as major and minor, according to their level of impact on therapeutic management and patient evolution. Major discrepancies are those in which a different diagnosis would have brought about a change in treatment with a probable impact on clinical evolution and survival. Minor discrepancies are those in which the difference in diagnoses is not directly related to the cause of death and its treatment would not have altered the patient's clinical evolution.10
Similar reports have shown that the frequency of diagnostic errors has not decreased significantly over time but remained at approximately the same percentage.11,12 Some studies have found that the diagnoses recorded on death certificates are incorrect in up to one third of cases and the final diagnosis reached after the autopsy as the cause of death was clinically unsuspected in up to 50% of cases.13,14
Objective
The main purpose of this study is to review the diagnoses obtained in the postmortem anatomopathological examination and compare them with the clinical diagnoses in order to find out if there are discrepancies and establish whether they are major or minor, as well as to compare our findings with the reports in the literature. Our secondary objectives are to identify the most frequent discordant diagnoses overall and to determine whether length of hospitalization plays a role according to the type of discrepancy. Additionally, we aim to identify the most frequent pathologies of patients treated at the "Dr. Jose Eleuterio González" University Hospital of the UANL and who underwent an autopsy.
Material and methods
The medical records and protocols of the autopsies conducted at the Anatomic Pathology and Cytopathology Service of the "Dr. Jose Eleuterio González" University Hospital from January 2004 to September 2010 were reviewed and classified according to main clinical diagnoses, causes of death, age and sex of patients. Final clinical diagnoses were compared with autopsy diagnoses and we determined the type of discrepancy, classifying discrepancies as major, when a different diagnosis would have prompted a change in treatment with a probable impact on clinical evolution and survival and minor, when the difference in diagnoses is not directly related to the cause of death.
Additionally, we determined the relation existing between the percentage of cases with diagnostic discrepancies and the length of hospitalization (less and more than 24 hours).
Autopsies whose anatomopathological diagnosis was massive autolysis were excluded from this study. There were 62 of these cases (all of them fetal deaths).
In order to ensure diagnostic correlation, the medical records were reviewed for all cases where the clinical information provided in the autopsy protocol was insufficient or when the clinical diagnoses included in the protocol did not match the anatomopathological diagnoses. In 35 cases not enough information was found in the medical records to carry out a diagnostic correlation analysis.
Results
The University Hospital of the UANL is a tertiary level hospital, which has 500 permanent beds. Over the last seven years, an average of 898 hospitalized patients have died per year. The first autopsy conducted and recorded at our hospital took place in 1954. From then and until September 2010, a total 4 863 autopsies were performed. At our institution, an autopsy is performed at the request of the treating physician after obtaining consent in writing from the patient's family.
Over a seven years period, 6 289 hospitalized patients died and 428 autopsies were carried out at the Anatomic Pathology and Cytopathology Service, which corresponds to 6.8% of all deceased patients. Out of the total 428 autopsies, 190 (44.4%) were performed on adult patients and 238 (55.6%) on pediatric patients (under 18 years of age). From the latter group, 62 autopsies performed on stillborns were excluded because tissues showed massive autolysis and the advanced state of tissue necrosis made it impossible to give an appropriate anatomopathological diagnosis. A total 366 autopsies were analyzed for this study, 189 of them (51.6%) were of females and 177 of them (48.4%) were of males. One hundred ninety autopsies (51.9%) were performed on adult patients and 176 (48.1%) were performed on pediatric patients.
Despite the fact that the medical record of each case was reviewed in detail, not enough information was found to carry out a diagnostic correlation in 35 (9.6%) of the total 366 autopsies analyzed. Therefore, the universe of analyzed autopsies for this purpose was reduced to 331 cases.
