Objective: To establish the prevalence of olfactory dysfunction in smoking and non-smoking students of our Faculty who attend the Department of Otolaryngology (ENT) of our Hospital. Materials and method: Students (smokers and non-smokers) that do and do not suffer from olfactory dysfunction. We applied a questionnaire and a pocket smell test for screening all of the students.
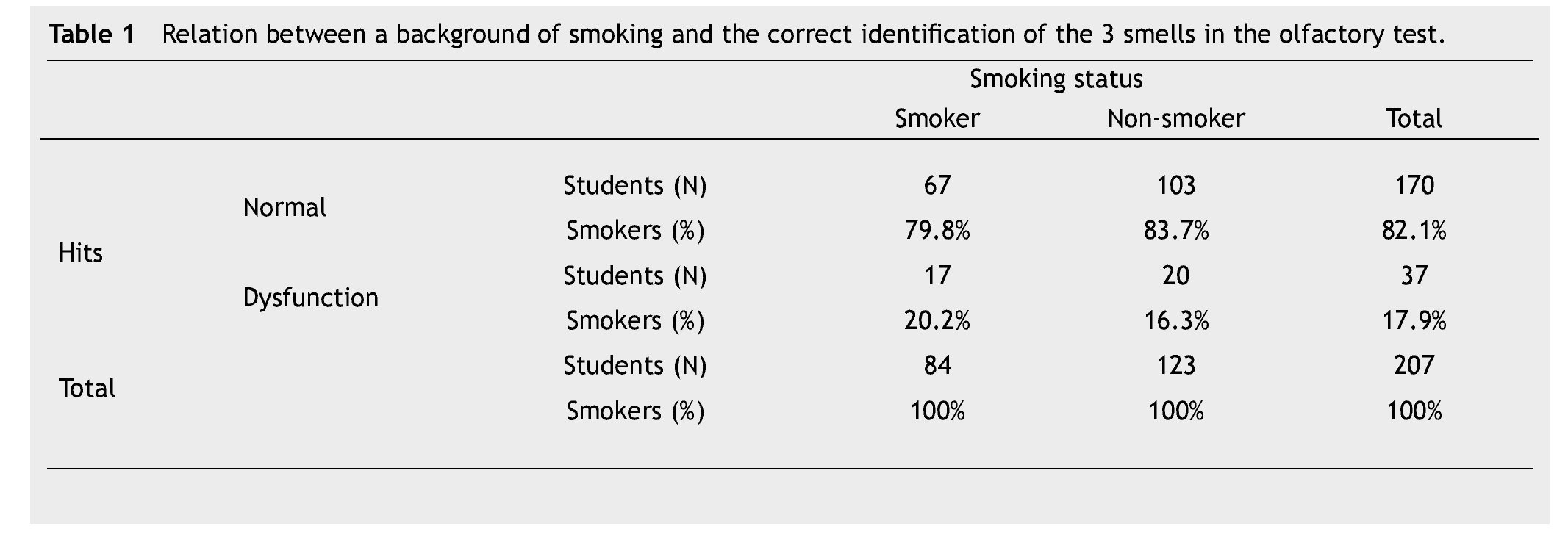
Results: We evaluated 207 students, between 18 and 30 years old; 50.7% (n=105) were women and 49.3% (n=102) were men. The smokers among them smoked up to 6 packs per year. One hundred twenty three students were non-smokers and 84 students were smokers. Of the 84 students who were smokers, 67 (79.7%) answered the Pocket Smell Test correctly (3/3) and 17
(20.2%) students had one or more errors. We had 123 non-smoker students and 103 (83.7%) students answered the Pocket Smell Test correctly and 20 (16.2%) answered with one or more errors. The prevalence of olfactory dysfunction in young smokers with a 95% confidence interval would be 32.8%.
Conclusions: This study informed us about olfactory dysfunctions in our student population and their smoking habits. We corroborate that the Pocket Smell Test is reliable with the questionnaire; nevertheless it is a screening test. We have a population of young people who smoke one cigarette per day and who didn't have a significant alteration in their ability of smell at the time of the study. This is consistent with medical literature. More studies should be conducted in order to expand this information.
Introduction
Smoking is one of the most harmful epidemics the world has seen. Over 6 million people die every year due to tobacco-consumption related diseases. In addition, smoking is a major cause of respiratory morbidity, including medical conditions which affect the nose.1 However, few studies have evaluated the relationship between tobacco smoke exposure and the generation of olfactory dysfunction.2
In the olfactory process there is a chemoreceptor system intimately related with emotions and the limbic system. This system regulates nutrition and the sense of well-being.3 Olfactory sensitivity depends on age and gender, among other factors. Women are superior in every aspect of the olfactory function.4 The 4 main causes of olfactory disorders are: trauma, viral infections, nasal causes (e.g., chronic rhinosinusitis and septal deviation) and those related to aging and neurological conditions.5,6
The objective evaluation of the sense of smell can be performed through odor recognition tests (ORT). In the United States, the most utilized test is the one created by the University of Pennsylvania (Smell Identification Test, Sensonics Inc. Haddon Heights, NJ, USA). This is a "scratch and sniff" test which includes 40 odors, and has been validated with a high reproducibility throughout different populations. Additionally, it is a cheap, easy to use test.7 The objective of this study was to establish the prevalence of olfactory dysfunction in medical students and to evaluate its association with tobacco consumption.
