This study reports physical and psychological health outcomes following mindfulness- based stress reduction (MBSR) training in an inner city environment. Results show: (a) the relative difficulty contacting referrals; (b) a relatively high completion rate (65%) once people have enrolled in the program; and (c) clinically and statistically significant reductions over the eight weeks of the intervention period in measures of medical symptoms (MSCL) and anxiety (BAI), and corresponding increases in self-esteem (Self-Esteem Inventory) and mental health (SF-36). A small follow-up sample characteristic of the larger population showed maintenance of these changes for periods of up to seven years. The limitations of this uncontrolled descriptive study and the particular challenges and rewards of working in this environment are discussed.
Este estudio describe la evolución en variables físicas y psicológicas tras una intervención con el programa Mindfulness-based stress reduction (MBSR) en una ciudad del interior de Estados Unidos. Los resultados muestran: a) la relativa dificultad para contactar con las personas derivadas al programa; b) la tasa de cumplimentación relativamente alta (65%) una vez que los pacientes habían contactado con el programa, y c) la reducción significativa tanto desde el punto de vista clínico como estadístico a las ocho semanas de tratamiento en medidas de síntomas médicos (MSCL) y ansiedad (BAI), con incremento en la autoestima (Self-Esteem Inventory) y la salud mental (SF-36). Una pequeña submuestra mantuvo las mejorías a los siete años de seguimiento. Las limitaciones de este estudio no controlado y los particulares desafíos y recompensas que produjo en los profesionales también se discuten.
Very few mind/body-oriented stress reduction interventions are targeted to low income, multiracial, multicultural populations. Yet such populations suffer from high levels of poverty and concomitant psychosocial stress in our society (Adler, Boyce, Chesney, Folkman, & Syme, 1994). It seemed appropriate, therefore, to test the feasibility and potential impact on physical and psychosocial health of such an intervention, delivered under the umbrella of a neighborhood health center, and in which certain barriers to attendance, such as cost, need for childcare, and transportation were lowered by making the program free of charge, offering on-site day care and free transportation to and from the health center to attend classes, and by offering the program in Spanish as well as in English.
Mindfulness-based stress reduction (MBSR)The mind/body-oriented clinical intervention known as mindfulness-based stress reduction (MBSR) was developed in the Department of Medicine at the University of Massachusetts Medical Center (now UMass Memorial Medical Center) in 1979 (Kabat-Zinn, 1990). The program was established to address the needs of patients falling through the cracks of the health care system by challenging them to participate in their own movement toward greater health and well-being through engaging in fairly rigorous and demanding mindfulness meditation-based practices as a complement to the more traditional allopathic medical care they were receiving. MBSR programs have proliferated and now number over 200 worldwide, the great majority in major medical centers, hospitals, and clinics (Kabat-Zinn, 1997). MBSR is an example of the ways in which a comprehensive, well-described and well-documented mind/body orientation and methodology can be fully integrated within the delivery of services in a large academic medical center (Baer, 2003; Bishop, 2002). The fact that MBSR is based on intensive training in the Buddhist meditative practice known as mindfulness, as well as on mindful hatha yoga, underscores the degree to which unconventional approaches have become established within mainstream medical practice, in large part driven by the rising desire of health care “consumers” for alternative approaches within medicine (Eisenberg et al., 1998; Eisenberg et al., 1993) and for alternative services to which overburdened physicians might send patients who have only responded partially, if at all, to their treatments (Epstein, 1999; Kabat-Zinn, 1982).
