Objective: To determine whether a falls prevention program reduces the incidence of falls within a hospital.
Materials and methods: Each patient admitted to the Internal Medicine ward was classified into a risk category (high, medium, low) according to the scale of J.H. Downton, and then various general and specific measures were applied by risk group. Interventions included appointments, teaching materials, and training of medical staff and family. Furthermore, a registration system was developed that allowed adverse event feedback to the program and identification of the causes of the fall. The SPSS version 20.0 was used for the data analysis. Descriptive analysis was used for quantitative variables, and qualitative variables were expressed as proportions. To compare the rate of pre- and post-program implementation falls, χ2 was used, with a ρ = 0.05 determining a significant statistical value.
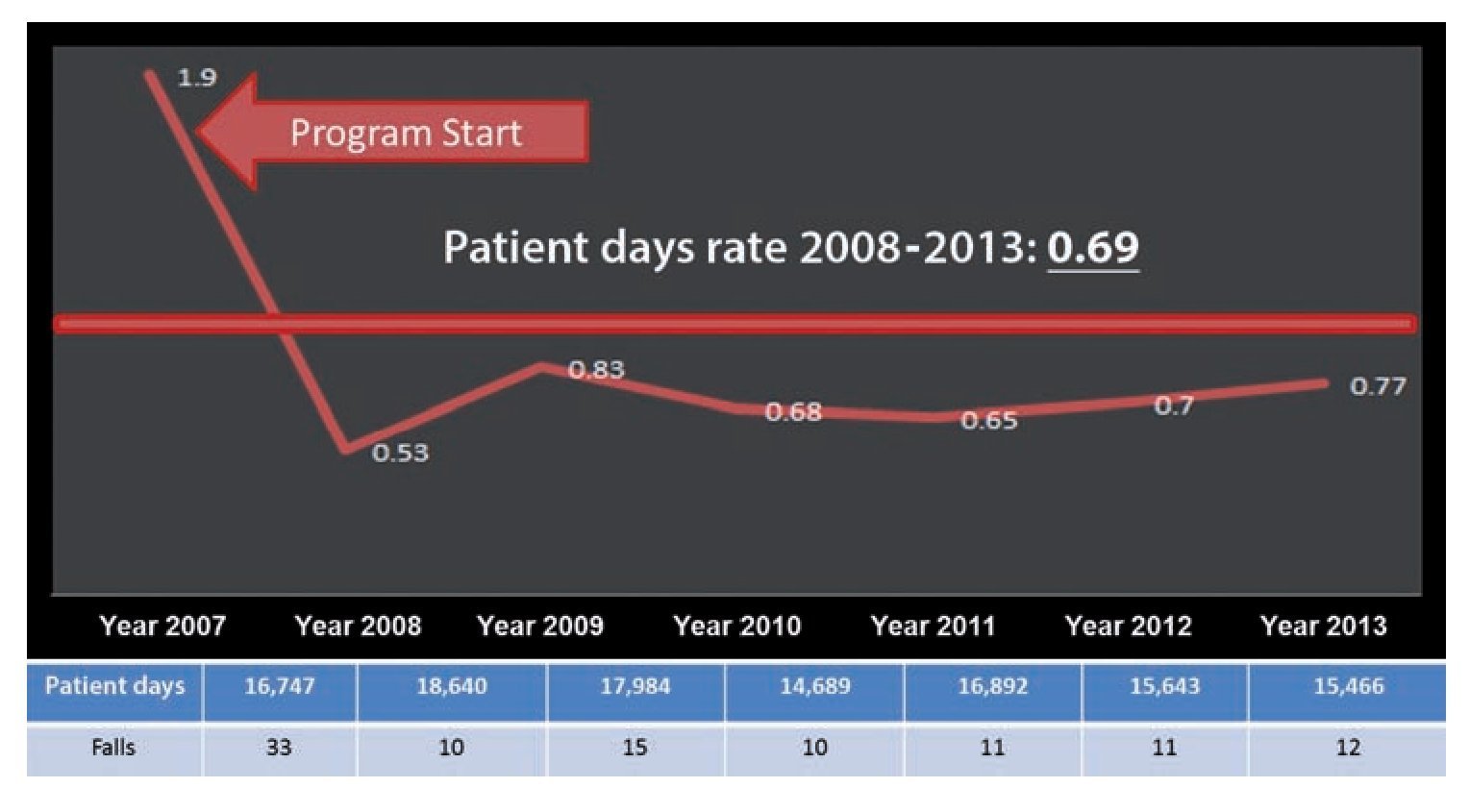
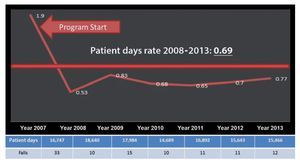
Results: Since the implementation of the program, the rate of falls per 1000 days/patient decreased from 1.9 in 2007 to 0.67 in the period 2008-2013, representing a decrease of the rate of falls of up to 70%, with a statistically significant difference (P=.02).