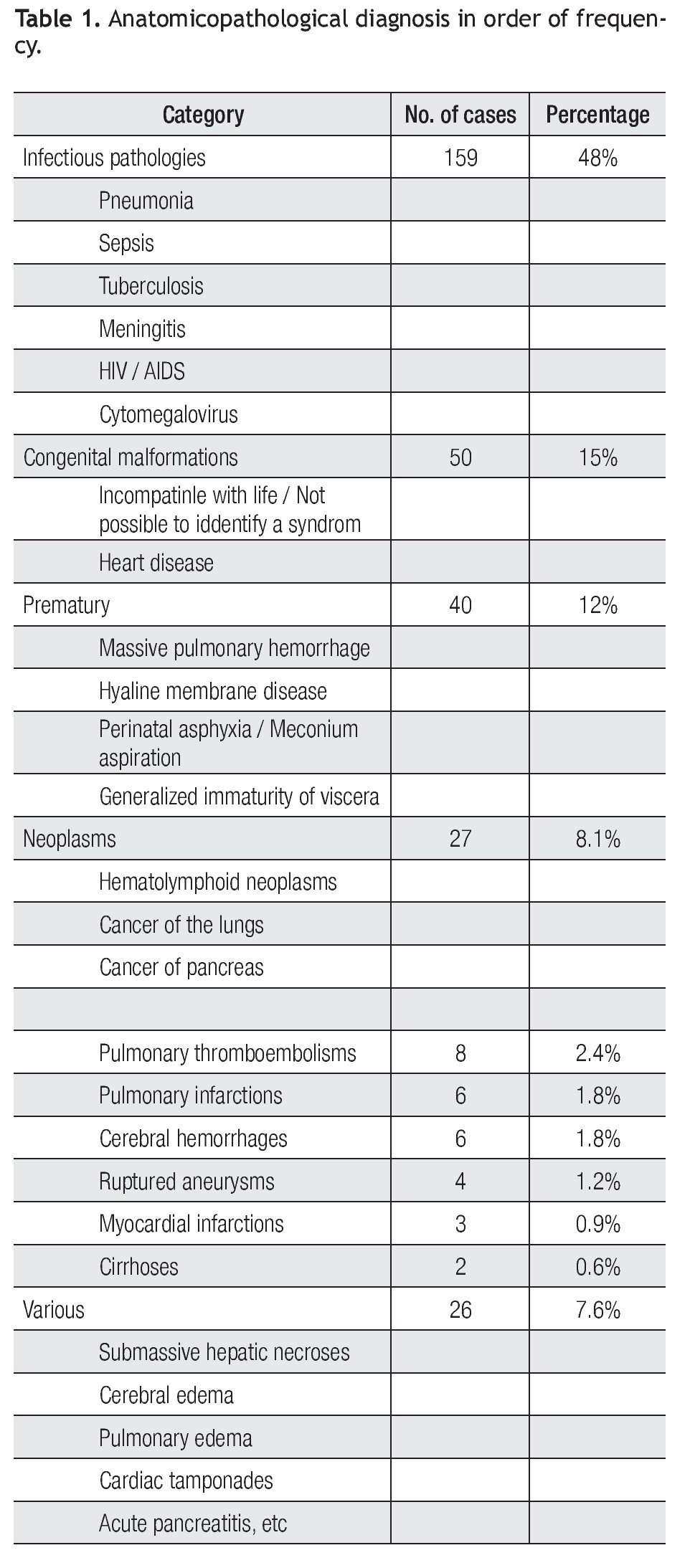
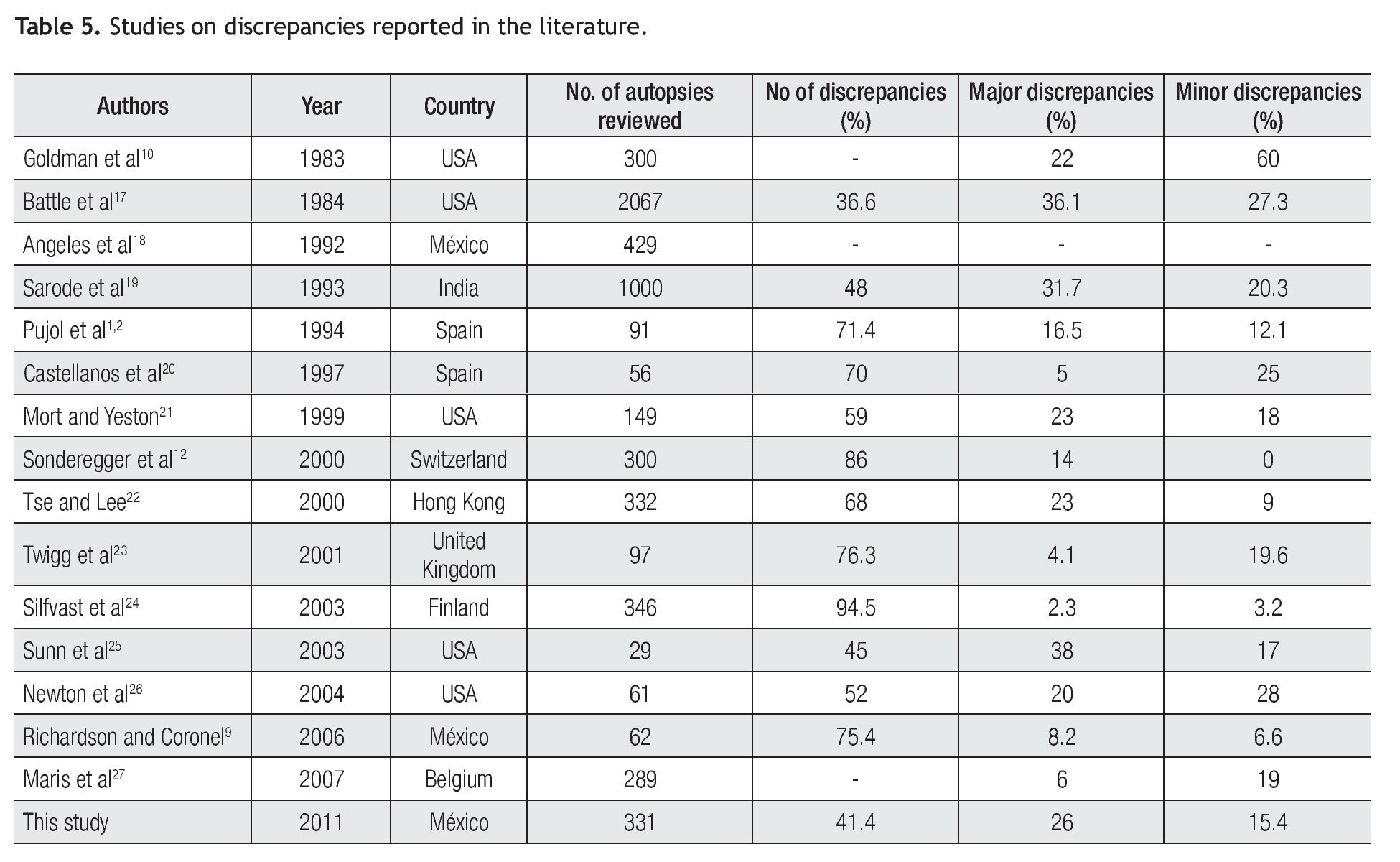
The most frequent anatomopathological diagnoses among the 331 cases corresponded to infectious pathologies (159 cases / 48%) with pneumonia taking first place, followed by sepsis and then by a lower number of cases of tuberculosis, meningitis, and Human Immunodeficiency Virus/ Acquired immune deficiency syndrome (HIV/ AIDS). In 50 cases (15%) the diagnoses corresponded to multiple congenital malformations, 38% of which were congenital heart diseases. In 40 cases (12%), disorders related to prematurity were diagnosed. The most frequent of these diagnoses was massive pulmonary hemorrhage, followed by hyaline membrane disease and perinatal asphyxia. Neoplastic pathologies were diagnosed in 27 cases (8.1%), 25 of which were malignant neoplasms and two of which were benign neoplasms. Hematolymphoid neoplasms were the most frequent, followed by pancreatic neoplasms. Less frequent cases were pulmonary thromboembolisms (eight cases / 2.4%), pulmonary infarctions and cerebral hemorrhages (six cases each / 1.8%), ruptured aneurysms (four cases / 1.2%), acute myocardial infarctions (three cases / 0.9%), and cirrhosis (two cases / 0.6%).
The rest of the pathologies found were not classified into a specific category because individually they did not represent a significant number. Nevertheless, altogether they accounted for 7.9% of cases, with a total of 26. Among these diverse pathologies we find, in order of frequency, cases of submassive hepatic necrosis, cerebral edemas, cardiac tamponades, and acute pancreatitis (Table 1).
