Acute abdominal pain is defined as pain of non-traumatic origin with a maximum duration of 5 days and it represents a common complaint of patients presenting at the emergency department (ED).1
There are many causes of acute abdominal pain that can be classified as urgent and non-urgent causes, the urgent causes require immediate treatment to prevent complications; mainly the location of pain can narrow the differential diagnosis. A complete evaluation is required to increase the diagnostic accuracy, leading to better outcomes.
The most frequent surgical emergency worldwide is acute appendicitis, with a lifetime risk of 7–8%, in low-income and middle-income countries mortality is reported as 1–4%.2 The diagnosis by clinical evaluation can be challenging in cases when the presentation is atypical and overlaps with other conditions, in these situations the use of image studies may be helpful. Delay of accurate diagnosis could result in rupture of the appendix, which is associated with worse prognosis.3 The objectives of an accurate and prompt diagnosis are lowering the normal appendectomy and perforation rates.
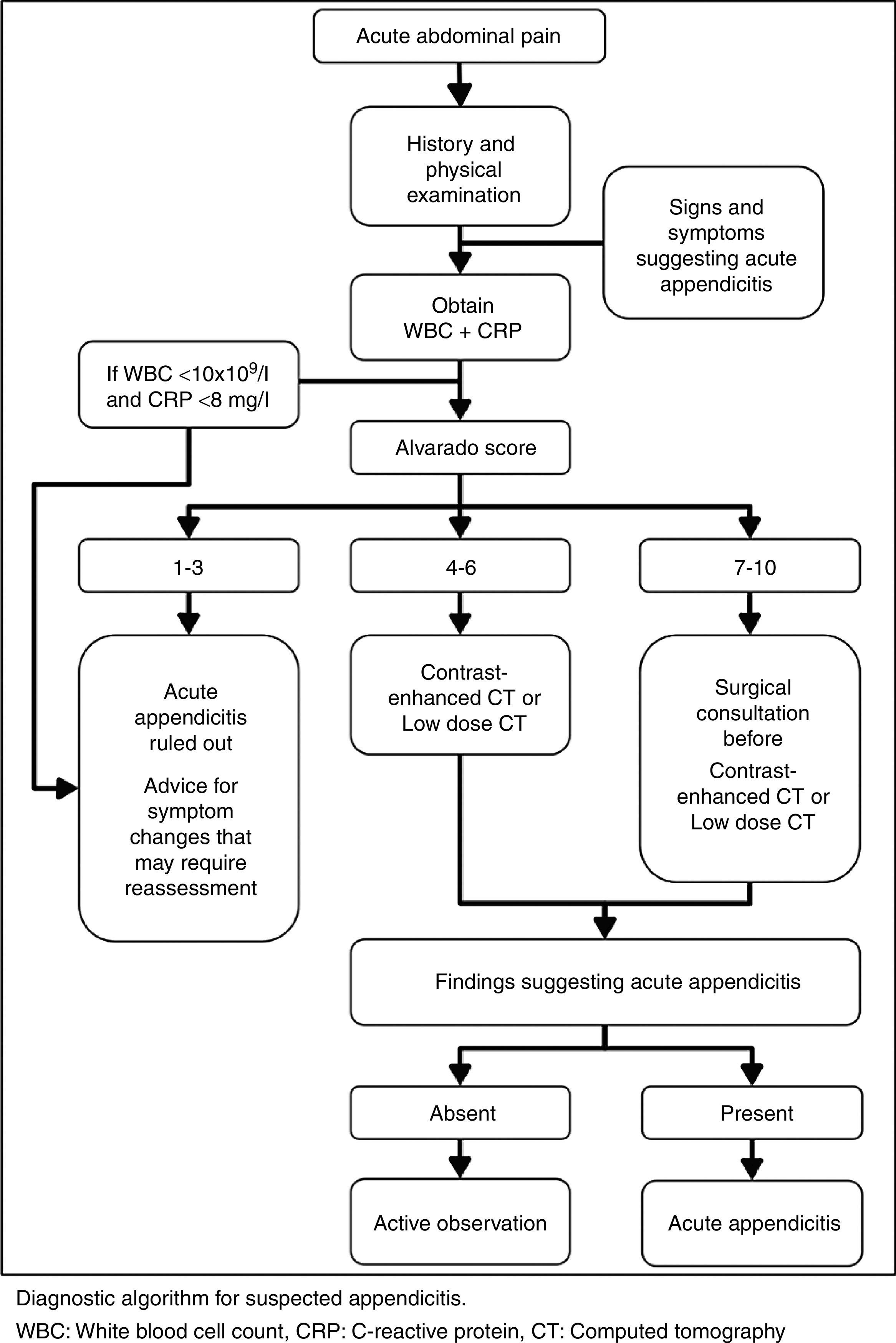
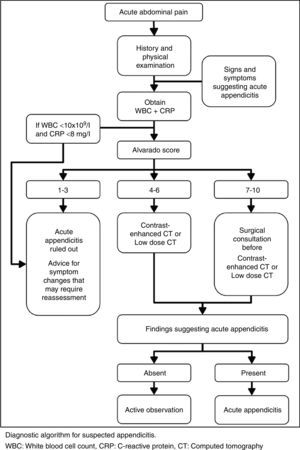
The authors recommend a diagnostic pathway in order to lower misdiagnosis, time to diagnosis and complications in patients in which acute appendicitis is suspected.
