Introduction: The treatment for venous ulcers in most cases is unsatisfactory, with recurrences and poor healing.
Objective: To evaluate adjuvant therapy in the treatment of active venous ulcers.
Methods: We analyzed 20 patients with active venous ulcers attending the general Surgery out-patient clinic at the "Dr. José Eleuterio González" University Hospital from October 2012 to January 2013. They were randomly divided into 2 groups: group A (11 patients) underwent compression therapy and group B (9 patients) underwent compression therapy plus removal of the vein that gives terminal reflux to the ulcer, guided by ultrasound (microphlebectomy). Patients were evaluated weekly (8 weeks). At each assessment, photographs and lesion measurements were taken and pain was evaluated using the visual analog scale.
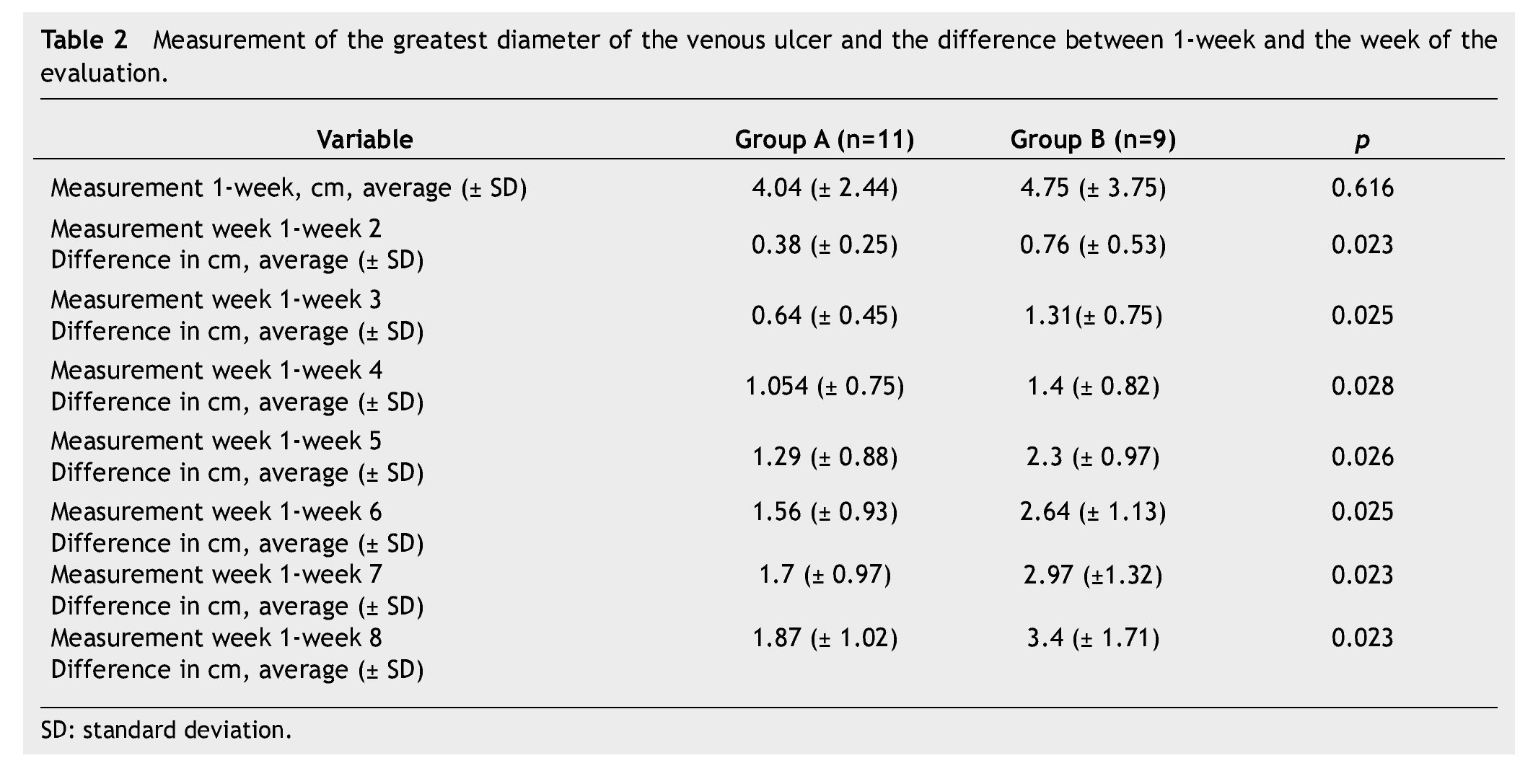
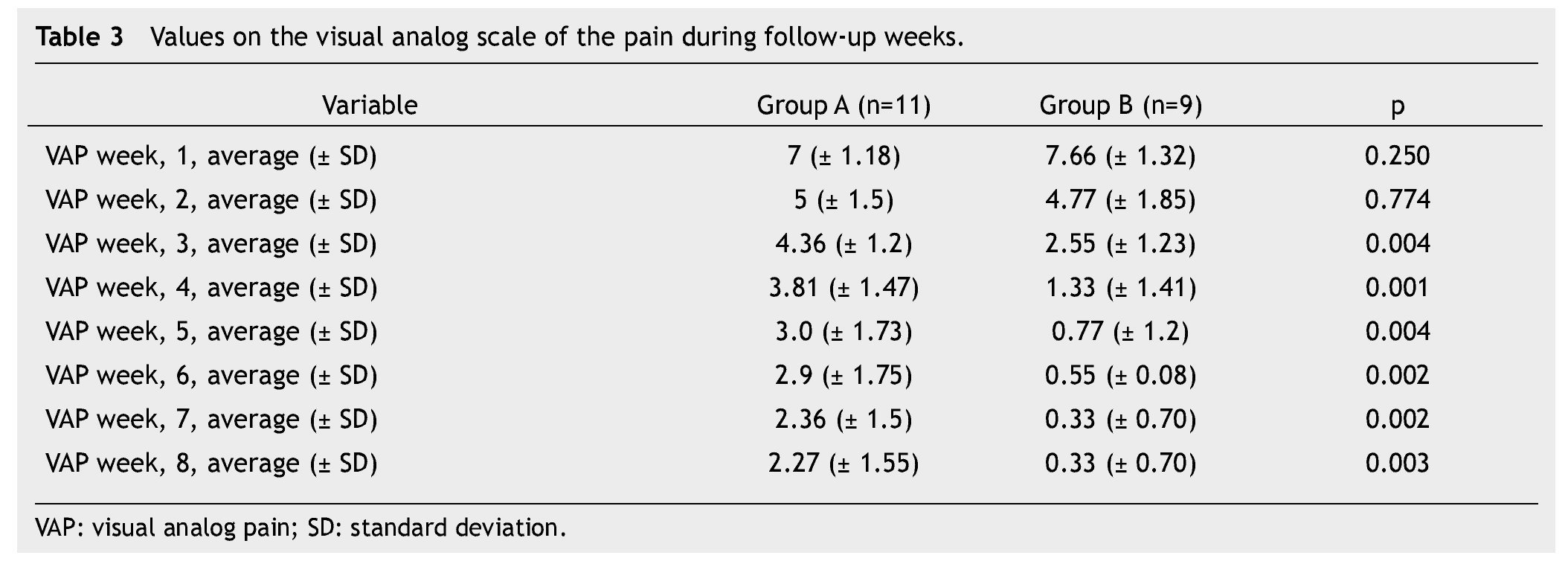
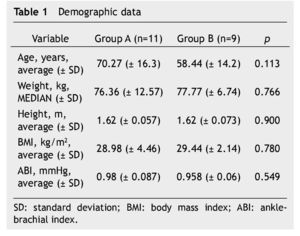
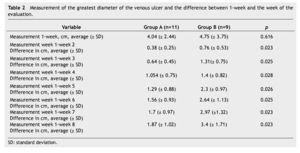
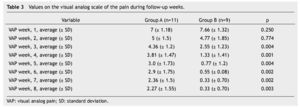
Results: No significant differences were found between the study groups in terms of age, weight, height, body mass index (BMI), ankle-brachial index, and baseline measurement of the ulcer (p>0.05). Group B showed a greater reduction in ulcer size and a statistically significant lower score on the visual analog pain scale (p<0.05) from the second and third week of treatment, respectively.