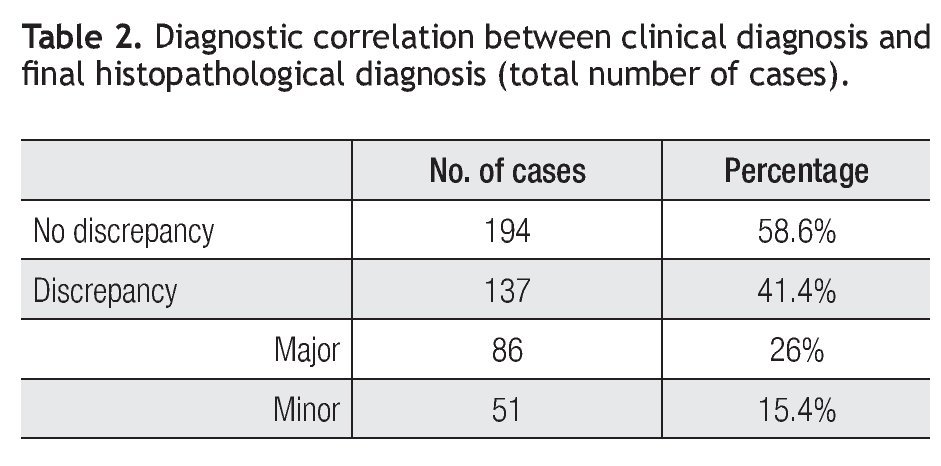
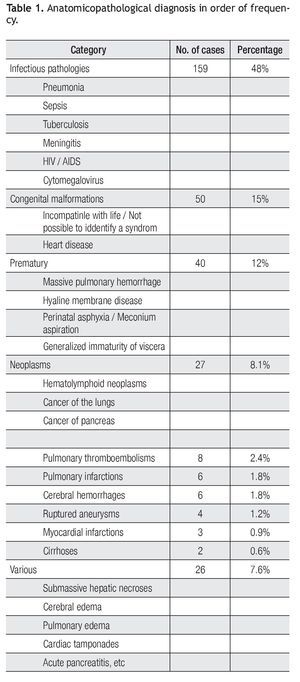
A correlation between the clinical diagnoses and the anatomopathological diagnoses was found in 194 cases (58.6%). In 137 cases (41.4%), there was a discrepancy between both diagnoses.
Out of the 137 cases in which there were discrepancies between the clinical diagnoses and the final autopsy diagnoses, in 86 cases (62.8%) the diagnostic differences corresponded to major discrepancies and in 51 cases (37.2%) they corresponded to minor discrepancies (Table 2). For the total number of autopsies reviewed (n=331), this represents a 26% of major discrepancies and a 15.4% of minor discrepancies.
In the cases where there were discrepancies, the main clinically unsuspected diagnoses were: pneumonia, 38 cases (27.7%), followed by sepsis and massive pulmonary hemorrhage, both with 12 cases (8.7%), pulmonary thromboembolisms and congenital malformations, both with five cases (3.6%). There were four cases of perinatal asphyxia / meconium aspiration, pulmonary infarction, and (2.9%).
