Introducción: A pesar de los avances en el diagnóstico y tratamiento de la endocarditis infecciosa, esta todavía representa un gran problema para los cirujanos cardiacos. Otras enfermedades raramente exceden la mortalidad y la morbilidad asociada a endocarditis.
Objetivo: Evaluar el tratamiento quirúrgico de la endocarditis infecciosa y sus complicaciones, en el periodo comprendido del 2000 a 2010 en un Hospital Universitario.
Material y métodos: Estudio descriptivo y retrospectivo. Se incluyeron 62 pacientes operados por endocarditis infecciosa en el periodo de septiembre de 2000 a diciembre del 2010, en el cual se analizaron variables demográficas, operatorias y posoperatorias.
Resultados: La mortalidad hospitalaria fue del 16% y la tardía del 3%. El seguimiento fue en un rango de dos a 72 meses, no se presentaron casos de endocarditis recurrente y la sobrevida fue del 95% en los pacientes que se dieron de alta.
Conclusión: Un diagnóstico temprano y un tratamiento médico-quirúrgico oportuno antes de que se presenten complicaciones, son la clave para obtener mejor pronóstico en los pacientes con endocarditis infecciosa.
Introduction: Despite advances in diagnostic and treatment of infective endocarditis, it still represents one of the most difficult surgical dilemmas that a cardiac surgeon encounters. Other diseases rarely exceed the mortality and morbidity associated with endocarditis.
Objective: To evaluate the surgical management of infective endocarditis and its complications, from 2000-2010 in a Mexican tertiary care hospital
Material and methods: A retrospective case study. Details of 62 consecutive patients operated upon for infective endocarditis from September 2000 to December 2010 were analyzed.
Results: Ten (16%) patients died at the hospital. Follow-up was complete in 51 (82%) patients. There were two late deaths (3%), three and 22 months after hospital discharge. The follow-up extended from two to 72 months and the overall survival was 95% and no cases of recurrent endocarditis.
Conclusion: An early diagnosis and indication of surgical treatment prior to deterioration of the left ventricular function and generalized sepsis is the key to improve prognosis.
In memoriam of Felix Rosita Noriega MD, 1973-2010
Introduction
In the last few decades we have seen a steady improvement in the management strategies among patients with infective endocarditis (IE). This greatly in part to a more aggressive and prompt diagnosis, antibiotic therapy and surgical intervention. Nevertheless, despite all diagnostic and therapeutic advances, IE is still related to a high risk of mortality and morbidity and remains a challenge to cardiac surgeons. Other factors that influence outcome have been general preoperative conditions, postoperative management, timing of surgery, surgical techniques and follow-up.1,2 Valve replacement or repair surgery has shown to favorably influence patient outcome in native valve endocarditis (NVE), as well as in prosthetic valve endocarditis (PVE).3-5
The purpose of our study is to describe our experience in the last ten years (2000-2010) of surgical treatment of IE and review the literature.
Patients and methods
in a systematic retrospective review of clinical records, we analyzed data on 62 patients who underwent surgery for IE from September 2000 to December 2010. All patients were reviewed at a peer review conference before being accepted for surgery.
We based the diagnosis of IE on the modified Duke criteria. The bases of these criteria are pathological, clinical, and echocardiographic findings.6,7 The indications for surgery in native and prosthetic valve IE were categorized into three groups according to the clinical consequence of IE: a) hemodynamic instability b) sepsis and c) embolic events.
We reviewed hospital records for patient's demographic characteristics, preoperative status and co-morbidities, intraoperative variables, and postoperative course. Surgery was considered urgent if the patient was treated with IV antibiotics until completion of assessment. We define emergency surgery as the condition that prompts immediate surgery within 24 hours from diagnosis. The follow-up time was calculated as the period from diagnosis to last contact or death. For definitions of mortality and morbidity, standard guidelines were used.8 An early event is referred to any event within the first 30 postoperative days or during the entire hospital stay.
Operative management
The surgery used in all patients was a standard cardiopulmonary bypass technique with mild to moderate hypothermia (28-32°C). Myocardial protection was achieved with anterograde and retrograde cold blood cardioplegia and hot shoot terminal. The surgical protocol for treatment was based on elimination of infection foci and correcting the hemodynamic derangement. If the infection was limited to the leaflets of the valve, and there were no indications for valve repair, simple valve replacement using monofilament sutures reinforced with pledgets, only in cases of annular fragility, was the most common surgical procedure. The decision regarding the type of valve used was based on indications such as patient's age and compliance with anticoagulation administration and monitoring, and presence of contra-indications to anticoagulant therapy. If the infection had extended into the annulus and adjoining structures, it was repaired with either fresh autologous pericardium or glutaraldehyde-fixed bovine pericardium.
Patients received intravenous antibiotic therapy for a total six weeks or in selected cases more time. No patient was kept on antibiotics permanently.