Conclusions: The results obtained in patients with surgical procedure (group B) are consistent with the reported efficacy of chronic venous ulcer treatment with saphenectomy (conventional surgery), the difference is that in this study we used a minimally invasive procedure (microphlebectomy).
Introduction
A venous ulcer is the most serious consequence of chronic venous insufficiency. This disease has been known for over 3500 years. Nowadays, it is a pathology which draws little attention, despite new findings regarding its pathogenesis and treatment. In our opinion, we should focus on its healing rather than on the cause of the problem. About 1% of the population has a history of Postphlebitic ulcers. This percentage increases to 4% in the population over 65.1 the
Bonn Vein Study included 3072 participants, finding changes in pigmentation or eczema in 2.9% and a postphlebitic ulcer in 0.7%.2 A multicenter study conducted in Poland with 40,085 participants found skin changes in 4.6% of the patients, a healed ulcer in 1% and active ulcers in 0.5%.7 Heit et al. found a venous ulcer incidence of 18 for every 100,000 people a year and a yearly Billion-dollar expenditure on public health.3
Current theories about the etiology of severe chronic venous insufficiency are related to chronic venous hypertension.4,5 When weakness develops in the walls of the veins, dilatation of the valve ring is produced, impeding valve coaptation.6 recent data indicates that venous hypertension causes extravasation of macromolecules and erythrocytes inside the interstitium.7,8 erythrocytes and protein interstitial degradation are a powerful leucocyte chemoattractant. This suggests a role in cytokines, demonstrated by the presence of beta growth factor, which may cause fibrosis by stimulation of the extracellular matrix, reducing oxygen and nutrient circulation thus resulting in changes in the color and consistency of the skin.5
Advanced isolated venous insufficiency includes a sensation of excessive weight on the legs as well as edema. Signs include a phlebostatic crown (spider-shaped outbreak consisting of small varicose intradermal veins on the medial aspect of the ankle and foot), and changes in skin such as lipodermatosclerosis, which in its chronic phase develops as shiny, hardened and pigmented skin.9,10 Ulcers have irregular edges with neo-epithelization with a pinkish base with granulation tissue, on occasions with a fibrin coating. Pulse palpation and the ankle-brachial index test are necessary in order to rule out an arterial insufficiency.11,12 the Doppler ultrasound is currently the gold standard in venous insufficiency diagnosis.13,14 The American Venous Forum classifies active venous ulcers as C6.15,16
Treatment includes general measures: patient education, weight loss, elevation of the extremity and exercise.17-20 Factors like immunosuppression, malnutrition, diabetes mellitus, arterial insufficiency, local infection, and cardiac insufficiency may affect ulcer healing. A compressive therapy is the base in venous ulcer treatment, and this has been validated in random studies.21
O'Meara et al. and Ukat et al., proved a statistically significant decrease in time in ulcer healing (p=0.005) with the use of multiple elastic bandages compared to the inelastic systems.22-24 Myers et al. found superficial venous insufficiency with Doppler ultrasound in 38% of the patients with venous ulcers, and a combination of superficial and deep venous insufficiency in 48% of the patients with ulcers.25 A study showed venous ulcer healing in 77% of the cases 12 months after superficial venous reflux surgical treatment.26
Bush included 14 patients with chronic venous ulcers (6 to 24 months) treated with compressive therapy. The patients were treated with the terminal interruption of reflux source technique guided by a Doppler ultrasound, which consisted of injecting sclerosant foam into the ulcers proximal veins, with an ulcer healing time of 6 to 8 weeks in 11 patients, with 5 years with no recurrences in 7 patients, 2 years with no recurrences in 4 patients, a year with no recurrences in 2 patients and recurrence in one of them.27
The objective of this study is to assess the clinical benefits in reducing the size and pain in active venous ulcers using terminal interruption of reflux source technique guided by ultrasound in the treatment of venous ulcers.
Materials and methods
We performed a prospective, comparative longitudinal study. A non-blind, experimental, controlled clinical trial.
Inclusion criteria: A C6 classification by The American Venous Forum (active venous ulcers), age of at least 18 years, venous insufficiency diagnosed by a Doppler ultrasound, BMI between 18.5 and 34.9, no local infection, a signed informed consent, having no previous venous surgery and an ankle-brachial index over 0.85.