Initial evaluationHistoryThe initial evaluation consists in history and physical examination; the differential diagnosis will be narrowed by the pain's location, radiation, and migration. General information about onset, duration, severity, quality of pain, associated symptoms, exacerbating and remitting factors should be described.4
For appendicitis, right lower quadrant pain has the highest positive predictive value, although migration from periumbilical to right lower quadrant pain and fever also suggest the diagnosis.4 Appendicitis is also associated with gastrointestinal symptoms like nausea, vomiting, and anorexia. Variations in the anatomic location of the appendix may account for the differing presentations of the somatic phase of pain.5 The order of development of symptoms and signs in appendicitis are epigastric or periumbilical pain, anorexia, nausea, vomiting, tenderness in lower abdomen, fever, and leukocytosis.6
Gastrointestinal symptoms that develop before the onset of pain suggest a different etiology such as gastroenteritis.5
Symptoms in patients with abdominal pain that are suggestive of surgical or emergent conditions include fever, protracted vomiting, syncope or pre-syncope, and evidence of gastrointestinal blood loss.4
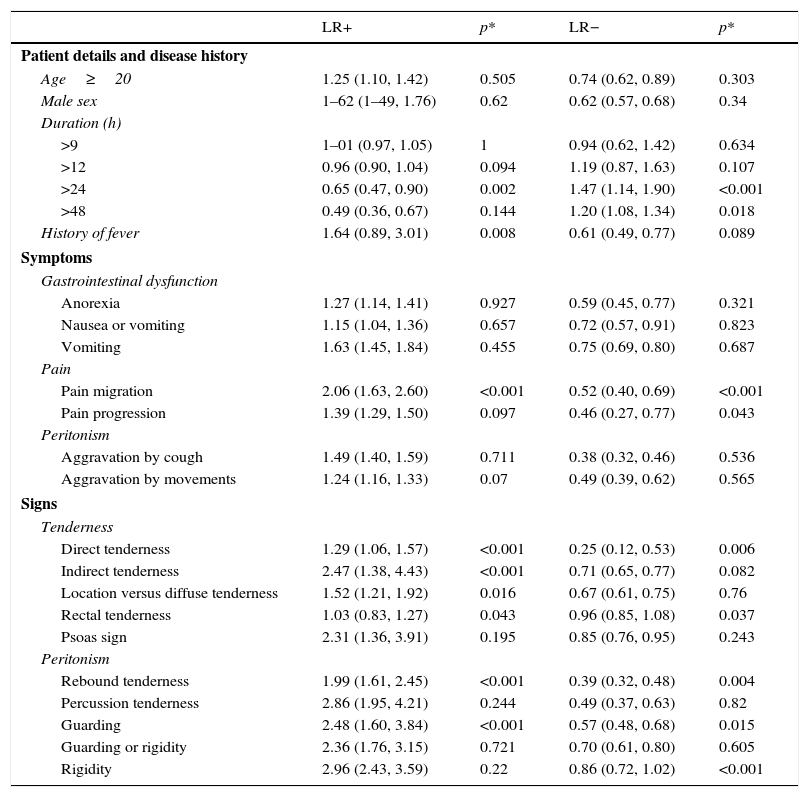
Physical examinationThe vital signs and general appearance should be noted first in the physical examination.4 In early presentation pulse rate and body temperature may be normal or slightly elevated. The peritoneal irritation will determine the presence of the next physical findings: tenderness at or near the McBurney's point, muscular resistance (guarding) may be felt on deep palpation, and sudden pain when the hand is quickly relieved (rebound). Indirect tenderness (Rovsing's sign) and indirect rebound tenderness (pain in the right lower quadrant when the left lower quadrant is palpated) are strong indicators of peritoneal irritation.5 Psoas sign and obturator sign indicates inflammation near the muscles.5 The positive and negative likehood ratios of the sings and symptoms were calculated in a meta-analysis (Table 1).7