The clinical effectiveness of MBSR has been reported in a number of studies from the “parent” clinic, which serves a predominantly white, middle-class and working-class population of medical patients referred with a wide range of chronic stress-related disorders, chronic pain conditions, and chronic diseases (Kabat-Zinn, 1982; Kabat-Zinn, & Chapman- Waldrop, 1988; Kabat-Zinn, Lipworth, & Burney, 1985; Kabat-Zinn, Lipworth, Burney, & Sellers, 1986; Kabat-Zinn et al., 1992; Miller, Fletcher, & Kabat-Zinn, 1995). Additional studies of this population have documented a high and invariant (over sixteen years) rate of program completion (Kabat-Zinn, Chapman, & Salmon, 1997; Salmon, Santorelli, & Kabat-Zinn, 1998). There is now a growing literature on the effects of MBSR programs serving a variety of different populations, including a predominantly fundamentalist Christian demographic (Randolph, Caldera, & Greak, 1999), patients with fibromyalgia (Golderberg, Kaplan, Nadeau et al., 1994; Kaplan, Golderberg, & Glavin-Nadeau, 1993; Weissbecker et al., 2002), cancer patients (Carlson, Ursuliak, Goodey, Angen, & Specca, 2001; Specca, Carlson, Goodey, & Angen, 2000), and a general medical population similar to ours (Reibel, Greeson, Brainaard, & Rosenzweig, 2001). MBSR has also been adapted for medical students (Shapiro & Schwartz, 1999; Shapiro, Schwartz, & Bonner, 1998), and delivered in the corporate work environment. Also, a randomized trial showed a significant shift in frontal activation asymmetry in the brains of MBSR subjects but not in wait-listed controls, consistent with a less reactive and more effective processing of emotions at baseline and in response to induced stress, and a correspondingly greater immunocompetence, as measured by response to an influenza vaccine challenge (Davidson et al., 2003). Recent developments have seen an integration of the MBSR approach within cognitive therapy, giving rise to what is now known as mindfulness-based cognitive therapy (MBCT). MBCT has been shown to halve the rate of relapse following successful pharmacotherapy for major depressive illness (Segal, Williams, & Teasdale, 2002; Teasdale, Segal, & Williams, 1995; Teasdale et al., 2000). Mindfulness is also a key element in acceptance-based cognitive-behavioral treatments for generalize anxiety disorder (Borkovec, 2002; Hayes, Strosahl, & Wilson, 1999; Romer, & Orsillo, 2002), as well as in dialectic behavior therapy (Linehan, 1993). However, to date, very few MBSR clinics or other mind/body-oriented interventions, with the notable exception of the work of Roth and colleagues (Roth, 1997; Roth, & Creaser, 1997; Roth, & Stanley, 2002) have focused on addressing the specific needs of underserved minority populations in the inner city.
This report: (a) documents the feasibility and clinical and social impact of MBSR with low-income, minority populations based on data from seven years of continual experience with this program in the inner city in Worcester, Massachusetts, and (b) highlights population-specific challenges in both the delivery and the investigation of this intervention.
MethodsPopulation DemographicsA demographic characterization of the population is presented in Table 1. The ratio of women to men in both the referral population (N=1,898) and in the cohort of first-exposure program completers (N=452) was approximately three to one. Over 60% were receiving government assistance, and this percentage was higher in the Latino population than in the English-language cohort, both for all referrals and for first-exposure completers (p=.0086). Only approximately twenty percent of individuals were gainfully employed, again higher in the English-speakers and lower in the Spanish-speakers (p<.0001). Eighty-eight percent of Latino completers had an annual income below $15,000. For the English-language completers, 72% had an annual income below $15,000 (p<.0001).
Demographics: total referral population (N=1,898).
| Overall | Spanish | English | |
|---|---|---|---|
| Age | 39.46 (993) Range 14-77 | 40.11 (529) Range 14-70 | 38.72 (464) Range 15-77 |
| Years of education | 10.91 (820) Range 0-24 | 9.38 (452) Range 0-19 | 12.79 (368) Range 2-24 |
| Years w/condition | 8.3 (314) Range 0.08-54 | 5.97 (147) Range 0.08-31 | 10.36 (167) Range 0.08-54 |
| Gender (% Female) | 1418/1876 75.59% | 735/967 76.01 | 683/909 75.14 |
| Receiving government assistance | 590/862 68.45% | 339/456 74.34% | 251/406 61.82% |
| Income<$15,000 annually | 683/798 85.59% | 375/408 91.91% | 308/390 78.97% |
| Work outside the home | 160/835 19.16% | 54/442 12.22% | 106/393 26.97% |
Demographics: first-exposure program completers cohort (N=452).
| Overall | Spanish | English | |
|---|---|---|---|
| Age | 41.70 (447) Range 14-75 | 41.93 (244) Range 14-70 | 41.43 (203) Range 15-77 |
| Years of education | 11.38 (432) Range 0-24 | 9.74 (236) Range 0-19 | 13.36 (196) Range 2-24 |
| Years w/condition | 7.8 (168) Range 0.08-54 | 6.24 (91) Range 0.08-30 | 9.63 (77) Range 0.08-54 |
| Gender (% Female) | 347/452 76.77% | 194/245 79.18% | 153/207 73.91% |
| Receiving government assistance | 271/425 63.76% | 159/229 69.43% | 112/196 57.14% |
| Income<$15,000 annually | 325/405 80.25% | 187/213 87.79% | 138/192 71.88% |
| Work outside the home | 97/429 22.61% | 28/230 12.17% | 69/199 34.67% |
The majority of the participants in the Spanish classes were from Puerto Rico, followed in descending order by individuals from other regions of the Caribbean, from Central America, and from South America. North American Latinos with Spanish as a second language also attended. The Latino population represented the full spectrum of racial origins and racial mixing characteristic of most Caribbean, Central and South American societies. Among the participants in the English classes were Caucasians, African Americans, Native Americans, Latinos with English as their main language, and recent immigrants from Central and Western Africa, Egypt, Eastern Europe, Germany, the Middle East, and the Caribbean.