We analyzed 20 patients with a diagnosed venous ulcer in their lower limbs, with a previously signed consent form, attending the general Surgery outpatient clinic at the "Dr. José Eleuterio González" University Hospital, and meeting the inclusion criteria, from October 2012 to January 2013. The patients were randomly divided into 2 groups: group A (control) with compression therapy and group B with surgical treatment in addition to compressive therapy (experimental). Patients were evaluated weekly (8 weeks). At each assessment, photographs and lesion measurements were taken and pain was evaluated using the visual analog scale. We indicated rest and elevation of lower extremities for 30 minutes in the morning and 30 minutes in the afternoon, as well as sleeping with the affected limb elevated. Patients were discharged on an outpatient basis with analgesic (paracetamol 500 mg orally every 8 hours) in case of pain, and treating the wound every 24 hours with a super-oxidized antiseptic solution (Microdacyn®), non-adherent dressings and mild compression elastic socks (20-30 mmHg).
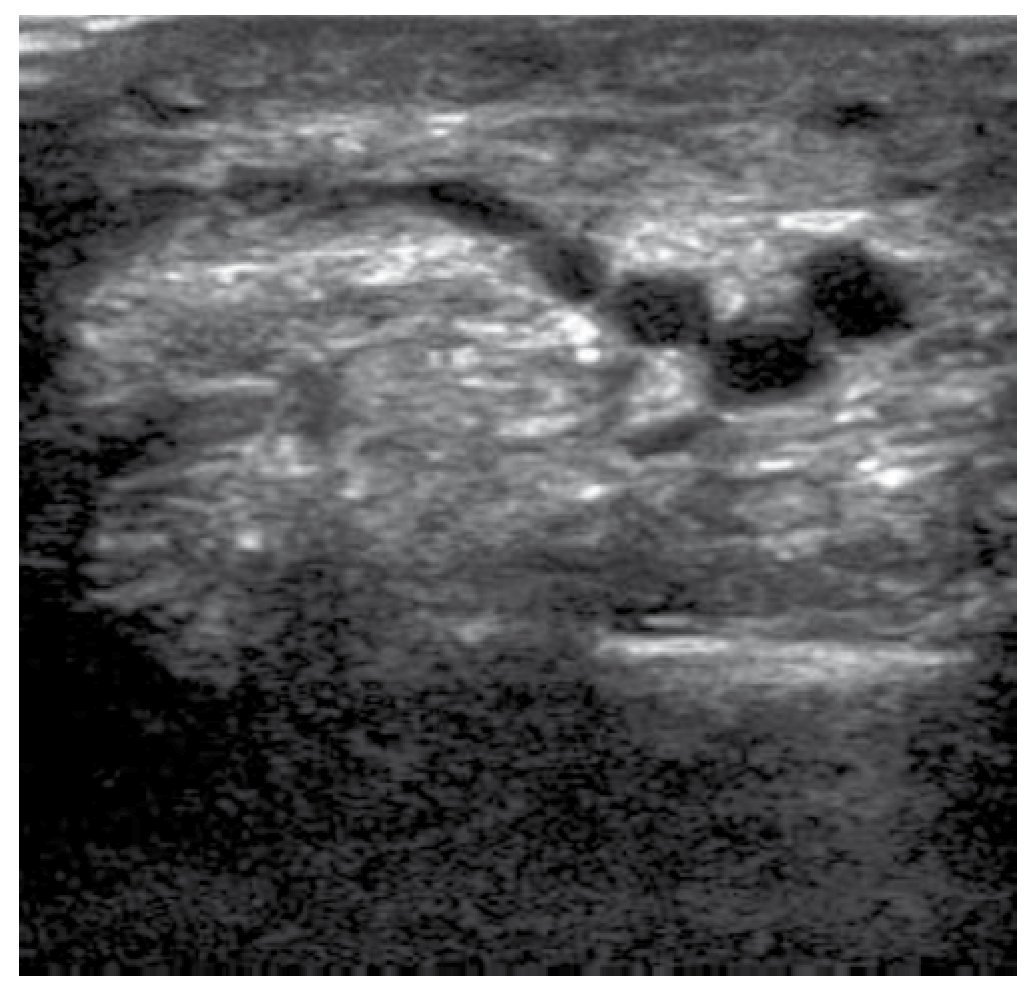
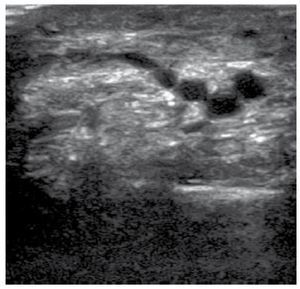
In group B, using an ultrasound with lineal transducer of 7.5 MHz, with the patient standing, the researcher looked for and marked the responsible vein(s) of the terminal blood reflux to the ulcer (Fig. 1). Once we identified the vein(s), we proceeded with: infiltration with local anesthesia (lidocaine 1%), a puncture with a Jelco® catheter #14 adjacent to the marked vein, dermis dissection and vein extraction with a hook (Fig. 2), avulsion of the vein with hemostat clamps (Fig. 3), compression in order to achieve hemostasis, application of a super-oxidized antiseptic solution (Microdacyn®), non-adherent dressings and mild compression elastic socks (20-30 mmHg).
