To evaluate the efficacy of local anesthesia and diagnostic or therapeutic Arthroscopy procedures and compare them with spinal anesthesia.
Material and methodsWe conducted a longitudinal, prospective, non-blind and analyst comparative clinical trial with two groups of 54 patients, aged 18–65 years. In the group assigned to local anesthesia and sedation, fentanyl, midazolam and propofol infusions were administered at the beginning of the surgery, the surgeon infiltrated ports and articular cavities with lidocaine and bupivacaine to provide postoperative analgesia. In the spinal anesthesia group, 7.5mg of simple bupivacaine was injected into the cerebro-spinal fluid (CSF). Clinical indicators were evaluated and were contrasted using inferential statistics.
ResultsThere was a significant difference in the following variables: time from the patient's entry to the beginning of the surgery (Local 39.19min SBA 55. 56min,), the group treated with SBA showing a statistically greater value (p<0.01), and length of stay in the recovery area (Local 102.33min SBA 143min), with the SBA group having the longest time (p<0.01).
ConclusionsValues were observed to be significantly lower in the time from the anesthetic procedure until the beginning of the surgery and the time of discharge from the recovery in the group treated with local anesthesia and sedation technique, with a maximum value of EVA 3. In conclusion, this technique is a good choice for this type of procedure, having a lesser total duration for the procedure and recovery.
Joints are innerved structures which transmit proprioceptive and nociceptive information, the main afferent pathways are A-delta fibers,which conduct nociceptive impulses, and group C nerve fibers which are slow-conduction nervous fibers, slower than group-A fibers. The receptors react to mechanical and surgical stimuli1; the synovial membrane is highly vascularized externally; in some places capillaries are deep and innervation scarce. Small diameter nerve fibers have been identified, and implicated mechanoreceptors have been described, important for the transmission of articular pain, with large diameter afferents and fast conduction. These afferent pathways are called silenced nociceptors, the cartilage is not innerved, the capsule has free Ruffini-type nerve endings and ligament innervation is through myelinated fibers, therefore the effect of anesthetics is direct, thus requiring small doses.2
The development of less invasive surgical techniques such as arthroscopy, and the improvement of postoperative analgesic control through local anesthetic techniques, have helped patients to reduce their hospital stay, along with the implementation of outpatient surgery and short hospital stay programs, which avoid unnecessary expenses.3 Intra-articular local anesthesia of the knee is a simple, safe technique well accepted by patients. It is linked to a low morbidity, reducing analgesic intake as well as reducing hospital stay, and thus a reduction in costs. Moreno-Regidor et al.3 conducted a study with 56 patients using local anesthesia and sedation. Their reports showed that it was necessary to reinforce the pain analgesics in portals or during knee valgus/varus stress maneuvers in 6 patients.
Subarachnoid spinal blocks and epidurals are the most commonly used methods in arthroscopic surgery for the knee. These techniques provide a sensation and motor block for the lower limb. Amongst the advantages of regional or general anesthesia are a greater convenience for the surgeon and greater analgesic levels; on the other hand, the disadvantages are linked fundamentally with risks for the patient and discomfort during recovery,4 i.e. low-back pain, urinary retention, and post-puncture headaches. These complications are not frequent, however, one must keep in mind the fact that there is a valid alternative: intra-articular local anesthesia.4
The use of local anesthesia and sedation compares favorably with other techniques: surgery time is not increased, the recovery time is significantly shortened and there is a high degree of satisfaction among patients using this technique.5
The first biopsy procedures using local anesthetics spread in the late 1960s. Mc Ginty and Matza developed an intra-articular knee anesthesia by adding bupivacaine to the washing fluid5; the first report by Williams using local anesthesia for a knee arthroscopy was in 1970, since then its use has increased and has been reported as effective.6
Local anesthesia for arthroscopic knee surgery is a well-documented procedure that offers many advantages over other types of anesthesia, there are only minor hemodynamic effects,7 it requires less surgical and recovery time, it shows good postoperative analgesia, a faster return to work or sports, less time needed for rehabilitation, is inexpensive and the results obtained are similar to other types of anesthesia. However, arthroscopic knee surgery is continuing to be performed more frequently with general or spinal block anesthesia. Previous reports such as that of Williams, et al. on the use of local anesthesia in knee arthroscopies, have emphasized the safety of this method and the low serum level of local anesthetics found during and after the procedure.8
A study by Moreno-Regidor3 concluded that although local anesthesia for the intra-articular knee is not the preferred treatment, it is a simple, safe technique, well accepted by patients, associated with low morbidity and increased time before the patient requests the first analgesic, reducing their consumption, and also reducing hospital stay and therefore lowering costs. That is why it is extremely interesting to contrast the use of spinal anesthesia (the widely-used technique) and local anesthesia, to determine their similarities and differences, in order to give the patient the best option.