Results
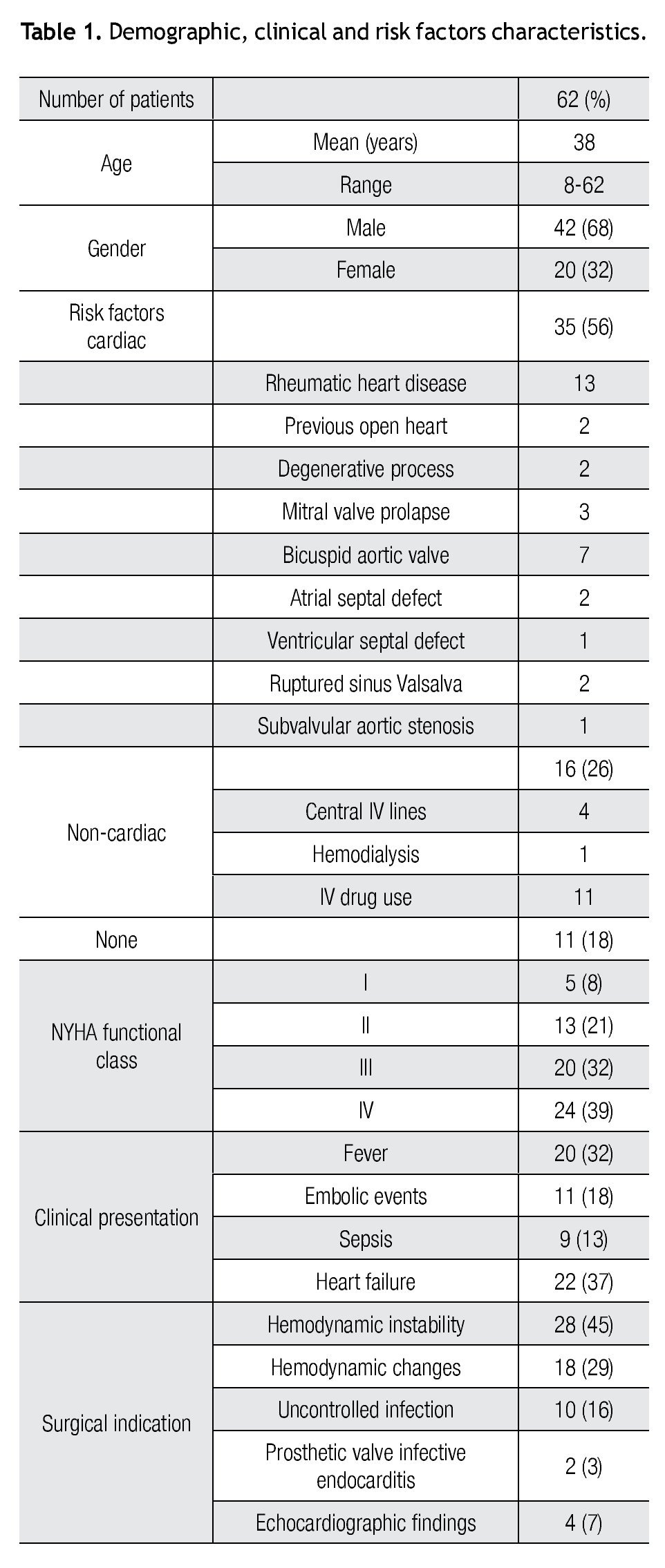
Demographic, clinical and risk factors characteristics
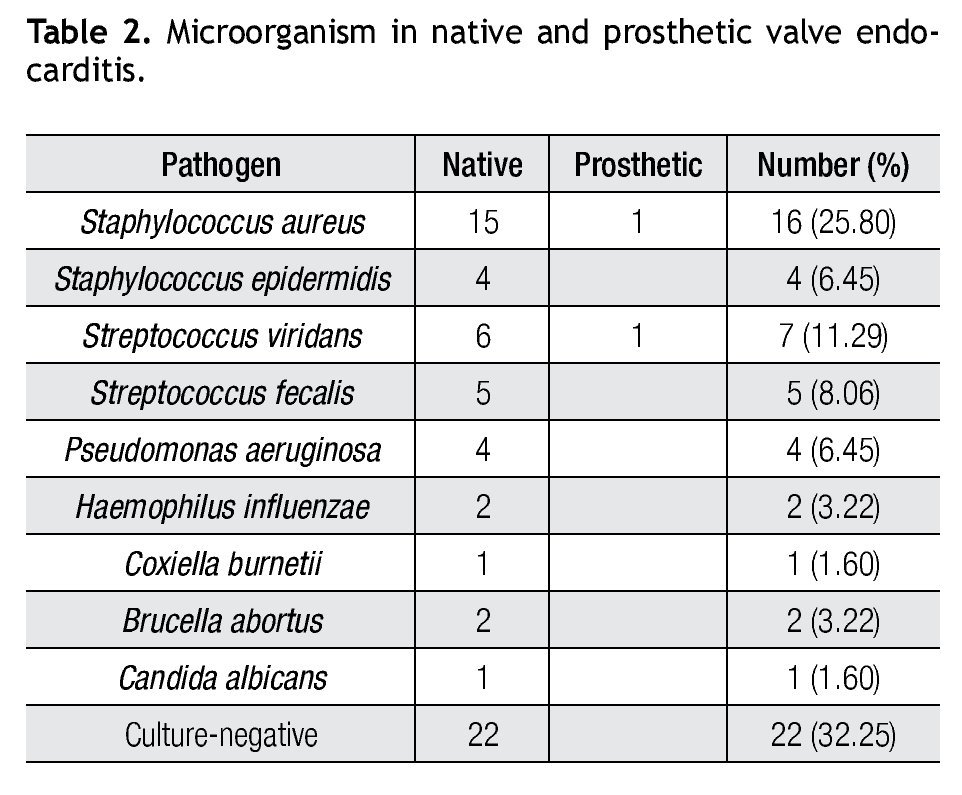
Demographic, clinical and risk factors characteristics are summarized in Table 1. Sixty-two patients enrolled in the study. Patient's mean age was 38 years, ranging from 8-62 years. There was only one pediatric patient. According to the New York Heart Association functional class classification, most of the patients were in class iii and IV (71%). Potential risk factors for the development of endocarditis varied widely, most patients had cardiac risks (56%), 26% had no cardiac risk factors and only 18% of the patients had no risk. For cardiac risk, rheumatic heart disease was the most frequent, and the bicuspid aortic was the most common among congenital cardiac diseases. In patients with no cardiac risk, the most common ones were IV drug abuse and the presence of a central IV lines.