Figure 1 echographic image showing the veins that give terminal reflux to the venous ulcer.
Figure 2 image showing the extraction with a hook of the vein with terminal reflux to the venous ulcer.
Figure 3 image showing the avulsion of the vein with terminal reflux to the venous ulcer with a hemostatic clamp.
Statistical analysis
The information was gathered in a database using excel®. We performed the Kolmogorov-Smirnov test to evaluate the variable distribution, and we determined that they all showed a normal distribution (gaussian). The other test used to compare both groups was the Student's t-test with a 95% confidence, and we considered it to be statistically significant p<0.05. We used the SPSS® Statistics version 20.0 (iBM Company). The study was approved by the institution's Committee of ethics.
Results
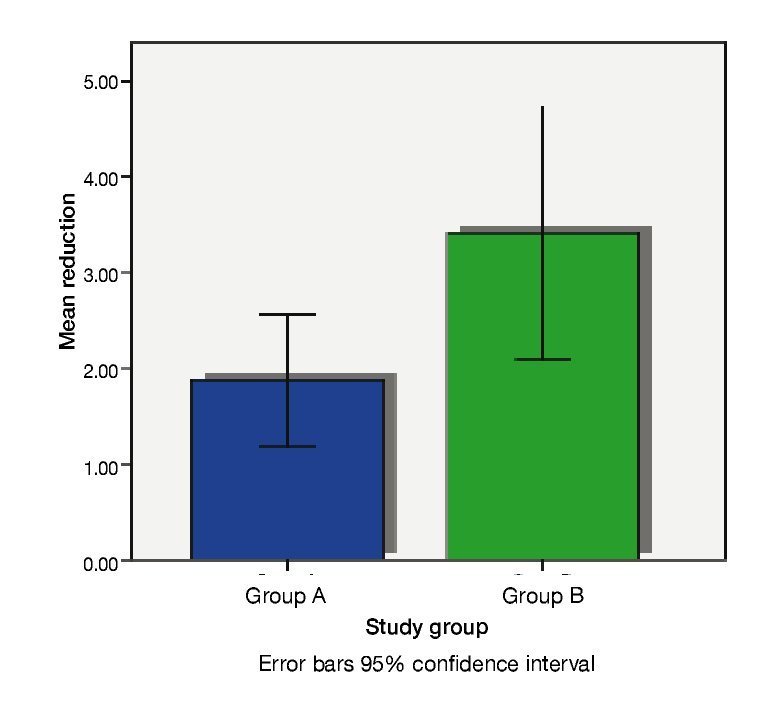