Referral Sources and Reasons for ReferralEighty percent of all referrals in this study came from providers (i.e., physicians, nurse practitioners, mental health specialists, and social workers) at health centers in the Worcester area1. Self-referrals stemmed from word-of mouth or from radio advertisements and occasional newspapers articles about the clinic. The most common referral and self-referral reasons were to learn to cope more effectively with stress, pain, anxiety, and depression. Depression was very prevalent in this population. Many individuals presented with a wide range of medical diagnoses (angina, asthma, cancer, chronic fatigue, congestive heart failure, Crohn's disease, fibromyalgia, headaches, hepatitis, HIV infection and AIDS, seizure disorder, and chronic pain) and psychiatric diagnoses (depression, life stress, anxiety, PTSD, panic disorder, insomnia, complicated bereavement, schizophrenia, substance abuse recovery, and violent behavior). Most had complex personal histories of family, psychosocial, and economic stress as well.
Description of the MBSR interventionThe major features of MBSR have been described in considerable detail (Kabat-Zinn, 1990, 1996, 1999, 2003; Santorelli, 1999), as have some of the more general features of mindfulness meditation practice and its applications in everyday life within a Western context (Beck, 1993; Goldstein, 2002; Goldstein, & Kornfield, 1987; Hanh, 1998; Kabat-Zinn, 1994; Rosenberg, 1998; Salzberg, 1999; Suzuki, 1970; Tarrant, 1998). MBSR is an outpatient group patient education intervention, consisting of eight 2.5hours weekly classes and an all-day silent meditation retreat on the weekend of week 6. The original format (recently modified in the parent clinic to a group-based introductory interview to accommodate changing realities in health care delivery at our institution) included an individual pre-intervention interview for each referral prior to enrolling in the group program. The purpose of the interview is for the clinician to encounter the patient as a unique individual, listen attentively to the patient's psychosocial and medical history, explain the program and its modalities, screen for potential barriers to effective participation (such as suicidality, alcohol or drug abuse), and clarify the level of commitment required for acceptance into the program. A post-intervention individual interview follows the program. Its purpose is to build on the work each person did during the program, give personalized attention to present and future goals and intentions and potential impediments to continued implementation of the mindfulness practices, give individualized suggestions, clarify questions the participant may have, and reinforce efforts to apply the skills developed in the program in “real-life” situations. In this study, both interviews were conducted by the MBSR class instructor. The program is offered in eight-week cycles which typically occur in the Fall, Winter, Spring and Summer.
Initially funded by the Nathan Cummings Foundation, the inner city MBSR program was established in January 1992. Between 1994 and 1999, the program was primarily supported by the operating budget of the Center for Mindfulness, supplemented by small and occasional grants from the Massachusetts Department of Public Safety and the Robbinsde Beaumont Foundation.
The MBSR intervention was modified in the inner city clinic to accommodate the specific needs of its potential participants: (a) class length was kept to 2hours during the initial 12 cycles to keep the demanded characteristics in a moderate range. However, in Cycle 13, the instructors extended classes to the normal 2.5hours to have more time for the teaching; (b) the timing of morning classes (9:30AM to Noon instead of 9AM to 11:30AM) accommodated the school bus schedule to facilitate the attendance of single parents needing to wait for the pick-up and drop-off of their school-age children; (c) most of the classes took place in the morning; on three occasions, classes were offered in the evening to accommodate working Spanish-speaking participants; (d) initially the all-day retreat in week six that is an integral part of the MBSR program was not included in the inner city program curriculum. Beginning in Cycle 9, participants were invited (optional) to attend the all-day retreats held at the main campus. However, over all cycles, only eight patients in total from the Spanish classes attended (3.3%), while approximately 15% of the English-speaking patients did so; (e) as noted, the inner city program was offered free of charge; (f) free on-site child care (with bilingual day-care personnel) and a voucher system for free door-to-door taxi transportation were offered for those individuals in need of this assistance; (g) the program was offered in Spanish as well as in English to make it maximally accessible for non-English-speaking Hispanics, who constitute a large percentage (43%) of the Worcester inner city community; (h) guided mindfulness meditation practice tapes were translated into Spanish and adapted for that population; (i) starting in Cycle 13, a full workbook in Spanish was given out at the beginning of the course (to match the intervention protocol provided to English-speaking participants); (j) data forms and questionnaires were available in English and Spanish; and (k) beginning in Cycle 3 introductory group meetings were substituted for individual interviews and were used to present the program to all referred individuals who chose to come, prior to enrollment in the program. This modification in the standard MBSR individual pre-intervention format was in response to a very high no-show rate for the initial interviews (80% of referrals were no-shows to the scheduled interviews). Following this introductory group meeting, interested individuals were then scheduled for an individual meeting with the instructor, which preceded the formal start of the group program.