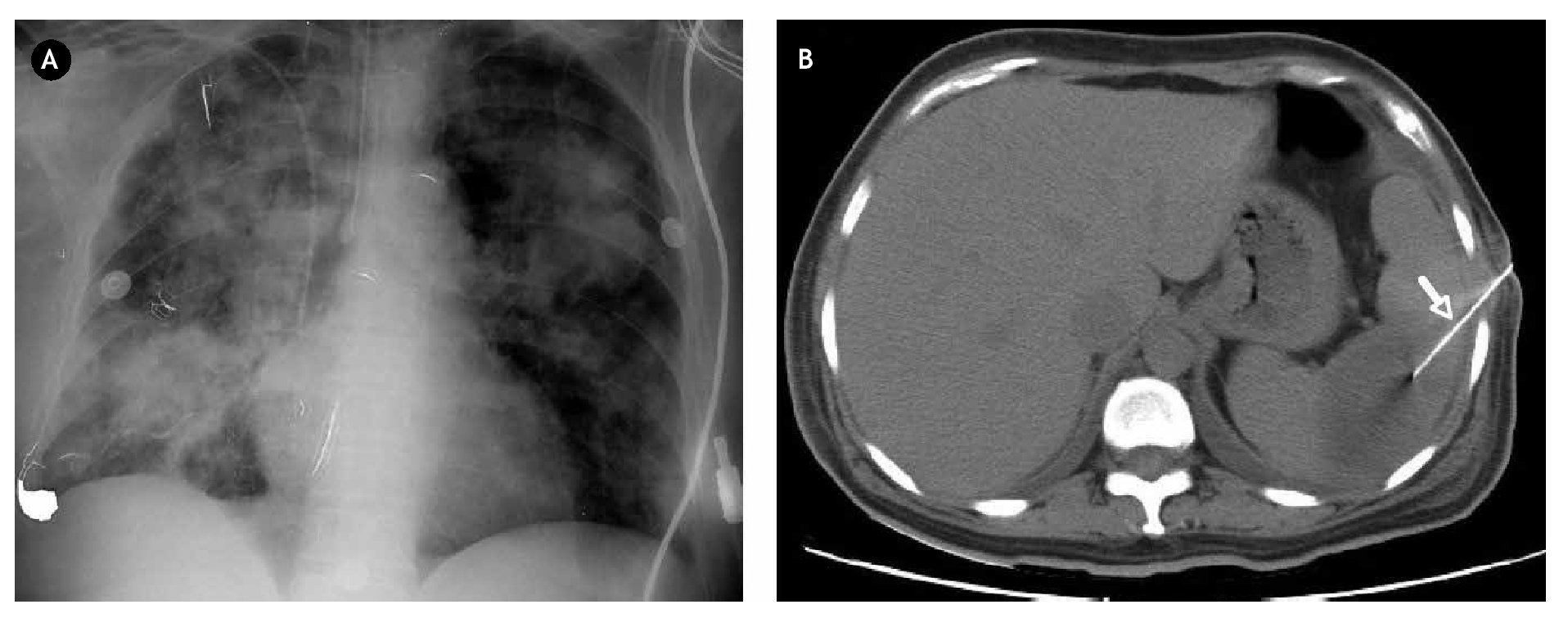
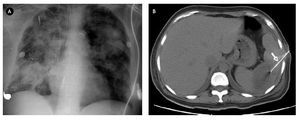
The most common clinical findings were preoperative signs and symptoms of heart failure (37%) and fever (32%). Embolic events were present in eleven patients (brain four, spleen five, kidney and lung one) (Figure 1).
Figure 1. A) Shows a chest X-ray of a 32-year-old male patient diagnosed with tricuspid infective endocarditis and multifocal pneumonia. B) Abdomen CT scan of a 57-year-old female with mitro-aortic infective endocarditis in which a splenic abscess was identified. She underwent fine needle aspiration/drainage (arrow).
All patients underwent at least one preoperative echocardiographic evaluation. A transthoracic echocardiography was performed in all the patients and a trans-esophageal echocardiography in 22 patients.
Echocardiographic findings were acute valve incompetence, evidence of vegetation (most common), abscess, and paravalvular leak. Their complementary studies included computerized tomography of the brain in five patients, magnetic resonance in two patients and computerized tomography of the abdomen in others six patients. No patient required cine coronary angiography.
Indications for surgery were mainly because of hemodynamic instability and hemodynamic changes (74%). The reasons for surgery for the rest of the patients were uncontrolled infection (16%), echocardiographic findings (7%) and PVE (3%).