Conclusions: The implementation of a falls prevention program is an effective tool and reduces the rate and complications associated with them.
Introduction
According to the World Health Organization (WHO), a fall is defined as an “involuntary event causing an individual to lose his/her balance and precipitate to the ground or any other firm surface which stops them.”1
Falls are common in hospitals, and are responsible for up to 40% of adverse events associated with patient safety. The prevalence of in-hospital falls varies depending on institutional characteristics and types of inpatients, with reported rates going from 1.4 to 13.0 falls for every 1000 days/patient.2 Fall-related injuries occur in between 15 and 50% of the events. Injuries range from contusions, scratches and ecchymosis to fractures, hemorrhages, and post-fall syndrome, among others, increasing morbidity and compromising recovery, length of in-hospital stay as well as in-hospital costs, and in worst-case scenarios an increase in mortality.2
Because of this, in-hospital falls have become a new focus of attention, not only because of the repercussions on the patients and their families, but also for the institutional repercussions, going from medical to economical and legal. Therefore, in The International Patient Safety Goals it is stipulated in goal 6: “Reduce the risk of patient harm resulting from falls”, hence it is a priority for each health institution to have a fall-prevention strategy in order to improve patient safety.3
In our hospital, from 2007 onwards, as a result of the efforts made by Dr. Félix Héctor Rositas Noriega, an Integral Patient Care Program was implemented in the Internal Medicine Unit, which included a series of groundbreaking programs in our institution designed to ensure in-patients’ care and safety, as well as a special section for fall-prevention.
This year, following a situational diagnosis of the Internal Medicine Unit, it was determined that the fall rate was 1.9/1000 days/patient. While it is true that the fall rate was within the ideal range according to medical literature as per the reported in international hospitals (1.4-13.0 falls/1000 days/patient), it was also determined that it could decrease, mostly because there wasn’t a fall-prevention strategy, pointing out the following deficiencies: a) an inadequate fall-prevention infrastructure; b) lack of medical and non-medical training; c) lack of timely and proper structure education for the patients and their families; d) there was no register with a pre-set and order form for the reporting of falls, and e) absence of an internal supervision committee.
The main goal of the program was to standardize the use of a technical, trustworthy tool, applicable to our population, which unifies risk classification criteria in all patients admitted to the Internal Medicine Unit in order to lower fall incidence. At the same time, the following secondary goals were established: to identify the degree of risk of falling of all patients admitted to the IMU, make use of available resources necessary for patient safety, lower the number of falls through the implementation of preventive measures and educate the patient and his/her family in fall prevention.
Materials and methods
The Fall Prevention Program has been in practice since 2008 to this day in the Internal Medicine Ward of the “Dr. José E. González” University Hospital, and is applied to each and every admitted patient.