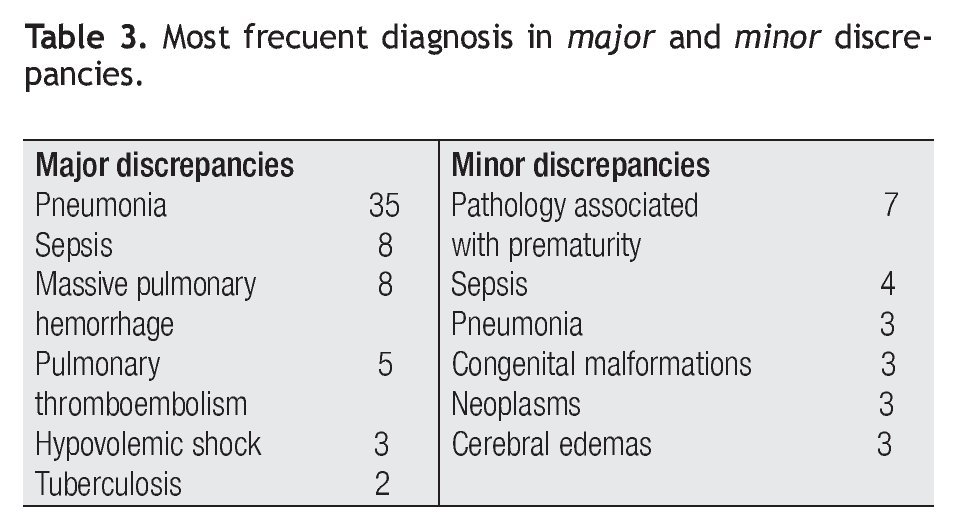
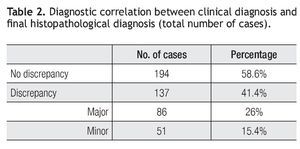
In regards to major discrepancies (62.8%), pneumonia takes first place (35 cases / 40.7%), followed by sepsis (eight cases / 9.3%), massive pulmonary hemorrhage associated with prematurity and pulmonary thromboembolisms (five cases / 5.8%), hypovolemic shock secondary to intra-abdominal hemorrhage, post-transplantation, or due to chronic gastric ulcers (three cases / 3.5%).
Among minor discrepancies (37.2%), the most frequent was the pathology associated with prematurity (seven cases / 13.7%), followed by sepsis (four cases / 7.8%), and pneumonia, congenital malformations, metastatic neoplasms, and cerebral edema, each with the same number of cases (three cases / 5.9%). Upon analyzing the hospitalization length in discordant cases, we found that in the majority of major discrepancies (65%), the patients had been hospitalized for more than 24 hours, whereas in the remaining number of major discrepancies (35%), the patients had been hospitalized for 24 hours or less (Table 3).