Materials and methodsA comparative clinical, longitudinal, prospective and non-blind trial was conducted with 54 patients, randomly chosen, probabilistically simple and divided equally into two groups of 27 patients at the Department of Anesthesiology in the University Hospital “Dr. José Eleuterio González”. The patients were aged 18–65 years, with anesthetic risk ASA I or II, and scheduled for intra-articular treatment (diagnostic or therapeutic arthroscopy including procedures such as meniscectomy or meniscal repair, joint lavage and osteochondral lesions). The patients agreed to participate willingly (expressing their will by signing the informed consent), and we had the approval of the Institution's Ethics Committee.
We excluded patients allergic to amide-type local anesthetics (lidocaine, bupivacaine and ropivacaine), patients with combined treatments (such as arthroscopic debridement and osteotomy), or the presence of any acute inflammatory condition such as swelling, severe pain, synovitis and/or sepsis.
In the preoperative period, patients were dosed with 50mg of ranitidine intravenously (IV), metoclopramide 10mg (IV), midazolam 0.04mg/kg (IV), and a single dose of crystalloid at 10mL/kg. After the pre-anesthetic medication, patients were taken to the operating room where they were placed supine, underwent type 1 monitoring (electrocardiography, pulse oximetry and noninvasive blood pressure), were administered oxygen at 4–5L/min via face mask without a reservoir, and initial vital signs were recorded.
For the patients randomly assigned to local anesthesia and sedation, 100mcg of fentanyl was also administered and a propofol infusion was started at 1mg/kg (IV) for pervasiveness, and 0.01–0.05mg/kg/min (IV) of sodium chloride at 0.9% (200mg in a 250mL solution) for maintenance before port infiltration. At the start of the surgical procedure, the surgeon (the teacher assigned for the arthroscopic knee operation) infiltrated the two ports with 6 cc of lidocaine, and subsequently infiltrated the joint cavity with 20cc of simple lidocaine at 2%. Before starting the surgical procedure, the two ports were infiltrated with 6mL of bupivacaine at 0.5% for postoperative analgesia. For surgery irrigation, 500mg (25cc) of lidocaine were added per liter to the 3L bags so the local anesthetic concentration was 0.05%. At the end of the surgery 20cc of ropivacaine at 0.75% was injected into the cavity as an analgesic.
For the patients assigned to the spinal block group:
- A)
The patient was placed in lateral decubitus, with the iliac crests and shoulders accommodated perpendicularly to the bed. For the placement of spinal block, the midline was approached, which had been made by the anesthesiologist appointed in the operating room in question. After asepsis and antisepsis of the lumbar region and the selected space, L2–L3 or L3–L4, the skin was infiltrated with 2mL of lidocaine, infiltrating with a simple number 25 hypodermic needle; A Withacre short number 25 needle was used, finding the subarachnoid space.
- B)
We injected 7.5mg of plain bupivacaine (1.5mL) into the cerebrospinal fluid (CSF).
- C)
Sensory block was evaluated using the hypodermic needle picket test bilaterally with an evaluated clavicular midline. Motor block was assessed with the Bromage scale.