Predictive power of elements of history and clinical examination in the diagnosis of appendicitis, expressed as pooled likelihood ratios.7
| LR+ | p* | LR− | p* | |
|---|---|---|---|---|
| Patient details and disease history | ||||
| Age≥20 | 1.25 (1.10, 1.42) | 0.505 | 0.74 (0.62, 0.89) | 0.303 |
| Male sex | 1–62 (1–49, 1.76) | 0.62 | 0.62 (0.57, 0.68) | 0.34 |
| Duration (h) | ||||
| >9 | 1–01 (0.97, 1.05) | 1 | 0.94 (0.62, 1.42) | 0.634 |
| >12 | 0.96 (0.90, 1.04) | 0.094 | 1.19 (0.87, 1.63) | 0.107 |
| >24 | 0.65 (0.47, 0.90) | 0.002 | 1.47 (1.14, 1.90) | <0.001 |
| >48 | 0.49 (0.36, 0.67) | 0.144 | 1.20 (1.08, 1.34) | 0.018 |
| History of fever | 1.64 (0.89, 3.01) | 0.008 | 0.61 (0.49, 0.77) | 0.089 |
| Symptoms | ||||
| Gastrointestinal dysfunction | ||||
| Anorexia | 1.27 (1.14, 1.41) | 0.927 | 0.59 (0.45, 0.77) | 0.321 |
| Nausea or vomiting | 1.15 (1.04, 1.36) | 0.657 | 0.72 (0.57, 0.91) | 0.823 |
| Vomiting | 1.63 (1.45, 1.84) | 0.455 | 0.75 (0.69, 0.80) | 0.687 |
| Pain | ||||
| Pain migration | 2.06 (1.63, 2.60) | <0.001 | 0.52 (0.40, 0.69) | <0.001 |
| Pain progression | 1.39 (1.29, 1.50) | 0.097 | 0.46 (0.27, 0.77) | 0.043 |
| Peritonism | ||||
| Aggravation by cough | 1.49 (1.40, 1.59) | 0.711 | 0.38 (0.32, 0.46) | 0.536 |
| Aggravation by movements | 1.24 (1.16, 1.33) | 0.07 | 0.49 (0.39, 0.62) | 0.565 |
| Signs | ||||
| Tenderness | ||||
| Direct tenderness | 1.29 (1.06, 1.57) | <0.001 | 0.25 (0.12, 0.53) | 0.006 |
| Indirect tenderness | 2.47 (1.38, 4.43) | <0.001 | 0.71 (0.65, 0.77) | 0.082 |
| Location versus diffuse tenderness | 1.52 (1.21, 1.92) | 0.016 | 0.67 (0.61, 0.75) | 0.76 |
| Rectal tenderness | 1.03 (0.83, 1.27) | 0.043 | 0.96 (0.85, 1.08) | 0.037 |
| Psoas sign | 2.31 (1.36, 3.91) | 0.195 | 0.85 (0.76, 0.95) | 0.243 |
| Peritonism | ||||
| Rebound tenderness | 1.99 (1.61, 2.45) | <0.001 | 0.39 (0.32, 0.48) | 0.004 |
| Percussion tenderness | 2.86 (1.95, 4.21) | 0.244 | 0.49 (0.37, 0.63) | 0.82 |
| Guarding | 2.48 (1.60, 3.84) | <0.001 | 0.57 (0.48, 0.68) | 0.015 |
| Guarding or rigidity | 2.36 (1.76, 3.15) | 0.721 | 0.70 (0.61, 0.80) | 0.605 |
| Rigidity | 2.96 (2.43, 3.59) | 0.22 | 0.86 (0.72, 1.02) | <0.001 |
LR, likelihood ratio.