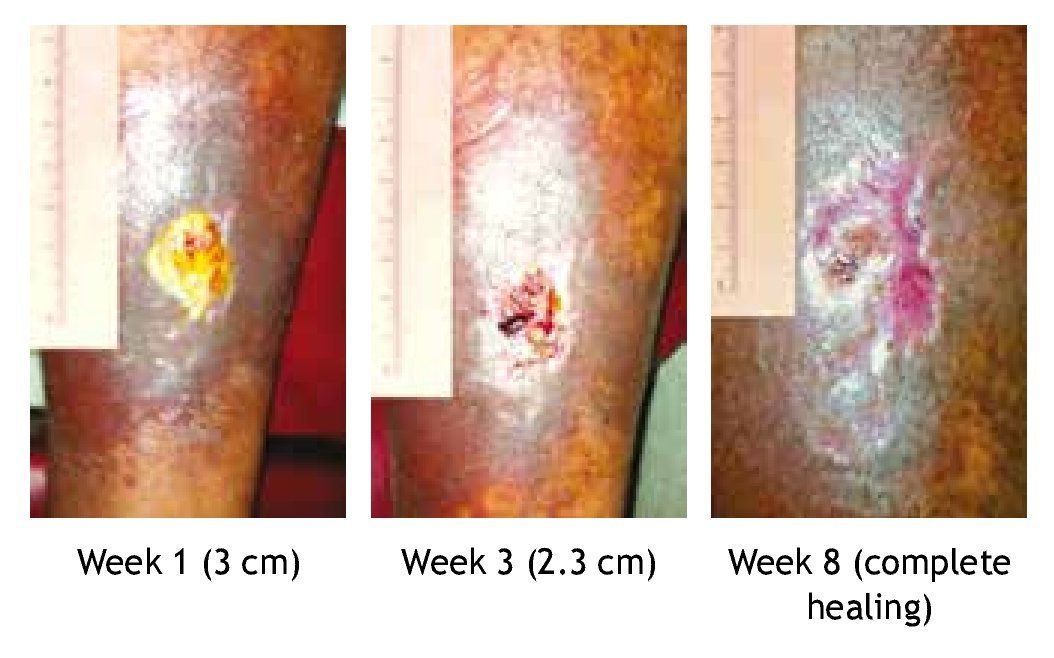
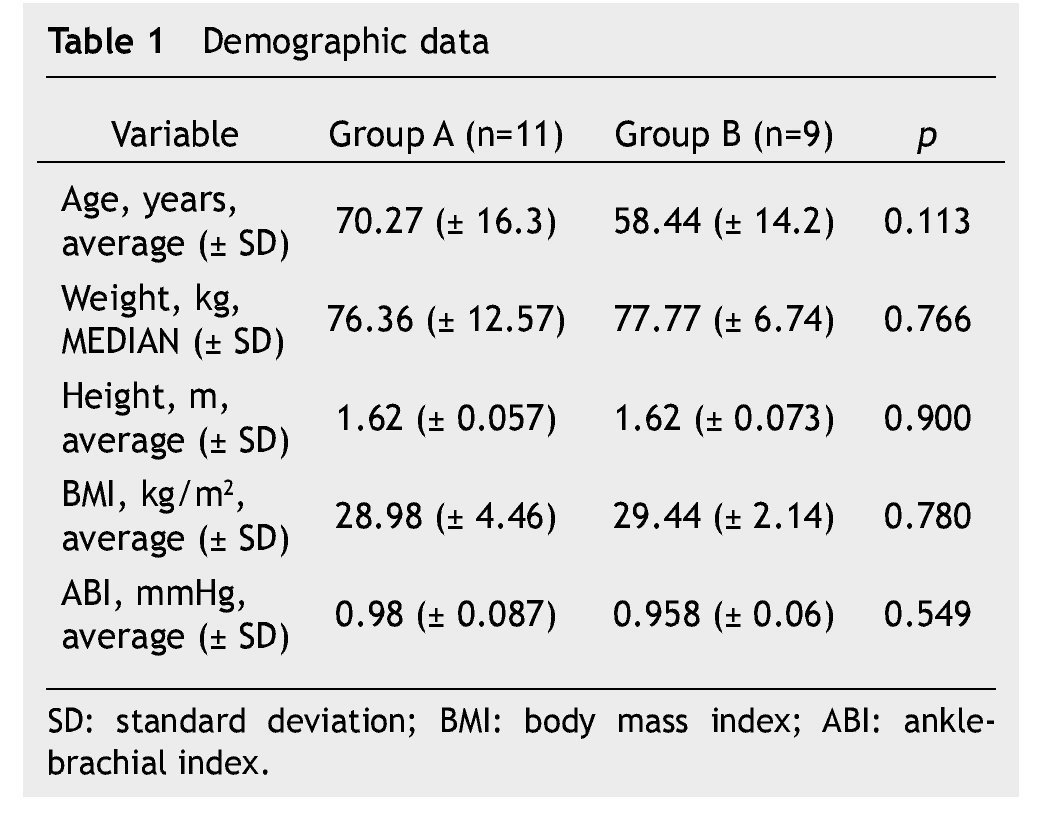
A total of 20 patients with active venous ulcers were included, 11 of them -9 female and 2 male- in group A (compressive therapy), and 9 of them -8 female and 1 male- in group B (surgical and compressive therapy). No significant differences were found between the study groups in terms of age, weight, height, BMI, ankle-brachial index, and baseline measurement of the ulcer (table 1). Venous ulcer mean diameter in week 1 was 4.04 cm (± 2.44) for group A and 4.75 cm (± 3.75) for group B with a p=0.616 (table 2). Group B showed a greater reduction in ulcer size and a statistically significant lower score on the visual analog pain scale compared to group A (p<0.05) with full healing (scarring) in 3 patients. This difference was significant from the second and third week of treatment, respectively (table 3).