Site involvement valve and microbiologic study
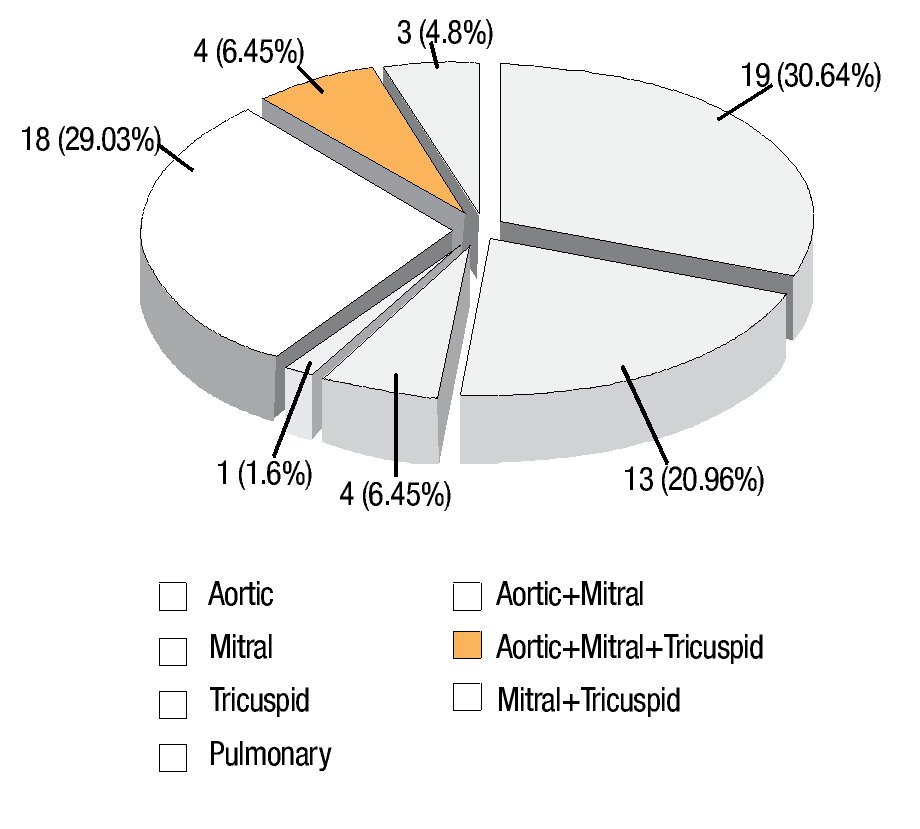
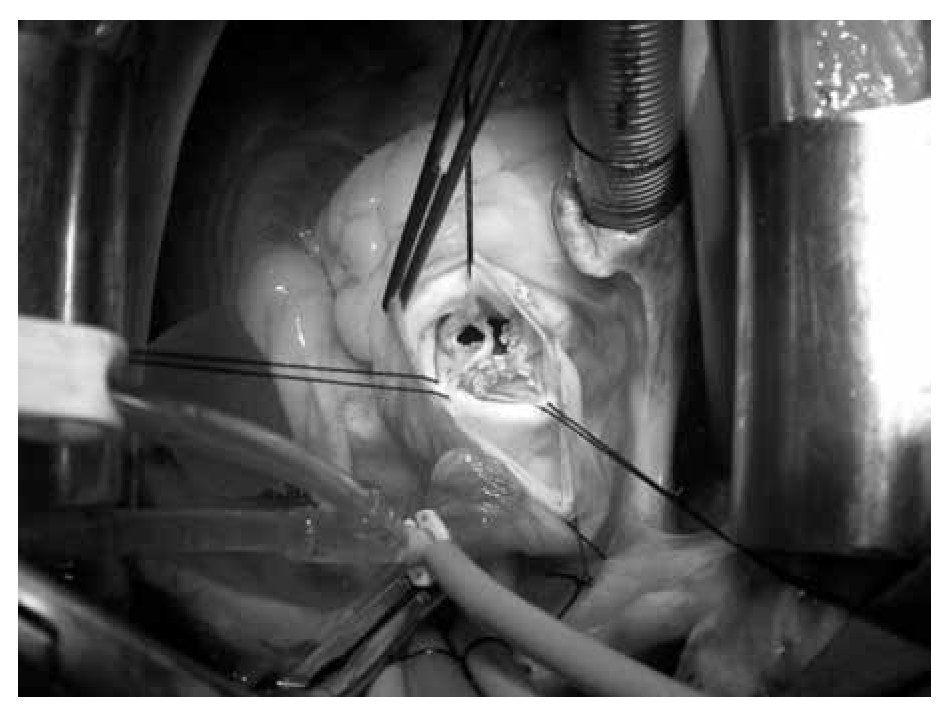
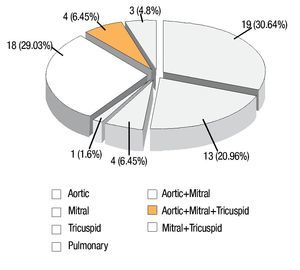
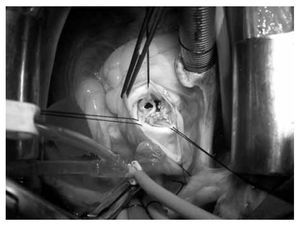
The site of involvement was determined by echocardiography and confirmed at surgery (Figure 2). The infective process involved the native valve in 60 patients (97%) and prosthetic valves in two patients (3%). Left heart valvular endocarditis predominated in the study population. From these, the aortic valve was the most commonly affected (30.64%), alone or combined with mitral and tricuspid valves (35%) (Figure 3). In the right side there were only four patients (6.45%) with tricuspid involvement (Figure 4), and one in the pulmonary valve (1.6%). Prosthetic valve endocarditis involved only two patients, own in the aortic valve (15 days after aortic valve replacement) and one in the mitral valve (six months after mitral valve replacement).