In the physical examination for evaluation of appendicitis, digital rectal examination (DRE) has been considered necessary, it has been described that when the appendix hangs into the pelvis, abdominal findings may be absent; right-sided rectal tenderness is said to help in this situation.5 For DRE a meta-analysis found a pooled sensitivity of 0.49 (95% CI 0.42–0.56), the pooled specificity was 0.61 (95% CI 0.53–0.67), the pooled Positive Likelihood Ratio (LR+) was 1.24 (95% CI 0.97–1.58), the pooled Negative Likelihood Ratio (LR−) was 0.85 (95% CI 0.70–1.02), and the diagnostic odds ratio (DOR) was 1.46 (0.95–2.26).3 Considering sensitivity, specificity and the discomfort the DRE causes, Toshihiko T. et al. question the necessity of DRE in patients with suspected appendicitis.
Laboratory testsWhen acute appendicitis is suspected after initial evaluation a white blood cell count (WBC) with differential and C-reactive protein (CRP) must be ordered. No inflammatory marker alone, such as white blood cell count, C-reactive protein, or other novel tests, including procalcitonin, can identify appendicitis with high specificity and sensitivity.2
Appendicitis was more likely in patients with a strong inflammatory response, high granulocyte counts or WBC, high proportion of PMN cells or increased CRP concentration.7
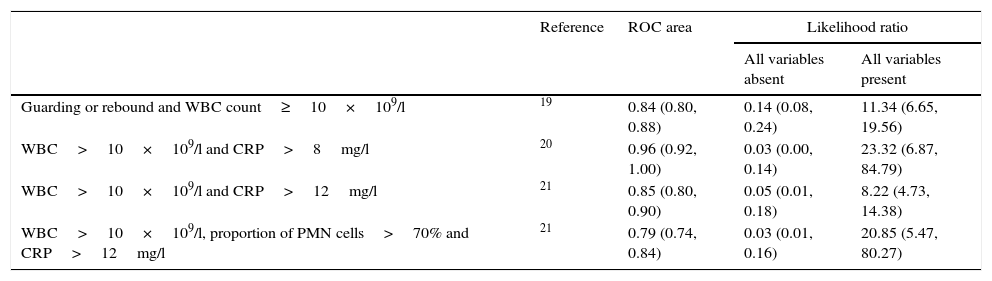
Appendicitis was likely when two or more descriptors of inflammation were increased, with a LR+ of more than 10; it was unlikely when all markers of inflammation were normal, with a LR− of less than 0.10 (Table 2).7
Discriminatory and predictive power of combinations of variables.7
| Reference | ROC area | Likelihood ratio | ||
|---|---|---|---|---|
| All variables absent | All variables present | |||
| Guarding or rebound and WBC count≥10×109/l | 19 | 0.84 (0.80, 0.88) | 0.14 (0.08, 0.24) | 11.34 (6.65, 19.56) |
| WBC>10×109/l and CRP>8mg/l | 20 | 0.96 (0.92, 1.00) | 0.03 (0.00, 0.14) | 23.32 (6.87, 84.79) |
| WBC>10×109/l and CRP>12mg/l | 21 | 0.85 (0.80, 0.90) | 0.05 (0.01, 0.18) | 8.22 (4.73, 14.38) |
| WBC>10×109/l, proportion of PMN cells>70% and CRP>12mg/l | 21 | 0.79 (0.74, 0.84) | 0.03 (0.01, 0.16) | 20.85 (5.47, 80.27) |
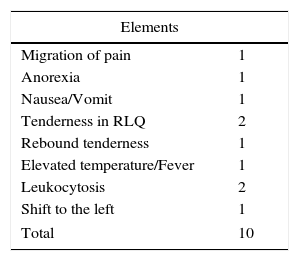
Alvarado A. developed a score in 1986 based in symptoms, signs and laboratory findings (Table 3). The predicted number of patients with appendicitis is 30% in those with score 1–4 (low-risk), 66% with 5–6 (intermediate risk) and 93% in scores 7–10 (high risk). He proposed that patients with a score of 5–6 should be observed, and a score of 7 and more requires surgery.8
Alvarado score.8
| Elements | |
|---|---|
| Migration of pain | 1 |
| Anorexia | 1 |
| Nausea/Vomit | 1 |
| Tenderness in RLQ | 2 |
| Rebound tenderness | 1 |
| Elevated temperature/Fever | 1 |
| Leukocytosis | 2 |
| Shift to the left | 1 |
| Total | 10 |
An Alvarado score of 1–4 has a sensitivity of 99% in the overall population, 96% for men and 99% for women. However, a higher Alvarado scores (7–10), has limited clinical value since it has a specificity of 82% in overall population, 57% for men, 73% for women. In women the score over-predicts the probability of appendicitis and should be used with caution. As a sole decision criterion for surgery (cut point of 7) the score produces negative appendectomy rates from 13.3% to 16.2%.9
A discharge decision by ruling out acute appendicitis can be made if the patient has an Alvarado score of 1–4, but it is important to warn the patient for symptom changes that may require re-assessment. An intermediate-high risk Alvarado score (5–10) cannot be used to diagnose acute appendicitis since it has low specificity, in these patients the use of image studies should may be appropriate.