All patients underwent a pre-anesthetic assessment, and their arrival time at the operating room was registered, after calculating their arrival at the operating room, the start of the surgical procedure and the duration of the surgical procedure were also recorded. We recorded the patients’ hemodynamic parameters during surgery, time spent in recovery to ambulation, intraoperative pain by visual analog pain scale or VAS, as well as initial and final level of sedation by RAMSAY scale in both groups. Data was analyzed using the IMB SPSS Statistics program, and we obtained the traditional descriptives and frequencies in both groups (for quantitative and qualitative variables, respectively), contrasting averages with the Student t-test and determining correlations (according to distribution) by Pearson's or Spearman'stests; all of the above to a reliability of 95%.
ResultsThere were 27 patients in the group with a subarachnoid block (SAB). Their average age was 40.81 years (±12.81), weight was 82.22kg (±21.13), height was 1.66 meters (±0.098), and their average BMI was 29.84 (±6.72). The averages treated with local anesthesia group (LOCAL) (N=27) were: age, 41.59 years (±13.33); weight, 76.96kg (±11.70); height, 1.69m (±0.079), and BMI, 27.04 (±3.60). To analyze the study groups’ behavior, a predominance of males in the two groups was observed, and meniscal injury was the main diagnosis observed in both groups.
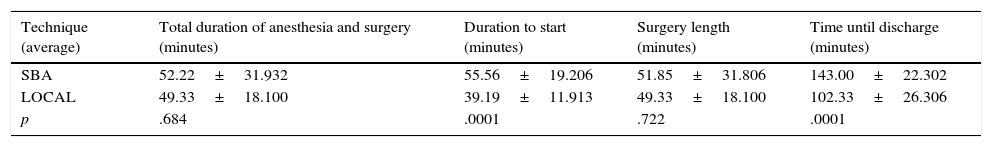
A significant difference was observed in the following variables: duration from admission of the patient to the room to the start of surgery, with the value of the SBA group being statistically higher (p=<0.01), and length of stay in the recovery area, in which the SBA group was also higher (p≤0.01), as shown in Tables 1 and 2.
Descriptive analysis of times.
| Technique (average) | Total duration of anesthesia and surgery (minutes) | Duration to start (minutes) | Surgery length (minutes) | Time until discharge (minutes) |
|---|---|---|---|---|
| SBA | 52.22±31.932 | 55.56±19.206 | 51.85±31.806 | 143.00±22.302 |
| LOCAL | 49.33±18.100 | 39.19±11.913 | 49.33±18.100 | 102.33±26.306 |
| p | .684 | .0001 | .722 | .0001 |
N=54 patients (SBA 27 patients, local 27 patients)/Source: Medical history and standardized instruments.
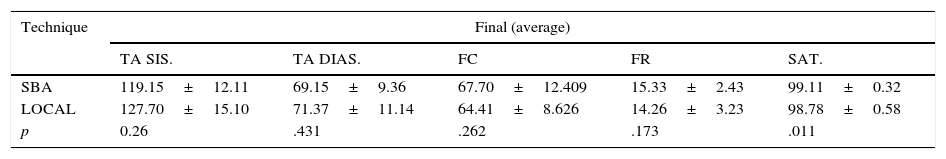
Descriptive analysis of clinical indicators.
| Technique | Final (average) | ||||
|---|---|---|---|---|---|
| TA SIS. | TA DIAS. | FC | FR | SAT. | |
| SBA | 119.15±12.11 | 69.15±9.36 | 67.70±12.409 | 15.33±2.43 | 99.11±0.32 |
| LOCAL | 127.70±15.10 | 71.37±11.14 | 64.41±8.626 | 14.26±3.23 | 98.78±0.58 |
| p | 0.26 | .431 | .262 | .173 | .011 |
N=54 patients (SBA 27 patients, Local 27 patients)/Source: Medical history and standardized instruments.