Figure 2. Sites of valve involvement in 62 patients with infective endocarditis.
Figure 3. Endocarditis in the aortic valve in a 37-year-old patients without cardiac risk factors.
Figure 4. Tricuspid valve endocarditis and supurative pericarditis in a 24-year-old male patient IV drug user.
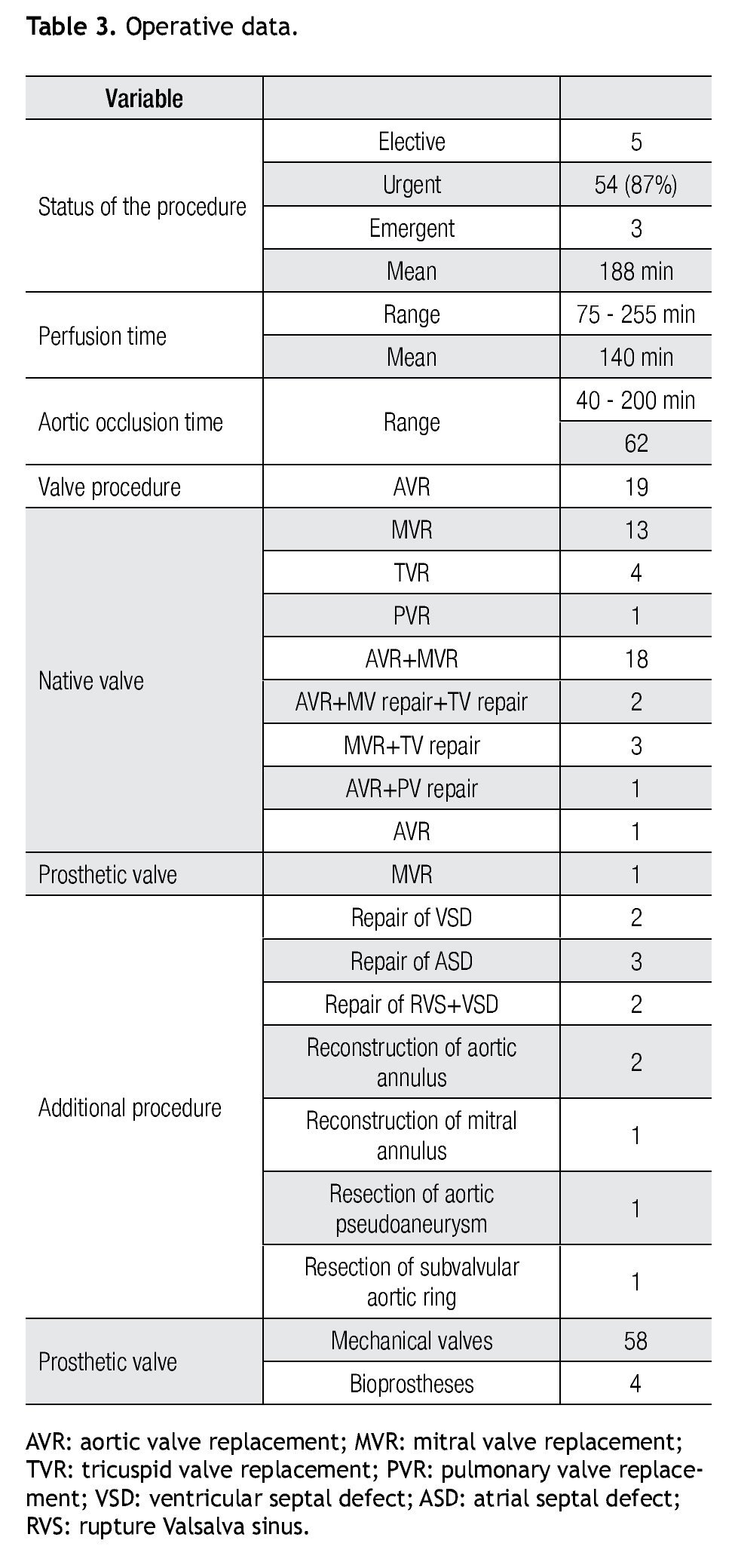
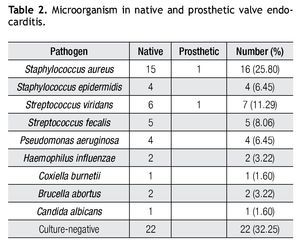
Of 62 patients, 40 (68%) had positive blood cultures; and 22 patients (32%) had negative blood cultures. Table 2 summarizes the blood culture results. As shown, Gram-positive cocci were the most common pathogens.