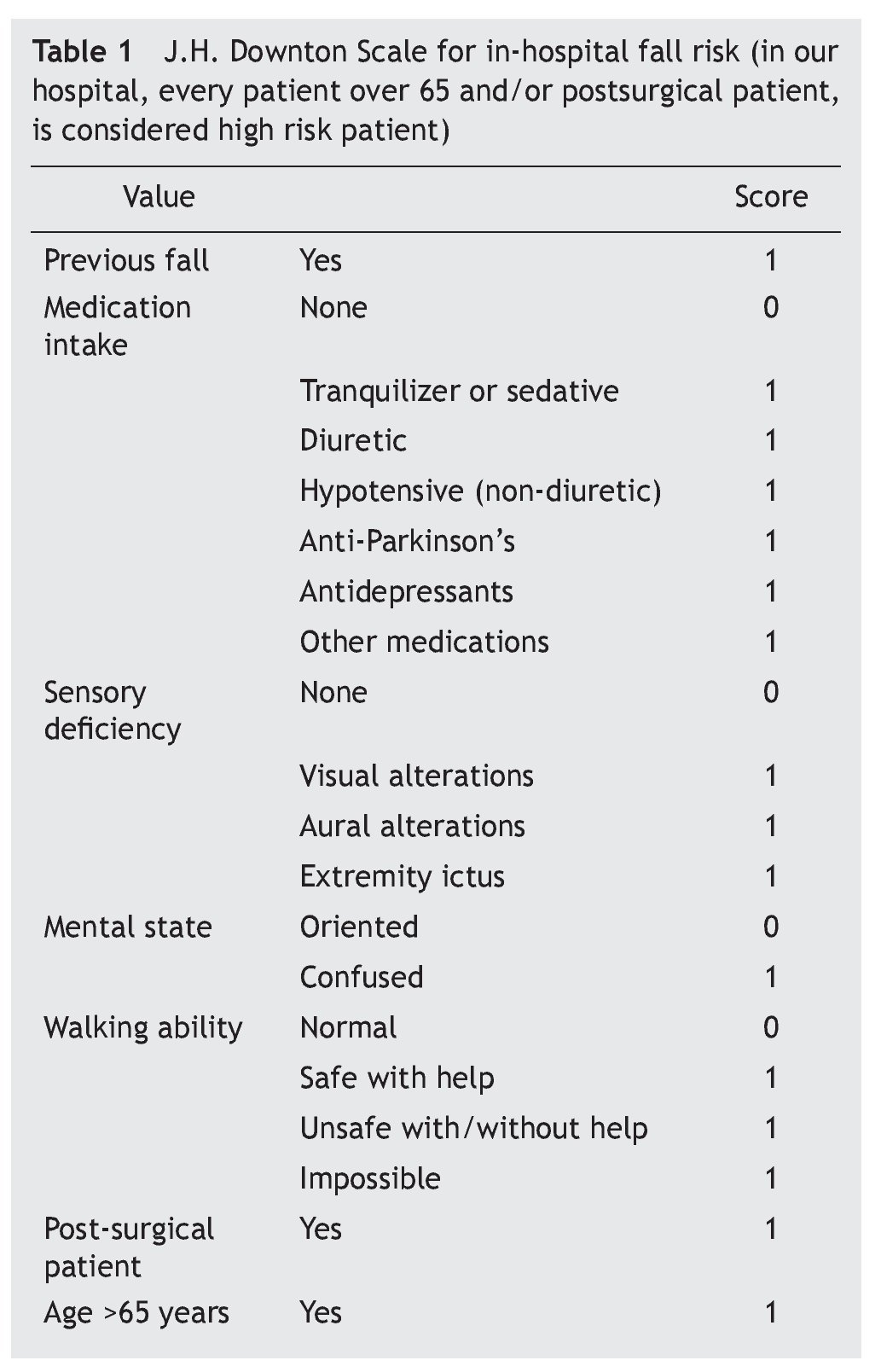
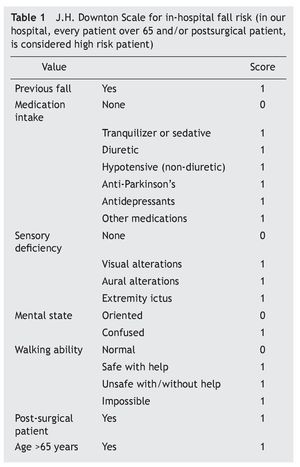
Several actions were necessary in order to implement the program concerning infrastructure and input: an intercom was installed at every bed in the ward, guardrails were installed on every bed, patient straps/fasteners were acquired, lamps were placed at every bed’s headboard and identification bracelets were used on patients with a high fall risk. In addition, information brochures were handed out to every patient’s family, a fall prevention placard was placed in every room, and an informational video was continuously projected outside the department’s main office. Finally, during information hours personalized education was provided to each family member for their patient’s care, and medical personnel and nursing staff were trained in the registration and care of patients who suffered a fall. As a screening tool, every patient admitted to the Internal Medicine Ward was administered the J.H. Downton Scale upon entry, and according to the score were divided into three categories: low risk (1 point), moderate risk (2 points) and high risk (3 or more points) (table 1).
