Diaphragmatic paralysis is a pathology characterized by the elevation of a plastic and inactive atrophic diaphragm, followed by an injury to the spinal column or to the phrenic nerve. Because it involves the phrenic nerve, it is often associated with an injury at its exit in the spinal cord at the radicular level, at the conduct or in the peripheral nerve.
Clinical caseA 50-year-old male patient with a history of thoracic trauma and diagnosis of unstable thorax is admitted for progressive dyspnea in the following 8 months. Diaphragmatic paralysis is diagnosed and a laparoscopic diaphragmatic plicature is performed. Patient improved his clinical status by 29%.
DiscussionThe consequences of the elevation of a hemidiaphragm can be respiratory, causing hypoxemia and decreases in the ventilation–perfusion ratio. This procedure is considered a corrective surgery from the morphological and functional point of view.
ConclusionsOur patient's clinical status improved according to the Saint George respiratory questionnaire, thanks to an improved perfusion of the basal lung expansion. Laparoscopic diaphragmatic plicature is a safe procedure associated with a minimal hospital stay, and more cases need to be reported. This is the procedure of choice in our institution.
Diaphragmatic paralysis (DP) is a pathology characterized by the relaxation and elevation and of an atrophic, aplastic and inactive diaphragm followed by a phrenic or spinal cord injury.1 A report by Christensen et al. showed 38 cases out of 107,778 individuals from Denmark with a radiographic report of hemidiaphragm elevation. The real prevalence of this pathology remains unknown.
Diaphragmatic paralysis, which involves the phrenic nerve, has an etiology linked to injuries to the spinal cord at a radicular level, at the conduct or in the peripheral nerve. At a cervical level, it may be caused by trauma or an iatrogenic injury during neck surgery. Mediastinal-level involvement is caused by mediastinal tumors, tuberculosis or trauma. When DP does not involve the phrenic nerve, thoracoabdominal trauma or an adjacent disease, such as sub-phrenic abscesses, atelectasis or pleural infection might be the cause.
The etiology often remains without explanation. A study by Pielher et al.2 proved that the cause could not be identified in 57.5% of cases. Neoplasia and surgery are responsible in 33% of the cases.
Clinical caseA 50-year-old male patient without significant family history, personal history of type 2 diabetes and arterial hypertension both under adequate control. Surgical history of an appendectomy 28 years ago. A year before being consultation, the patient was admitted to the emergency room after being involved in a car accident where he suffered trauma to the left hemithorax. With an unstable thorax and pulmonary contusion which progressed to respiratory insufficiency requiring intubation, the patient was moved to the intensive care unit. The patient was discharged after 2 weeks without additional surgical management.
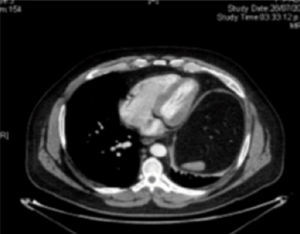
During the next eight months the patient presented progressive dyspnea, which was exacerbated by moderate to mild efforts; therefore, he went in for a medical assessment. The thoracic X-ray showed elevation of the left hemidiaphragm (Fig. 1) and the computer axial tomography (CAT) scan reported elevation of left hemidiaphragm and basal atelectasis, excluding associated pathologies (Fig. 2). A fluoroscopy was conducted under clinical suspicion (Fig. 3) confirming persistent elevation during breathing.
A St. George respiratory questionnaire (SGRQ)3 was conducted in order to assess the impact on his everyday life, producing an average of 57, with a symptomatology scale of 54, activities 70 and impact 48. Pulmonary function tests showed a severe restrictive process with a forced expiratory volume in the first second (FEV1) of 43 with 1.56L real and 3.5 theoretical, additionally a forced vital capacity (FVC) of 43 with 1.9L real and 4.4 theoretical. Preoperative arterial saturation was 92%.
Surgery was performed, 3 ports were introduced into the abdominal cavity: an umbilical, with a 30 degree camera, and two other 5mm ports. Diaphragmatic plication was done with intermittent non-absorbable 2–0 suture from medial to lateral direction. The process was repeated, ending with a double suture line. Operative time was 93minutes.
The patient was released on the third postoperative day. He was afebrile, tolerating oral diet and without dyspnea. Basal saturation was 97%, with a thoracic X-ray with radiological improvements (Fig. 4). The SGRQ was repeated 3 months later resulting in a reduction of 14 points (29%), patient referred symptomatic improvement.
DiscussionThe consequences of diaphragmatic elevation can be respiratory, causing hypoxemia and diminishing the relation of ventilation and perfusion. Other consequences can be digestive, with a rise of the abdominal organs, resulting in rare cases like Chilaiditi syndrome4–6 for the left side and gastroesophageal reflux for the right. Diaphragmatic plication is a corrective surgery, from a functional and morphological point of view.
The procedure can be performed by laparoscopic or thoracoscopic approach. Huttl et al.7 recently described the superior benefits of laparoscopy in comparison to the thoracoscopic approach.8 Our patient improved dramatically in our clinic according to the SGRQ, thanks to the improved perfusion of the affected basal pulmonary section.
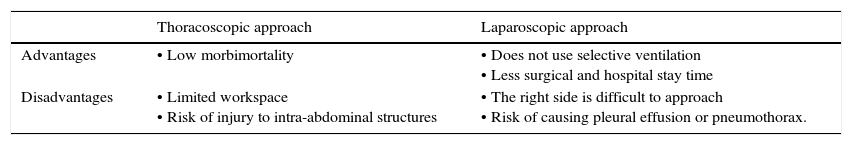
The majority of the comparative results of these procedures are similar. Others have demonstrated the usefulness of the thoracoscopic approach,9–11 while at the same time documenting that the disadvantages of this approach are selective intubation, reduced work space, an 8–10% risk of an abdominal organ injury because of no direct line of sight (5% with a laparoscopic approach) and greater postoperative pain (Table 1).
Advantages and disadvantages of the thoracoscopic and laparoscopic approaches to diaphragmatic plication.
| Thoracoscopic approach | Laparoscopic approach | |
|---|---|---|
| Advantages | • Low morbimortality | • Does not use selective ventilation • Less surgical and hospital stay time |
| Disadvantages | • Limited workspace • Risk of injury to intra-abdominal structures | • The right side is difficult to approach • Risk of causing pleural effusion or pneumothorax. |
There is an important relevance in this topic to include this management as part of the therapeutic arsenal, and having no standardized treatment and anecdotal case reports need more cases to define it.
The laparoscopic approach is definitively associated with reduced hospitalization time. More cases should be reported. This is the approach of choice in our institution.
Conflict of interestThe authors have no conflicts of interest to declare.