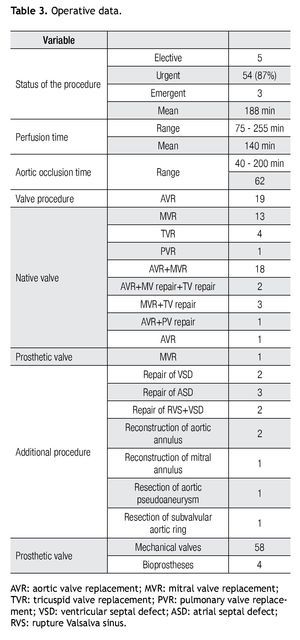
Operative data
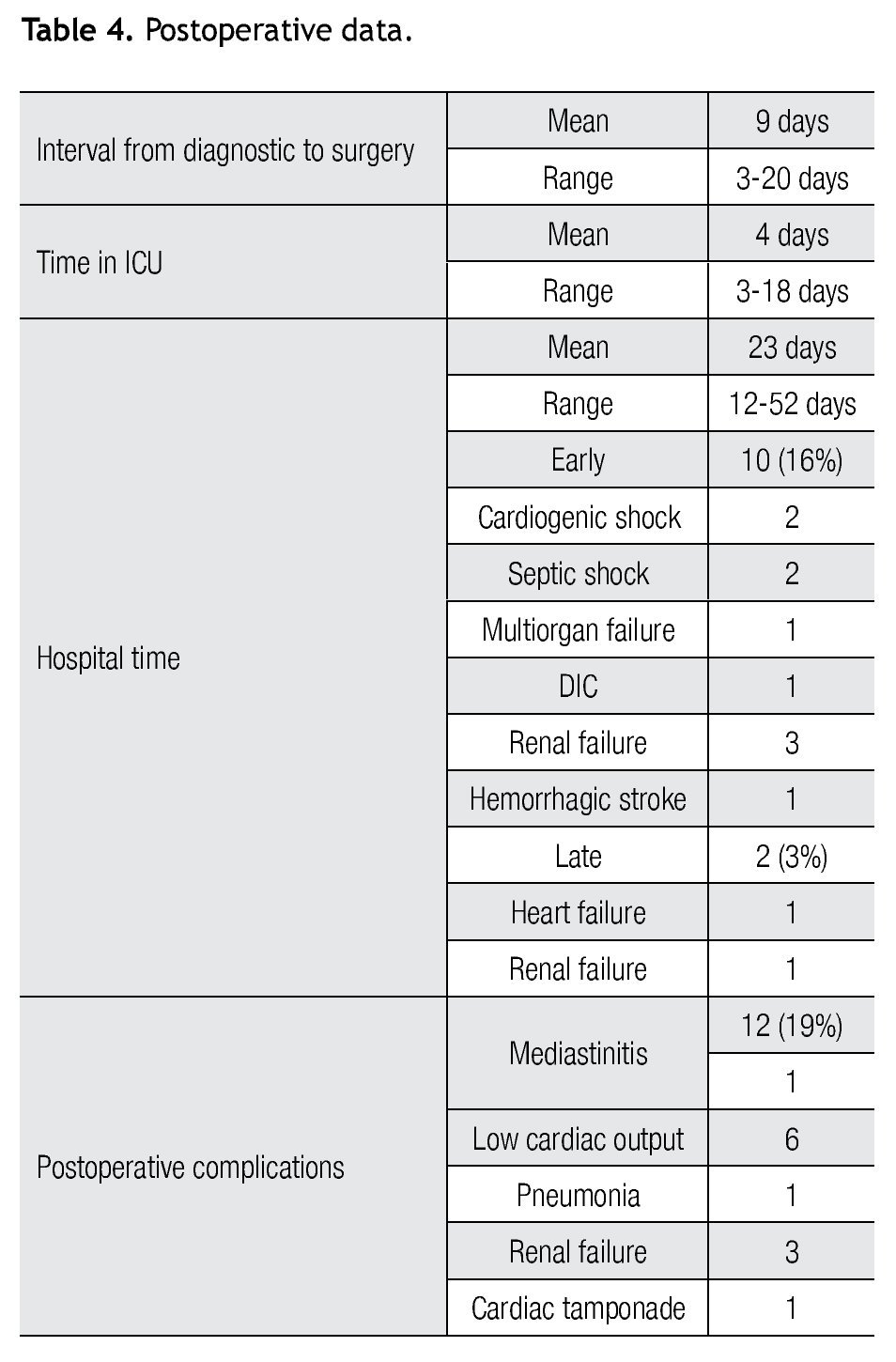
Most procedures were performed in an urgent basis (87%). The mean interval from diagnosis to surgery in patients who underwent surgery in an urgent basis was 12 ± 5 days (median six days).
The surgical procedure in 62 of the 62 patients included valve replacement or repair. In eleven patients (18%) surgery was related to a cardiac structure other than a valve. In six patients (9.67%), surgical treatment included a replacement of one valve and repair of at least another one. Non-cardiac procedures were performed in six patients before cardiac surgery for endocarditis; three percutaneous drainage of splenic abscess (SA) and in the other two, a splenectomy was performed, one before surgery and the other fifteen days after mitro-aortic valve replacement; and one patient was operated because of an intracerebral hemorrhage and scheduled for elective surgery three months later. The operative data are summarized in Table 3.