For patients with low and moderate risk of falling, the following actions were implemented: a green (low risk) or yellow (moderate risk) sign was placed on the headboard of the patient; identifications of fall risk factors (physical, mental and pharmacological), warning the patient and family members of this risk; installation of guardrails and an intercom bell; placement of a placard in order to prevent falls; notification to family members of the risk; proper illumination in hallways and stairs; and frequent rounds to the assigned patients’ ward.
In high risk patients, in addition to the previous actions, we took the following actions: a red sign identifying them as high-risk fall patients was placed on the patient’s head-board; a blue bracelet with the inscription “HIGH FALL RISK” was given to the patient; a permanent pass for a family member was provided; and if necessary, bed straps/fasteners were installed, upon signed consent by a direct family member (the doctor and family members were notified of the need for these measures).
Moreover, since 2013, we reassessed patients who have undergone any surgical approach or minor procedure (bronchoscopy, upper endoscopy, etc.), with the purpose of assessing their state of consciousness as a consequence of sedation, the procedure and anatomical alterations that may compromise walking, thus avoiding falls.
In case a patient presents an active fall an emergency code is activated, and the Internal Medicine Ward personnel perform the following protocol: the nursing staff notifies the doctor in charge or the on-call doctor and it is among his/her functions to assist and assess the patient and provide follow-up during the patient’s stay. Additionally, she/ he is in charge of filling out the fall registration form. The on-call doctor is in charge of evaluating the patient to determine if there is any type of injury; once the doctor’s evaluation is done, it is reported to the doctor in charge of that patient. That doctor is responsible for reassessing and following-up until the patient is discharged. Lastly, the supervisor nurse must identify the cause of the fall and monitor proper compliance of preventive measures.
In the adverse event registration form, date and time of the adverse event, date and time of the report, the patient’s general information, diagnosis as a cause of internment, description of the event, medial report, analysis of the event (with identification and cause) and evaluation of the preventive measures are all recorded.
The analysis of information was performed using the statistical software SPSS version 20.0; a descriptive analysis was used for quantitative variables and qualitative variables were expressed as proportions; in order to compare fall rates previous and subsequent to the implementation of the program an χ2 was used, determining a statistically significant value of P<.05.
Results
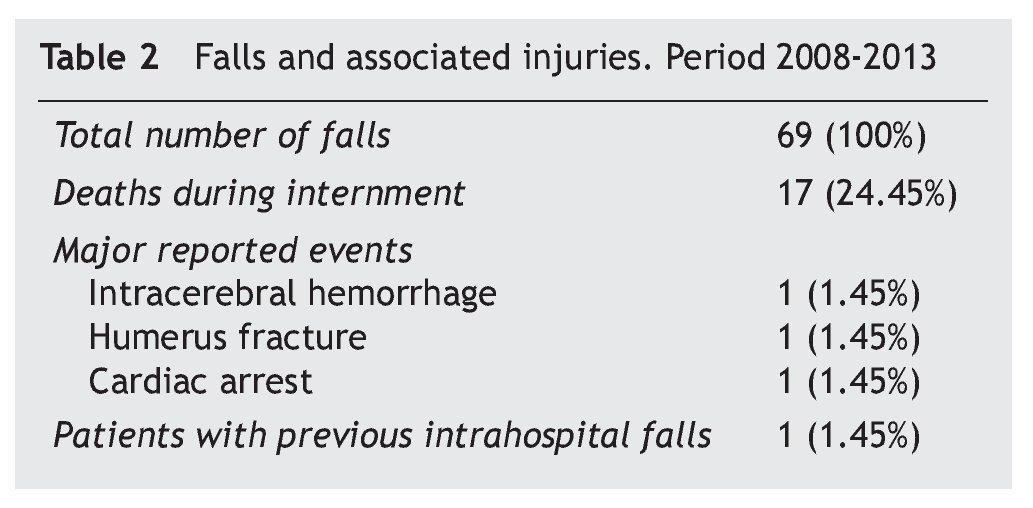
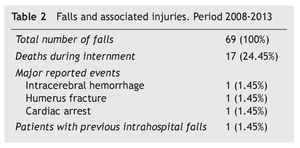
Since the program’s implementation in 2008, there have been 69 falls in 67 patients up to November 2013, of a total of 16,032 patients admitted to the Internal Medicine Ward (which represents a total of 99,314 days/patient). In tables 2 and 3 there is a summary of the characteristics of the patients. During this period of time, most of the patients just presented minor injuries, like scratches or ecchymosis. However, among the major events reported there was a patient who suffered a humerus fracture, a patient with intra-cerebral hemorrhage and a patient who was found with cardiac arrest at the moment of the fall (this patient recovered and days later was discharged from the hospital).