By correlation between Alvarado score and diagnostic findings in computed tomography (CT) for acute appendicitis, a score of 3 or lower had an incidence of 3.7% of acute appendicitis (96% sensitivity), and those of a score 7 or higher had an incidence of 77.7% of acute appendicitis (100% specificity). Those with a score between 4 and 6 had specificity of 94%. McKay R. recommends CT on patients with an Alvarado score from 4 to 6, in patients with 7 or more, a surgical consultation is recommended before the CT. CT is not recommended in scores of 3 or less, since it may delay diagnosis and time in ED.10
Imaging studiesIn adolescent and adult patients, computed tomography (CT) has become the most widely accepted imaging strategy.2 Twelve studies were reviewed by Terasawa S. et al. in which CT and US were evaluated as diagnostic tools for acute appendicitis, finding that CT had pooled estimates of 0.94 (95% CI 0.91, 0.95) for sensitivity, 0.95 (95% CI: 0.93, 0.96) for specificity, 13.3 (95% CI: 9.9, 17.9) for the positive LR and 0.09 (95% CI: 0.07, 0.12) for the negative LR. Ultrasonography had pooled estimates of 0.86 (95% CI: 0.83, 0.88) for sensitivity, 0.81 (95% CI: 0.78, 0.84) for specificity, 5.8 (95% CI: 3.5, 9.5) for the positive LR and 0.19 (95% CI: 0.13, 0.27) for the negative LR, concluding a better diagnostic performance by CT.11
On 5-mm-section contrast-enhanced helical CT examinations, one enlarged appendix, appendicular wall thickening, peri-appendicular fat stranding, and appendicular wall enhancement were the most useful findings for diagnosing acute appendicitis.12
In cases of abdominal pain suspected to be appendicitis, imaging studies were more cost-effective than physical exam to make accurate diagnostic decisions. Tomography offers the best cost-effectiveness in prepaid system and in public health system.13 The use of CT reduces the negative appendectomy rate to 6% compared with no CT approach.2,14–16 The use of CT in the absence of an expedited imaging protocol may delay surgery, but this is not associated with increased appendicular perforation rates.17
However, CT radiation is a common concern in children and young patients, reducing the radiation without affect the accuracy which can be achieved with a low-dose CT. Low-dose CT was non-inferior to standard-dose CT with respect to negative appendectomy rates in young adults with suspected appendicitis.18
ConclusionsThe diagnosis by clinical evaluation can still be challenging in cases where presentation is atypical and overlaps with other conditions, there is continuous effort in evaluating clinical, laboratory and image findings in order to make an accurate and early diagnosis. It is not recommended a diagnosis made merely by clinical evaluation since it may increase the normal appendectomy rate, also a routine CT is not recommended because unnecessary radiation exposure and increases costs in low risk situations; a systematic evaluation combining clinical evaluation, laboratory and imaging depending on Alvarado score is proposed in order to lower misdiagnosis and normal appendectomy rate. The recommend approach for us is shown in Fig. 1.
FundingNo financial support was provided.