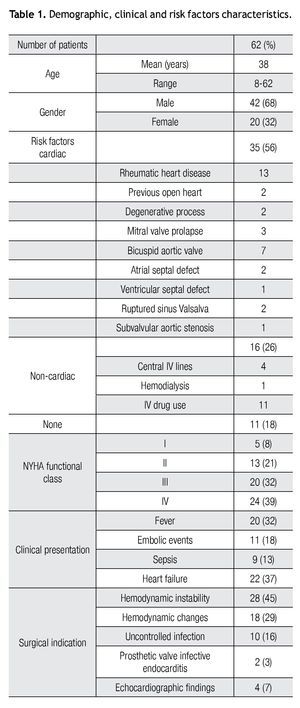
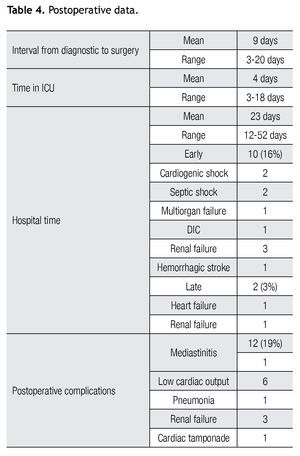
Postoperative data
The mean length of stay in the intensive care unit was four days (range 3-18 days) and the mean hospital stay was 23 ± 15 days (range 7-52 days). All patients were treated with intravenous antibiotics for a mean period of 42 days.
The hospital mortality was 16%, corresponding to 10 patients. Three patients were intravenous drug abusers and operated in an emergency basis. They had staphylococcal endocarditis, and two of them succumbed to sepsis and multiorgan failure during the first and third postoperative days and the other one due to a hemorrhagic stroke (this patient had a preoperative ischemic stroke, nevertheless the surgery was performed because of hemodynamic instability) during the fifth day. The other seven deaths were as follows: two patients developed a disseminated intravascular coagulation three days after surgery, three patients because of acute renal failure and the other two intraoperatively because of cardiogenic shock, not responding to neither medical therapy nor mechanical assistance.
Morbidity was 19% (12 patients). Six patients developed low cardiac output syndrome, two patients were re-operated, one because of cardiac tamponade and other due to mediastinitis. The postoperative data are shown in Table 4.
From the 52 patients discharged from the hospital, there were two late deaths (3.22%), one because of chronic kidney injury after three months and one more 22 months after due to heart failure. There was no recurrent endocarditis, episodes of thromboembolism, anticoagulant-related hemorrhage, valve thrombosis, or other complications during follow-up. The follow-up extended from two to 72 months and the overall survival was 78.57%.
Discussion
Since the first modern clinical description of IE by Osler,9 the profile of the disease has continuously evolved, like it has been described in different epidemiological studies,10,11 around the world. Unlike others countries, in México, the profile of IE has not changed too much in the last five decades.12 Although in México there is no national epidemiologic study about IE, the incidence of IE is calculated to be between one to six cases per 100 000 patient/year (personal communication from The National institute of Statistic, Geography and informatics, Mexico). In the author's institution the incidence of IE is six to 12 cases per year, and from these just 30% to 35% require surgical therapy. In our study, like in other reports,13,14 the incidence is higher in men than in women (3:1), but the average age group affected is in the third decade and generally in the majority of the reports, the age group most affected is after the fifties (mean 46-64 years).15 This difference could be due to the still high prevalence of rheumatic fever, the important presence of congenital cardiac diseases and the increasing group of intravenous drug user, as risk factors for IE in México.
Mitral valve prolapse, which has been described as an important predisposing factor in several reports,16,17 was present in just two cases in our study and it is of interest that there were three patients who developed endocarditis in association with an atrial septal defect, despite evidence that such a defect is associated with low o negligible risk. The overall prevalence of cardiac risk factors (56%), the increasing non cardiac risk factors (26%) and in 18% predisposing factors can not be identified, were comparable with others series.16-18
In the past, IE was classified as acute and subacute, but today, when such typical IE cases are less common, thanks to the use of antibiotics; the classification is based on the anatomical condition of the heart. IE is divided into NVE and PVE.19 In the current report, 96% of the cases were in NVE and from these 60% of the individuals (with the exception of intravenous drug addicts) present a preexisting heart lesion. PVE was present in just two patients and both cases had an early presentation. Our incidence of IE in patients with prosthetic valve is 1% per patient year, which is the same than other studies.20
The high incidence of mitral valve and more than one valve involvement in this report is in contrast to most other studies reporting a greater proportion of surgery involving just the aortic valve.21-23 The most common pattern of double valve infection was a jet lesion on the anterior mitral leaflet.
The clinical presentation of IE is frequently neglected and, when evident, normally it is the reflect of a complication. Clinical suspicion should be highly emphasized until diagnostic definition. Application of the criteria reported in the literature allows an approach with excellent sensitivity and specificity for the diagnosis of IE.24,25
Because echocardiography shows vegetations, abscesses and complications of IE, it represented the diagnostic imaging technique of choice in our cases. Despite the fact that transesophageal echocardiography (TEE) has significantly increased the sensitivity and has a lot of advantages,26,27 our strategy is to use transthoracic echocardiography (TTE) as our first choice except in PE, blood negative cultures, suspected paravalvular abscess among other selected cases, due to ease and cost-effectiveness analysis, which gives priority to TTE in our hospital.
A positive blood culture is important not only from the therapeutic viewpoint and from diagnosis, but for prognosis. In patients who had not previously taken antibiotics, positivity of blood cultures should be expected in more than 95%.28,29 However, the indiscriminate use of antibiotics in the initial stage of symptoms was the major cause of negative cultures (32%) in our report. The list of microorganism causing IE reported in our analysis included uncommon pathogens like B. abortus, and C. burnetti, but S. aureus was the most frequent causative organism followed by S. viridans.
The role of surgery in IE has been expanding since the first report of successful ventricular septal repair and removal of tricuspid vegetation in 1961 and the first successful valve replacement during active IE in 1965.30,31
Surgery is potentially lifesaving and is required in 25% to 50% of cases during acute infection and 20% to 40% during convalescence. Operative procedures are often technically difficult and associated with high risk, not least because patients are frequently extremely sick with multisystem disease. Nevertheless, indications for surgery are clear in many patients.