According to age group, we found that discrepancies were more frequent among adults (59%) and less frequent among pediatric patients (41%).
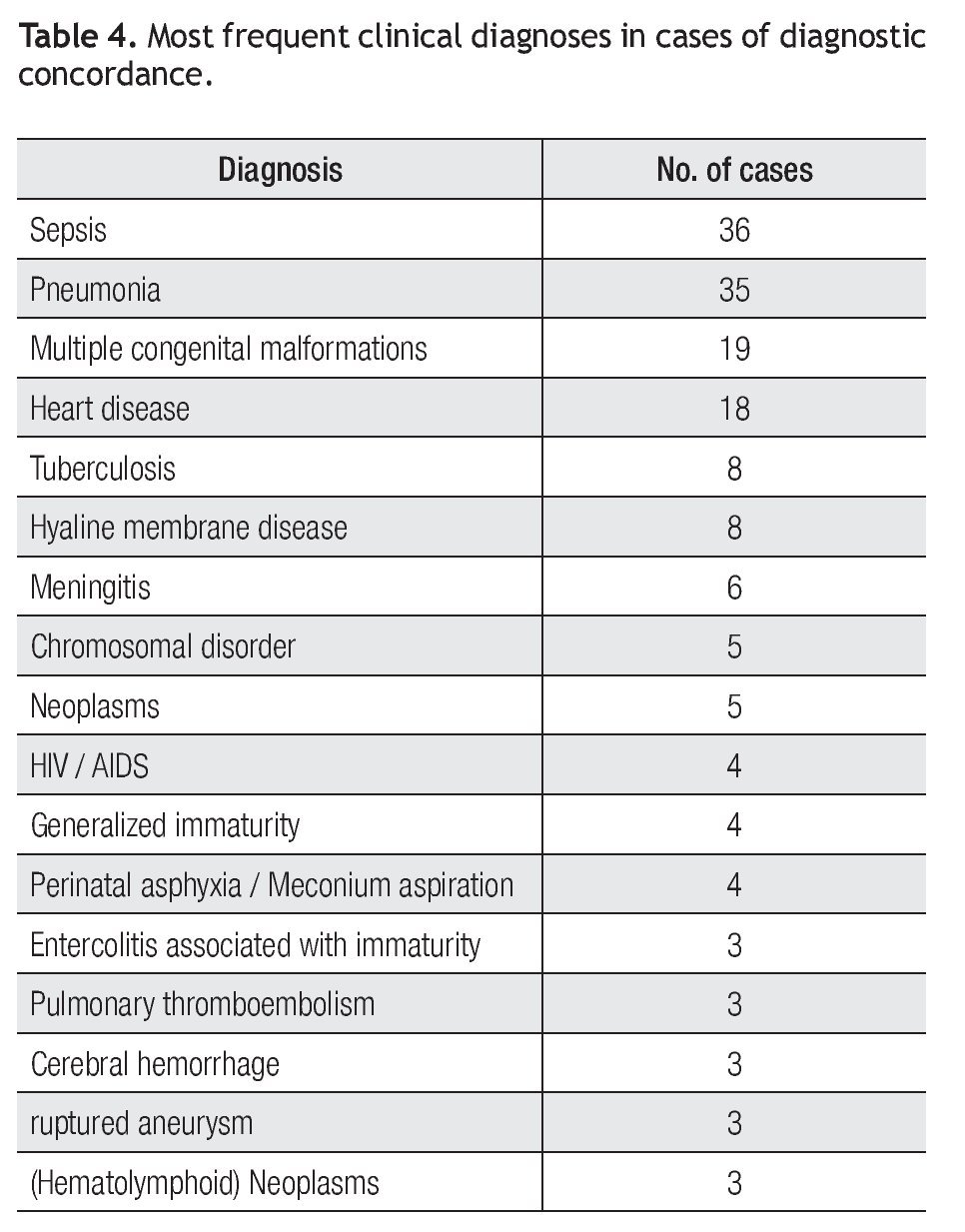
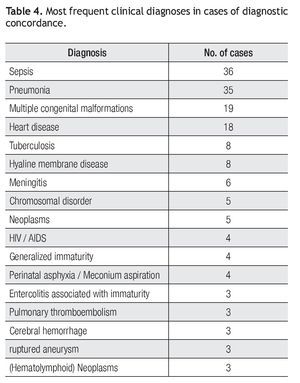
In 194 cases (58.6%), clinical diagnoses actually correlated with the final autopsy diagnoses. The most frequent diagnosis was sepsis (36 cases / 18.6%), followed in decreasing order by pneumonia (35 cases / 18%), multiple congenital malformations (19 cases / 9.8%), heart disease, hyaline membrane disease, and tuberculosis, (eight cases each / 4.1%), meningitis (six cases / 3%), chromosomal disorders and neoplasms (five cases / 2.6%), and other less frequent diagnoses (Table 4).
In a previous unpublished study carried out at our hospital we analyzed diagnostic concordance in 327 autopsies conducted between 1987 and 1996. We found 55% concordance, while the clinical diagnoses did not correlate with the histopathological diagnoses in 45% of cases. The main discordant diagnoses corresponded to pneumonia (19%), neoplasms (15%), CNS infections (13%), hyaline membrane disease and myocardial infarctions (10% each).