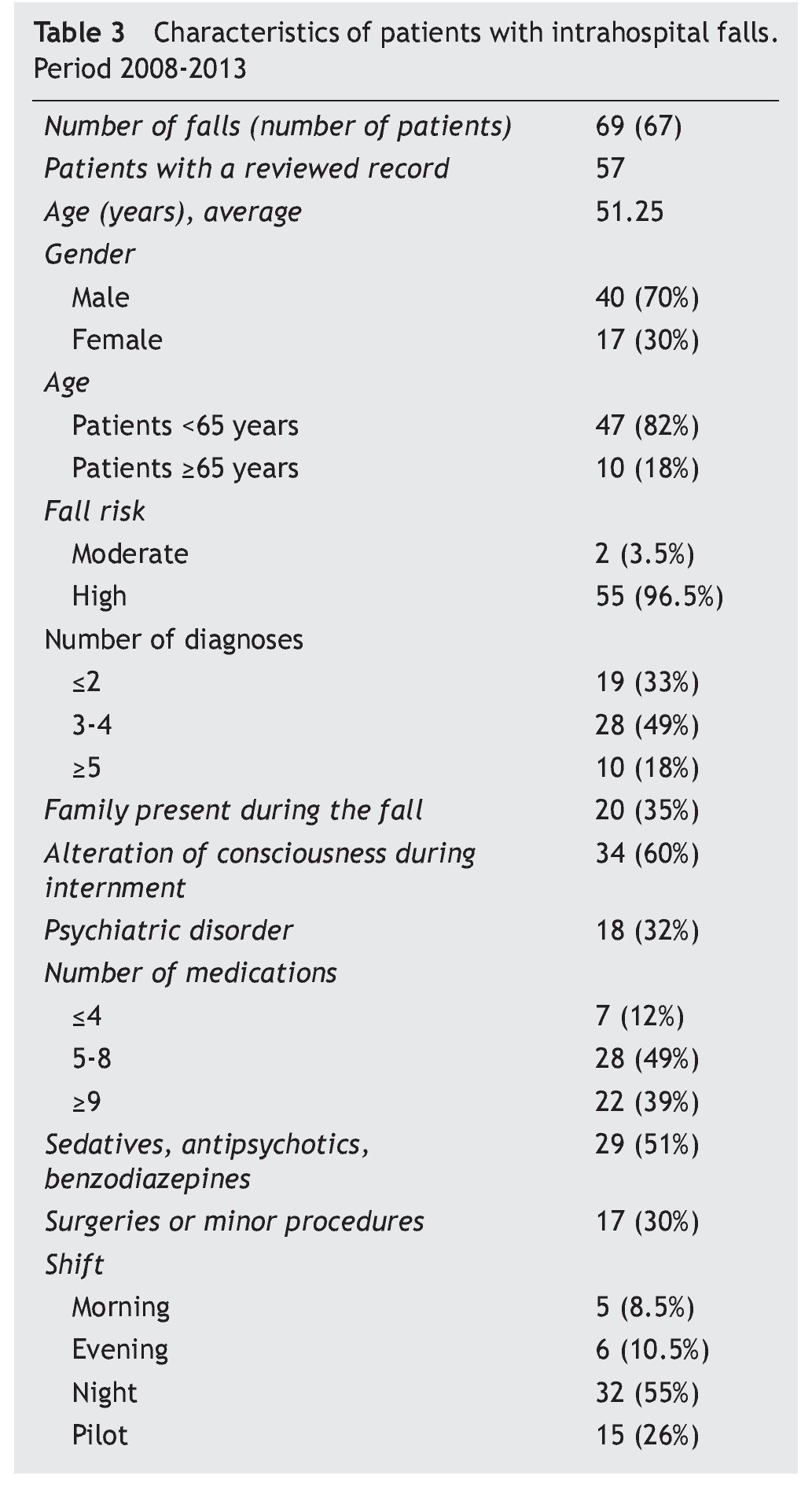
The files of the patients who suffered a fall were reviewed, with the purpose of making a demographic analysis; 57 out of the 67 files were reviewed (the rest of the files had already been depurated from the hospital’s archives).