The indications for the surgical treatment of IE reported in the literature,32,33 are similar to those in our series and may be grouped as follows: hemodynamic instability, hemodynamic changes, uncontrolled infection, echocardiographic finding and prosthetic valve IE. In our case series hemodynamic instability and hemodynamic changes were the surgical indications in 74% of the cases and most patients were in NYHA functional classes iii and IV (71%). Although in our report eleven patients had embolic events, none of them was the main surgical indication.
The most common surgical procedure was valvular replacement with mechanical valves. Valvuloplasty was also possible with reconstruction techniques in selected cases. Homografts, considered the best choice in IE for most surgeons,34 but were not used in these cases due to availability reasons other than a surgical decision. Perivalvular involvement is a risk factor for recurrence of the disease.35 Despite extensive debridement, complex cases and use of autologous or bovine pericardium, no patient presented a relapse of IE. Danchin et al.36 and Renzulli et al.37 did not find differences between the patients with and without perivalvular reconstruction, in a 10-year follow-up, reported a 42% of relapse.
Splenic abscess is a well described but rare complication of IE. Clinically recognized SA occurred in 3% to 5% of cases of IE.38,39 The pathogenesis of SA in IE is likely a septic embolism that produces a splenic infarct, which in turn evolves into a frank abscess. Given the variable and often subtle clinical manifestations of SA, a high index of suspicion is necessary to make the diagnosis in a patient with IE. Computed tomography is the most sensitive and specific imaging technique to diagnose SA. The differentiation between common splenic infarcts and much rarer abscesses can be challenging. Percutaneous CT-guided needle aspiration may play a role in differentiating an infarct from abscess in dubious cases.40 In the largest reported series of patients with IE and SA, Robinson and colleagues38 identified 27 patients with SA among 564 (4.8%) patients diagnosed with IE during a 20-year period. Among the 10 patients treated without splenectomy (five of whom also had valve replacement), the mortality was 100%. In contrast in other report, 17 patients were treated with splenectomy and 14 (82%) survived. In a review of the literature of 37 patients with IE and SA, the mortality for 17 not treated with splenectomy was 100%, whereas 19 of 20 treated with splenectomy survived.39 These series provide compelling evidence that among patients withIE and SA, splenectomy is essential to eradicate the extracardiac focus of infection as a prerequisite to successful treatment of IE with either antibiotics alone or in conjunction with heart valve surgery. Currently percutaneous CT-guided drainage or aspiration of SA has been performed successfully, and this procedure may be an alternative to splenectomy. In this report, there were five patients with SA, three of them were treated uneventfully with percutaneous CT-guided needle aspiration, and the other two required a splenectomy. The survival rate of these patients was 100%.
Neurological events arise in 20% to 40% of patients with IE, mainly as a consequence of vegetative embolism,40,41 and are most common in those with S. aureus infection.42 The clinical spectrum of complications is wide and includes ischemic or hemorrhagic stroke, transient ischemic attack, silent cerebral embolism, symptomatic or asymptomatic mycotic aneurysm, cerebral abscess, meningitis, toxic encephalopathy, and seizure. All manifestations are associated with excess mortality.43 Most patients with a neurological complication have at least one other indication for cardiac surgery. Although inherent concerns exist about the role of surgery in these situations (fear of neurological deterioration or perioperative cerebral bleeding), these risks are low after a silent cerebral embolism or transient ischemic attack,44 and surgery can be performed without delay. In our study, four patients showed neurologic impairment before the surgery. One of them required neurosurgery and because he was hemodynamic stable and without complications, the cardiac surgery was postponed for three months with good results.
Overall surgical mortality in active IE is 6% to 25%, with long-term survival rates of approximately 70% in most series.44-54 In the past years, our in-hospital mortality was in average 30%, and in the present study the overall operative mortality is 16%. This decrease in mortality was due to early diagnosis, new antibiotic regimens, better timing of surgical intervention, adequate surgical therapy, improved management of complications and more experience.
The follow-up in our series was not to long (2-72 months). However, the survival of 78.5% and freedom from recurrence of endocarditis of 100% are quite satisfactory.
Conclusion
Surgery has an established role in the management of IE across a wide range of patients, a role that appears poised to increase as the complexity of patients with this difficult condition rises and the benefits of earlier surgery emerge. As large international research collaborations become established, the future may see a more robust evidence base to guide management strategy. Nevertheless, decision making in individual patients will remain difficult, with the best outcomes obtained as a result of expert multidisciplinary collaboration between the cardiologist, microbiologist, and cardiac surgeon. Only with such interaction will the questions of who and when seem easier.
Conflict of interest
The authors declare that there is no conflict of interest.
Financial disclosure
No financial support was received in relation to this article.
Corresponding author:
Felipe Gerardo Rendón Elías, MD.
Servicio de Cirugía Torácica y Cardiovascula,
Hospital Universitario "Dr. José Eleuterio González" Universidad Autónoma de Nuevo León,
Av. Madero y Gonzalitos s/n, C.P. 64460, Monterrey, N.L., México.
Teléfono: (+81) 834 67800, ext. 3334. Fax: (+81) 834 88305.
E-mail: drfrendon@gmail.com
Received: February 2012.
Accepted: October 2012