Discussion
The percentage of autopsies conducted at the University Hospital represents 6.8% of patients deceased in the hospital. This figure, albeit low, remains within the percentages reported in the literature. In the 1960s, the average percentage of autopsies performed in the United States and Europe was around 60%. However, since then such percentage has dropped and it currently stands at 10% or even less.14,15
In a study carried out in eight states of the USA, they found that this percentage has decreased from 10.9% in 1990 to 6.1% in 1999. Excluding forensic autopsies, the current percentage of autopsies performed at the Massachusetts General Hospital stands at 13% (approximately one autopsy per day).13 A high percentage of the deaths at our hospital results from violent events and the autopsies conducted are of the medico-legal type, which is not included in this study. According to some publications, the average autopsy rate at Mexico's national health institutes varies between 25% and 30%.9 Other studies carried out in Mexico report average autopsy rates between 10% and 37% for the Federal District (Mexico City) and between 0.2% and 58% for the rest of the country, according to figures reported in 1984. It is accepted that for a general teaching hospital, the average autopsy rate should be between 20% and 30%.16
According to some published studies, relevant clinically unsuspected findings that could have changed patient prognosis if medically controlled or treated are found in 20% to 40% of autopsies.13 It is important to point out that the diagnostic discrepancy rate has not decreased significantly over the last 30 years, in spite of the developments in diagnostic methods.7
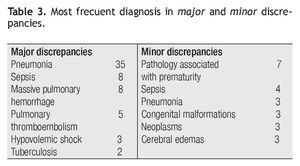
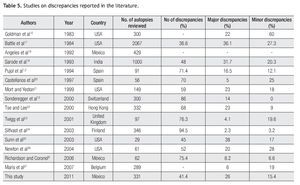
In this study, 366 autopsies were analyzed and diagnostic discrepancies were found in 41.4% of them. Twenty six percent of such discrepancies were major discrepancies and 15.4% were minor discrepancies. This is in keeping with the figures reported in the literature.17-27 (Table 5). The factors that play a role on this situation vary in nature and they range from the availability of appropriate technology and means and a rational and judicious use of laboratory and imaging tests to establish the diagnosis to the practice of good clinical medicine as the basis to be guided to an appropriate diagnosis. Another important factor is the length of hospital stay. Tavora analyzed a total of 291 cases and found major discrepancies which were associated to a short length of hospitalization (less than 24 hours) in 50 cases (17.2% of autopsies). In contrast, in our study the majority of discrepancies corresponded to patients whose length of hospitalization was greater than 24 hours.3
In a study published by Bonds, 276 cases of autopsies on patients with infectious pathologies were analyzed. One hundred and eighty two of these patients were adults, 137 of them (75.3%) had an infectious disease at the moment of the autopsy and in 43.1% of these cases the disease had not been suspected clinically. Forty eight percent of pediatric patients had an infectious disease at the moment of the autopsy and in 58% of these cases the disease was clinically unsuspected.28 As part of our results, we found that the most common infectious pathology overall was pneumonia, both for discrepancy cases and non-discrepancy cases.
Richardson et al analyzed 62 autopsies and found differences in the main clinical diagnosis in 24.6% of cases. In accordance with Goldman's classification as modified by Battle, they found type I discrepancies in 8.2% of cases and type II discrepancies in 6.6% of cases. Type I consists of major discrepancies that may extend patient's life with appropriate therapeutic management. Type II consists of minor discrepancies whose detection before death would have probably not changed survival even with appropriate treatment.9,17
Autopsies continue to be a valuable source for the detection of unsuspected diagnoses since on occasions it is still difficult to establish a correct diagnosis and errors are unavoidable in spite of good medical practices and the advent of new technology.29 Additionally, we also consider that autopsy protocols and all the documents in the medical record should contain all information necessary to carry out a diagnostic correlation analysis, thus preventing cases classified as "insufficient clinical information to perform correlation analysis". In our study 35 cases (9.6%) corresponded to this classification.
The results of this study prove the need for autopsies in order to identify patient pathologies conclusively since a high percentage of clinical diagnoses are wrong or incomplete, which is nonetheless in line with the reports in the literature.29 If we compare our current review (2004-2010) with the previous study carried out at our hospital (1987-1996), global discrepancy varied from 45% in the latter to 41.4% in the former. It is interesting to notice that pneumonia remains the most frequent unsuspected diagnosis, which also happens in studies reviewed in the literature.3,14,17 This shows how autopsies indicate that our hospitalized patients are dying from diseases that are apparently simple to diagnose but which for some reason are not being identified, causing us to miss the opportunity to provide adequate treatment. We believe that autopsies should be a mandatory procedure, particularly in those institutions linked to undergraduate and postgraduate medical education, and that it is essential to increase the number of autopsies to achieve real monitoring of this practice within the practice of medicine in order to keep and maintain a reliable medical information database, as well as to provide feedback with this information to the training programs of the different medical specialties.
Corresponding author: María Victoria González Franco.
Department of Pathology, University Hospital "Dr. José Eleuterio González" Av. Madero y Gonzalitos S/N Col. Mitras Centro, C.P. 64460. Monterrey Nuevo León, Mexico.
Phone: (+52) 81 8336 8181. Fax: (+52) 81 8348 5981.
E-mail:vicky_gzz@hotmail.com
Received: August 2011.
Accepted: November 2011