Materials and method
We randomly included 207 students from the Faculty of Medicine of the Autonomous University of Nuevo León (UANL), México, between 18 and 32 years of age. These students agreed to participate in the study during the course of their rotation in the Otorhinolaryngology Department of the "Dr. José Eleuterio González" University Hospital. Pregnant women were excluded.
We registered the project and it was approved by the institution's ethics committee. All the subjects were administered a questionnaire of 10 questions followed by a "scratch and smell" type test consisting of 3 items.
Those who denied having ever smoked answered only the questions related to the perception of their olfaction, and if they considered it to be diminished. Those students who were smokers were asked to specify the number of packs/ year and type of cigarettes that they usually smoked. Sample size was determined considering a finite population of 1,600 students annually, with a reliability of 95%, a maximum variability of smoking possibilities of 50% and a maximum accepted error of 10%.
The Smell Identification Test (Sensonics Inc. Haddon Heights, NJ, USA), is a 3-item "scratch and sniff" strip olfactory test. This test was utilized for screening all participants in the study. Each participant was given a brochure containing 3 areas with a different smell each. Participants scratched each of these areas with a pencil, placed it under their nose and marked the perceived smell out of 3 possible options.
We eliminated the cases where the students did not fully complete the questionnaire, or did not participate in the olfactory strip test.
We analyzed the data obtained using IBM SPSS® Statistics version 20.0.0. The results derived from the descriptive statistics analysis were expressed in percentages with the use of charts. We crossed variables performing the hypothesis test using chi2 test.
Results
Out of the 207 evaluated students, 50.7% were female, and 59% of the students denied being a smoker. From the 84 students who were smokers, 67 answered the Olfactory Strip Test correctly (3 out of 3), while 17 had 2 correct answers or less. On the other hand, in the non-smokers group, 103 students answered the test correctly (3 out of 3) and the remaining 20 obtained 2 correct answers or less (Table 1).
However, when we asked students if they could perceive any abnormality in their olfaction, 81.6% answered "no" and 18.4% answered "yes". In regard to whether or not they felt any discomfort in their olfaction, 106 students said "no", and 101 students said "yes"; 79 students did not attribute it to any cause, 36 students attributed such to allergies and 92 students believed it was caused by upper airway infections. Out of the total of the students, 76 claimed to smoke one cigarette a day, 8 students more than one cigarette a day and 123 students said they did not smoke any cigarettes a day. All the smokers smoked filtered cigarettes. The prevalence of young adults who smoke and have olfactory dysfunctions is 32.8% with a 95% confidence level.
Discussion
In the United States, olfactory dysfunction is a major health problem, with a reported prevalence of 24.5% in people older than 53 years and up to 62.5% in people older than 80.8
The etiology is multiple and the main causes include cranioencephalic trauma, upper airway infections and nasosinusal affection.9
Smoking contributes to the development of diverse disorders which affect the airways, oral cavity and other organs.10 However, the relationship between smoking and the olfactory function is poorly known.11 Bramerson studied 1,387 patients in Switzerland, finding a prevalence of olfactory dysfunction of 19.1% with a statistically significant relationship between age, gender and nasal polyposis with the loss of sense of smell without finding a relationship with smoking.12
We investigated the amount of tobacco consumed among a young population, and its relationship with olfactory dysfunction. From the 207 students, 81.6% did not show abnormalities in their olfaction during the questionnaire and after the test 82.1% showed results indicating normal olfaction. Out of the total of the population, 40.6% presented a positive smoking background a 20.2% abnormality in the tests within this group. Compared to 16.3% abnormality in the non-smokers, we observed that there was no significant difference between both groups. With these results, we find that our study is very similar to the data found in medical literature.
In addition, we found that upper airway infections are a frequent cause of olfactory dysfunction, in contrast to the findings by Bramerson where the predisposing factors were age, gender and nasal polyposis.
In spite of the use of olfactory strips, the study is considered to be scrutinizing; the results were properly correlated with the data found in the questionnaires, facilitating the approach to this special sense which is the sense of smell.
Conclusion
This study allowed us to learn more about our student population, as well as their smoking habits. We conclude that, just as reported in medical literature, we did not find a significant association between smoking and olfactory dysfunction. At the same time, we found that upper airway infections are a significant cause for such dysfunction.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
No financial support was provided.
Received: March 2013;
Accepted: January 2014
* Corresponding author:
Department of Otolaryngology and Head and Neck Surgery,
"Dr. José Eleuterio González" University Hospital.
Francisco I. Madero and Avenida Gonzalitos, Mitras Centro, Z.P.
64460, Monterrey, N. L., Mexico.
Telephone: (+52) (81) 8333 2917. Fax: (+52) (81) 8333 2917.
E-mail address: otoramiro1@hotmail.com (R. Santos-Lartigue).