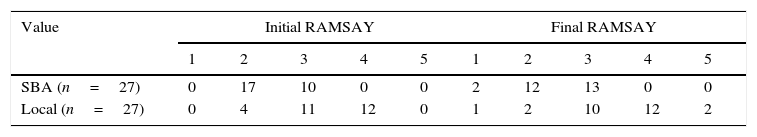
We evaluated the trans-anesthetic sedation with the RAMSAY scale (1=agitated patient, anxious or restless/5=slept in response only to pain. The distribution is shown in Table 3), in which, during the initial assessment, 100% of the SBA group were found to be between 2–3 scale values and 92.5% were in the same range during the final evaluation. In the local anesthetic and sedation group, 85.1% of patients were in the 3–4 range on the scale, and 81.4% remained in this range at the end of the procedure. These results can be explained because the SBA group patients only received an initial anxiolytic dose of midazolam at 0.04mg/kg (IV).
The trans-operative visual analog pain scale (VAS) in the local group showed a maximum recorded of 3 and an average of 0.41 (±0.88) while no patient in the SBA group reported pain (VAS=0).
Finally we observed a statistical correlation between the local group with the value of time to discharge (r=−0.648 and p≤0.0001); we found no statistically significant correlation between the two groups in the rest of the evaluated variables (hemodynamics) (p>0.01) as shown in Table 2.
No patient in the SBA group developed headache postpuncture and none of the two groups’ conversion to general anesthesia was required due to an insufficient anesthetic level.
DiscussionThe anesthetic methods used to perform arthroscopic knee surgery are the general regional peripheral anesthesia (inhaled and/or intravenous), neuraxial regional blockade, and local anesthesia. Each has advantages and disadvantages, as reported in the literature. Mondino, in his study of local anesthesia and sedation, reports a 1.6% failure rate in which conversion to balanced general anesthesiawas required in a series of 98 patients.5
To improve patient care and reduce surgical time and expenses, we attempt to show in our study that the use of local anesthesia and sedation is safe and effective in arthroscopic knee surgery, which was reflected in the results, and that a significant difference between the duration until the start of surgery was observed, with a statistically higher value in the SBA group. It was noted that time until discharge was higher in the SBA group (43min) and the maximum value recorded by the VAS in local anesthesia and sedation group was 3 at most, with 0 being the most frequent.
For carrying out the procedure under local anesthesia and sedation, we used intra-articular lidocaine at 2% as a local anesthetic, to have a more rapid onset of action5,9 allowing a local to block it immediately, and an early onset of surgery with optimum anesthetic levels, avoiding unnecessary delays during surgery. We also applied ropivacaine at 0.75% as a postoperative analgesic.
Maldini et al. reported a 96.6% success rate using local anesthesia and a propofol infusion, evaluating absence of pain, movement, and the patient referring to pain during the procedure.10 In our study, no patient required conversion to general anesthesia using our local and sedation technique.
Takahashi et al.11 evaluated pain during 63 cases of arthroscopic knee surgery with local anesthesia and found that this technique provides good pain control. He also concluded that intra-articular injection of lidocaine was the most severe pain encountered during the procedure. On the other hand, Ben-David et al.12, in a study analyzing spinal anesthesia for knee arthroscopy, was not able to achieve non-surgical anesthesia in four of his 15 patients using 5mg of bupivacaine, but there were no failures in doses of 7.5mg and above. In a subsequent study by the same author, the failure occurred in six of 25 patients who received only 5mg of bupivacaine, but in none of the 25 patients who received 10 mcg of fentanyl with the same dose of bupivacaine. In our group, we used the SBA technique with 7.5mg of bupivacaine at 0.5% (1.5cc), reaching an appropriate surgical level (T 10), and reporting a VAS of 0 in the 27 patients in the group.
In young patients, it is recommended to avoid dual punctures to avoid post spinal headaches. Researchers have shown that using small gauge needles with specially designed tips can bring down PSH (Post Spinal tap Headaches) to figures near zero.
Reina et al.13 state in their study that Whitacre 25 needles leave a dual hole by separation and disruption of the collagen fibers with an inflammatory component. These authors describe an edema caused by this inflammatory response, which is responsible for the closure of the dural hole, and would clinically lower PSH incidence and prevent further loss of spinal fluid into the epidural space. That is why, of the 27 patients in the SBA group that used Whitacre 25 needles, no post puncture headaches were reported.