The average age of the patients with a fall was 51 (range, 20-94) years old, with 82% of the patients under 65, and with a male predominance (70%). Most of the patients (96.5%) were classified as high-risk fall patients and therefore, as previously mentioned, received general and specific measures for fall prevention during their in-hospital stay. During their internment 67% of the patients had three or more diagnoses, which agrees with medical literature, which suggests that patients with two or more diagnoses have a greater fall risk.4 Even though family members of high risk patients are provided a permanent entry pass, only 35% of them were present at the moment of the adverse event.
A total of 60% of the patients presented some degree of conscience alteration due to a disease which necessitated internment: hepatic encephalopathy, uremic encephalopathy, encephalopathy by sepsis, hypoglycemia and hyperglycemia. Also, 32% of the patients had a history of psychiatric disease: dementia, major depression, bipolar disorder, schizophrenia, personality disorders and drug addictions/ withdrawal syndrome, the last one being the most common (present in 8 patients).
During their internment, 88% of the patients received six or more medications and 50% received some type of sedative or antipsychotic, due to their base disease or a surgical or minor procedure (endoscopy, bronchoscopy, colonoscopy), which was in 30% of the cases. Last but not least, as shown in the table, over half of the patients presented a fall during the night.
Average in-hospital stay in our Internal Medicine Ward is approximately 6.6 days per patient, but in a patient who suffers a fall the average stay extends to 12.2 days.
The most frequent diseases of the patients who suffered a fall during their stay were acute pulmonary infections, tuberculosis, neoplasia, drug addictions, chronic liver disease, acute coronary syndrome (ACS), seizures, chronic renal failure, digestive tube bleeding, HIV/AIDS, and hypoglycemia caused by oral glucose-lowering drugs.
When comparing fall rates per 1000 days/patient before and after the implementation of the fall prevention program (2007 vs. 2008-2013), a P=.02 was obtained, which represents a statistically significant value, and it shows a positive impact on the implementation of the program.
Discussion
A falls prevention program is not only a prevention tool for this adverse event, but it is also one of the International Patient Safety Goals (IPSG6), according to the Hospital Certification Standards guide of The General Health Council.3 Although it is true that previous to the implementation of this program, the Department of Internal Medicine was already within the international reference ranges, with a 100 days/patient rate of 1.9, since 2008 fall rates have behaved as seen in figure 1. In this table, we are able to observe that in 2008 there was a drastic drop in fall rates subsequent to the implementation of the program, since then and up to this day it has remained within the range of 0.53-0.83/1000 days/patient. This translates to up to a 70% drop of fall rates.
Figure 1 Number of falls and days/ patients per year since 2007 up to 2013, as well as the 1000 days/patient rate.
It is important to point out that, contrary to the reviewed bibliography, where it is possible to find that patients over 65 years old are the most likely to fall,4 in our hospital it is a younger population (average age, 51 years old). Dykes et al compared four fall prevention programs in four different hospitals, observing that 52% of the patients who suffered a fall were female; on the other hand, Duarte et al observed that men were the population with the higher fall risk. In our hospital the gender with a higher fall risk is male, representing 70% of the events. Duarte et al observed that 51% of the patients fell during the night, and when compared to our hospital, it is possible to observe that over half the patients fall during the night, one of the possible causes is that the night shift nursing staff is up to 60% less compared to the other shifts. Alteration in the conscious state during internment of a patient is an important fall risk factor6 and in our population was present in 60% of the cases. Other risk factors frequently linked to fall risk reported in the literature are polypharmacy and the use of medications which decrease consciousness,6 and our study wasn’t the exception, representing up to 72% and 51%, respectively, thus representing an area of opportunity, to reassess the proper use of medications employed and to avoid polypharmacy. The performance of surgical or minor procedures is a risk factor, not only because of sedation, but also because those are moments where the patient presents well-defined alterations in his/her gait, and in our study 30% of the patients who suffered a fall had undergone some type of procedure.