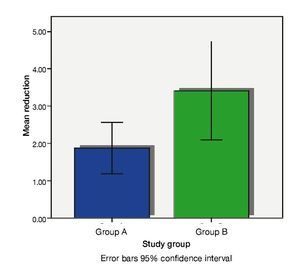
The average reduction in ulcer size during 8 weeks of follow-up for group A (compressive therapy) was 1.9 cm and for group B (compressive therapy and surgical treatment) was 3.4 cm with a confidence interval of 95% (Fig. 4).
Figure 4 Comparison of the reduction of the size of the ulcer in centimeters between groups A (compression therapy) and B (surgical and compressive therapy).
Figure 5 images of the follow-up of a patient from group A (compressive therapy).
Figure 6 images from the follow-up of a patient from group B (surgical and compressive therapy).
Discussion
Based on this study, we were able to find that the medical-surgical technique shown is better than the more conservative medical option. Favoring the results is the fact that no significant differences were found between the study groups in terms of age, weight, height, BMI, ankle-brachial index, and baseline measurement of the ulcer. Although patients in group B were younger (median age 58.44 years) than those in group A (median age 70.27 years), age wasn't significantly distinct. All this makes the possibility of distractor variables that could alter the final result less likely. Group B (medical and surgical therapy) showed a statistically significant reduction in ulcer size and complete healing (scarring) in 3 patients compared with group A. As Bush proves in his study with ulcer treatment at 8 weeks (11 patients out of the 14 initially included), group B showed a lower score in the visual analog scale of pain compared with group A, which was statistically significant from the third week of treatment.27
Considering the satisfactory evolution in group B with a statistically significant decrease in pain and ulcer size, it would be convenient to extend follow-up in order to evaluate complete healing in every patient within this group in particular. In addition, it is important to determine venous ulcer recurrence between both groups in order to demonstrate if there is a significant difference, as mentioned by the Landmark study ESCHAR (effect of Surgery and Compression on Healing and recurrence in patients with venous ulcers), which randomized 500 patients with advanced chronic venous insufficiency. The first group included 258 patients treated with compression, a second group with 242 patients was treated with compression and surgery; a recurrence after 12 months of 28% for the first group compared to 12% for the second group was found.28,29 the obtained results in this study of patients who underwent surgical procedure (group B) concur with the efficacy reported by Zamboni et al. In a randomized study of 45 patients with venous ulcers, 24 patients with compressive therapy and 21 patients with postsurgical use of elastic socks, with healing of 96% in a period of 63 days for the first group compared with 100% healing in 31 days for the second group,30 with the difference that in our study we utilized a minimally invasive procedure (microphlebectomy). Even though a sample of 20 patients is small (this being the study's main weakness), there is a clear tendency in favor of our experimental group. Another limitation of this study is a relatively short follow-up period. Terminal interruption of reflux source technique guided by ultrasound proved with statistically significant results to be more effective than the more conventional medical treatment to reduce pain and size of venous ulcers. The use of this surgical technique may be a promising line of minimal invasion in venous ulcer treatment in the immediate future. Further studies are required with this surgical technique and a longer follow-up period in order to evaluate recurrences.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
No financial support was provided.
Received: September 2013;
Accepted: March 2014
* Corresponding author:
Anillo Periférico 715-4 Avenue, Colinas de San Jerónimo, Z.P.
64630, Monterrey, N. L., Mexico (O. F. López-Lugo).