Today, a significant number of surgical procedures are outpatient, and arthroscopic surgery has been a leader in this field. Local anesthesia for arthroscopic knee surgery is a well-documented procedure that offers many advantages over other types of anesthesia. It has less surgical and recovery time, only minor complications, good postoperative analgesia, a faster return to work or sports, less time needed for rehabilitation, is also low cost and the results obtained are similar to that of other types of anesthesia in safety and effectiveness, as we confirm in our study.
We do not recommend local anesthesia in cases that require a synovectomy by arthroscopy or cases who are thinking of performing a cruciate ligament plasty, due to the duration of the procedure and greater intra-articular bleeding than a simple arthroscopy. It is necessary to consider that it is not possible to use a tourniquet because the upper area of the member is not anesthetized.
Postsurgical analgesia of several hours’ duration, reported by the patients in our study, ensures an immediate start at postoperative rehabilitation without the impediment of pain. This obviously represents an advantage over general or neuraxial regional anesthesia, in which it is necessary to wait out the anesthetic recovery time. In the case of general anesthesia, the use of intravenous analgesia is required,including with opioids. With neuraxial regional anesthesia, postoperative analgesia does exist, but it is associated with motor deficits associated with this anesthetic technique, therefore immediate postoperative rehabilitation is impossible with both of these.
With the aim of reducing the duration of the surgical procedure, time spent in recovery, cost and complications, several authors, such as Moreno-Regidor,3 Mondino,5 and Maldini10 have researched the best anesthetic technique for performing arthroscopic outpatient procedures.
The technique of local anesthesia and sedation described is effective, practical and safe for diagnostic and therapeutic outpatient arthroscopic knee surgery. It decreases operating time and requires a shorter hospitalization and post-anesthetic recovery, with no adverse events reported in our study.
In addition, the use of local anesthesia and sedation can be an excellent option for patients who are contraindicated neuraxial blockades due to infection, neurological diseases, coagulopathy, heart disease or rejection by the patient.
Our study has several limitations, one of which could be the recent publications on the cytotoxicity of local anesthetics at a chondrogenic level, which was not part of our research objective. Studies have been conducted to determine the cytotoxicity of bupivacaine and ropivacaine, like that of Breu-Wolfgang et al.14 in which they argue that the mechanisms for this are not yet well elucidated, and prolonged exposure to high concentrations of local anesthetics through a continuous infusion pump could be involved in chondrocytes toxicity. Their results show no significant reduction in chondrocytes viability twenty four hours after treatment with ropivacaine, and an increase in the number of apoptotic cells 96h after exposure to the aforementioned local anesthetics used in the study.
Another study by Angele and Breu et al.15 mentioned that it is unknown whether the cytotoxicity of local anesthetics can act on chondrogenic differentiation of mesenchymal stem cells. The most important finding in this study was that necrosis and apoptosis in mesenchymal stem cells after exposure to local anesthetics was reduced by the production of cartilage tissue differentiation during chondrogenic differentiation.15 Ra Jeong Kimy et al.16 however, mention mechanisms involved in preventing this apoptosis with different antioxidants, such as the cyanide group of anthocyanins (pigment found in blackberries, raspberries, grapes, cherries, blueberries and fruits like apples and plums). They conclude that in their vitro study, these had cytoprotective effects in the techno fibroblasts of the rotator cuff exposed to amide-type local anesthetics.
Uncooperative patients, who have doubts regarding the anesthetic technique for fear of pain and the cost of the drugs, do not constitute a limitation in and of themselves, but should be considered when deciding on an anesthetic technique.
The use of local anesthesia for certain arthroscopic knee procedures is a useful tool, that we have demonstrated to reduce surgery startup times and postoperative stay time, and is comparable in pain, as measured by VAS, compared to patients in which the SBA was used.
FundingNo financial support was provided.
Conflict of interestThe authors have no conflicts of interest to declare.