The medical literature indicates that injuries caused by falls occur in between 15 and 50% of cases,1 resulting in a wide range of damages, going from fractures and injuries in soft tissues to post-fall syndrome, increase in in-hospital comorbidity, a longer hospital stay, higher costs and even death. In our hospital, only a small proportion suffered a direct injury from falls, scratches being the most common injury, representing a total of approximately 8.7% of injuries. Only one of the patients who fell presented an injury directly attributable to the adverse event, and it is a patient who subsequent to the event suffered a humerus fracture. In a different case, one of the patients presented an intracerebral hemorrhage during evaluation; however, in this case we cannot consider that the hemorrhage had been caused directly by the fall, because the patient had a high blood pressure diagnosis and type II diabetes, thus it is impossible to determine whether the fall was the cause or the consequence of the hemorrhage, and we considered it an associated event.
Similarly, in the case of the patient found with a cardiac arrest during evaluation after the fall, it was impossible to establish a direct link between the two.
In-hospital stay in patients who suffered a fall, as previously mentioned, was longer than patients who did not present this adverse event, which corresponds with medical literature which indicates that in-hospital falls affect not only the patients’ health, but also hospital costs and stays.8 Nevertheless, it is important to stress the fact that a factor that directly influenced fall patients’ stays was not determined, because most patients presented only minor injuries (table 3).
Among the limitations of our study, there are: a) previous to the program implementation in 2008, there are no detailed records of the number of falls nor injuries suffered by the patients, since registration was done voluntarily by the nursing staff; b) the falls prevention program results were only compared to the year prior to implementation (2007 vs. 2008-1013), and c) the study is only descriptive, since it only compares populations which had presented falls before and after the program implementation, in other words, a comparative analysis —between the population who presented an adverse event and the population who didn’t— wasn’t conducted which could have determined variables really linked to fall risk.
However, according to the obtained results, it is possible to make important conclusions, from which it is possible to create an improvement plan. Among the areas where we must work are night falls. Most fall incidence in our internment ward occurred during the night. One of the most important observations is that the number of nursing staff is lower by up to 60% compared to the rest of the shifts, consequently each nurse is assigned a larger number of patients to his/her care. In order to avoid this situation, the clinical field will be offered to the different nurse schools which go to our hospital-school, with the purpose of having a larger number of personnel taking care of the patients during the night.
Deeper attachment from family members: even though most patients in our internment ward are classified as high-risk fall patients, and thus are given a permanent pass for family members, they were found to be present in adverse events in only a third of the cases. In order to attempt a deeper attachment from family members, during information hours, in addition to brochures, family members will be made aware of the importance of care and patient attachment for fall prevention; moreover, during rounds, doctors in charge will reinforce the information, and in the case of observing a patient with social abandonment or a patient who they consider needs a deeper attachment from family members, a social worker will be notified in order to locate the patients family members through phone calls or home visits.
Supervision of the use of sedatives: from 2013 a reassessment of patients who undergo a surgical or minor procedure will be realized, with the purpose of evaluating patients after sedation. Therefore,we will soon obtain the first value reports of this measure.
Conclusions
After implementation of the falls prevention program, fall rates have dropped by up to 70%, according to the days/ patients rate in comparison to previous years. The program has proven to be a useful tool for the identification of patients with a high fall risk, which has allowed the implementation of specific actions in this group of patients. Also, following the information obtained with the registration of falls has made it possible to identify the main associated pathologies, causes and time, thus the program continuously receives feedback and improves. Thus, it can be concluded that the falls prevention program is a useful and effective instrument in the reduction of this adverse event, in addition to a reduction of associated complications.
Received: March 2014;
Accepted: July 2014
*Correspondence author:
Departamento de Medicina Interna,
Hospital Universitario “Dr. José Eleuterio González” de la Universidad Autónoma de Nuevo León,
Ave. Madero y Ave. Gonzalitos s/n Col. Mitras Centro, Monterrey, Nuevo León, México.
E-mail address:dreynaldolara@gmail.com (R. Lara Medrano).