Due to improved attendance at initial individual evaluation interviews, the group interview format was abandoned after Cycle 16.
Outcome measuresSelf-report assessments were conducted prior to and following participation in the MBSR program. The assessment instruments as well as how they were administered (individual interview vs. group format) changed over time (Table 2). Post-intervention, the data forms were given out in the last class, and were reviewed by the instructor at the time of the individual post-intervention interview. Individuals unable to read or comprehend the forms received help to complete the forms from family members. Others received help from the instructor at the post-intervention interview.
Measurement instruments and administration formats by program cycle.
| Cycles | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement Instruments | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | F/U |
| MSCL | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| BAI | X | X | X | X | X | X | X | X | X | X | ||||||||||
| SEI | X | X | X | X | X | X | ||||||||||||||
| SF-36 | X | X | X | X | X | X | X | X | X | X | X | |||||||||
| Outcome Questionnaire | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Baseline Assessment Format | ||||||||||||||||||||
| Group1 | X | X | X | X | X | X | X | X | ||||||||||||
| Individual2 | X | X | X | X | X | X | X | X | X | |||||||||||
| All follow-up assessments were distributed at final (8th) class and collected at exit interview3 | ||||||||||||||||||||
Group administration consisted of reading each individual item of the questionnaires out loud to the group with the purpose of enhancing questionnaire completion rates.
The Medical Symptom Checklist (MSCL) (Kabat-Zinn, 1982), a measure of medical and psychological symptoms, was used in all cycles in this study (Cycles 1-19). The Beck Anxiety Inventory (Beck, Epstein, Brown, & Steer, 1988) was employed in Cycles 1-10. The Coopersmith Self-Esteem Inventory (Coopersmith, 1981) was used (Cycles 1-6), and the SF-36 (Ware, Snow, Kolsinski, & Gandek, 1993) in Cycles (10-19). A multipart Outcome Questionnaire (Kabat-Zinn et al., 1986)2 with different scaling for different parts was also employed post-intervention. On this retrospective face valid measure, participants could rate their level of change on a range of items assessing specific outcomes of relevance to them (Part 1: coping with stress; overall feeling; energy level and stamina; activity level; attendance at work or school; doctor and ER visits; medication use; frequency of pain episodes; severity of pain; blood pressure) and on compliance with the various meditation practices. They also rated the usefulness of different aspects of the program curriculum, as well as the degree of change they experienced on a range of specific health attitudes and behaviors (knowing to take better care of myself; actually taking better care of myself; believing that I can improve my own health; feeling self-confident; feeling hopeful; feeling assertive, etc.). A summary measure, the Outcome Average, gives an overall assessment of the degree of change on the specific items listed above (Part 1). On this scale, the higher the score, the greater the change. (1=much worse; 2=somewhat worse; 3=no change; 4=somewhat better; 5=great improvement). On the Health Attitudes and Behavior Change measure, the lower the score, the greater the change (1=great positive change; 2=some positive change; 3=no change; 4=negative change). All forms were translated into Spanish, except for the SF-36, for which the validated Spanish version was used.
Because different measures were used at different times over the course of the seven years of the program, and because of difficulty in obtaining post information on all completers, the reported sample size for various outcome determinations differs for different measures. Only MSCL and the Outcome Questionnaire were employed continuously over the seven-year study period.
Data AnalysisDataPerfect was used to enter compliance data and KeyEntry III for all data from outcome measure questionnaires. SAS Version 8 was used for all data analyses [PROC UNIVARIATE; PROC TTEST; PROC NPAR1WAY (for non-parametric analyses)].
A number of population-specific factors and the fact that our program was not constituted as research project but as an effort to document feasibility study shaped the data gathering and analysis. The fact that there were multiple referral routes into the clinic, coupled with high no-show and dropout rates, great difficulty in contacting people due to lack of telephone (the intervention well preceded the widespread use of cell phones) or frequent change of address, as well as a high percentage of people who attempted to complete the program on multiple occasions, and individuals who attended classes without ever having completed pre-data forms presented a range of challenges in obtaining reliable and complete demographic and program adherence data. For example, 2,676 names appeared on our lists of people who were either referred to the program or who inquired about it themselves between January 1992 and March 1999. Due to redundancies and individuals who took the program multiple times, it was determined through a stringent review of patient lists that only 1,898 (71.0%) of the 2,673 entries in the database were unique individuals. However, of these 1,898 unique individuals, 929 (48.9%) either expressed no interest in taking the program or were not reachable by any means, and were therefore lost to contact or follow-up; their names simply appeared on our master list one or more times, and no further information on them was ever recorded. Only patients with unique exposure and complete pre- and post-intervention data on at least one outcome measure were included in the present analysis of outcome, although the demographic results are reported for all subjects for whom there were data, as well as for the cohort of unique exposure completers.
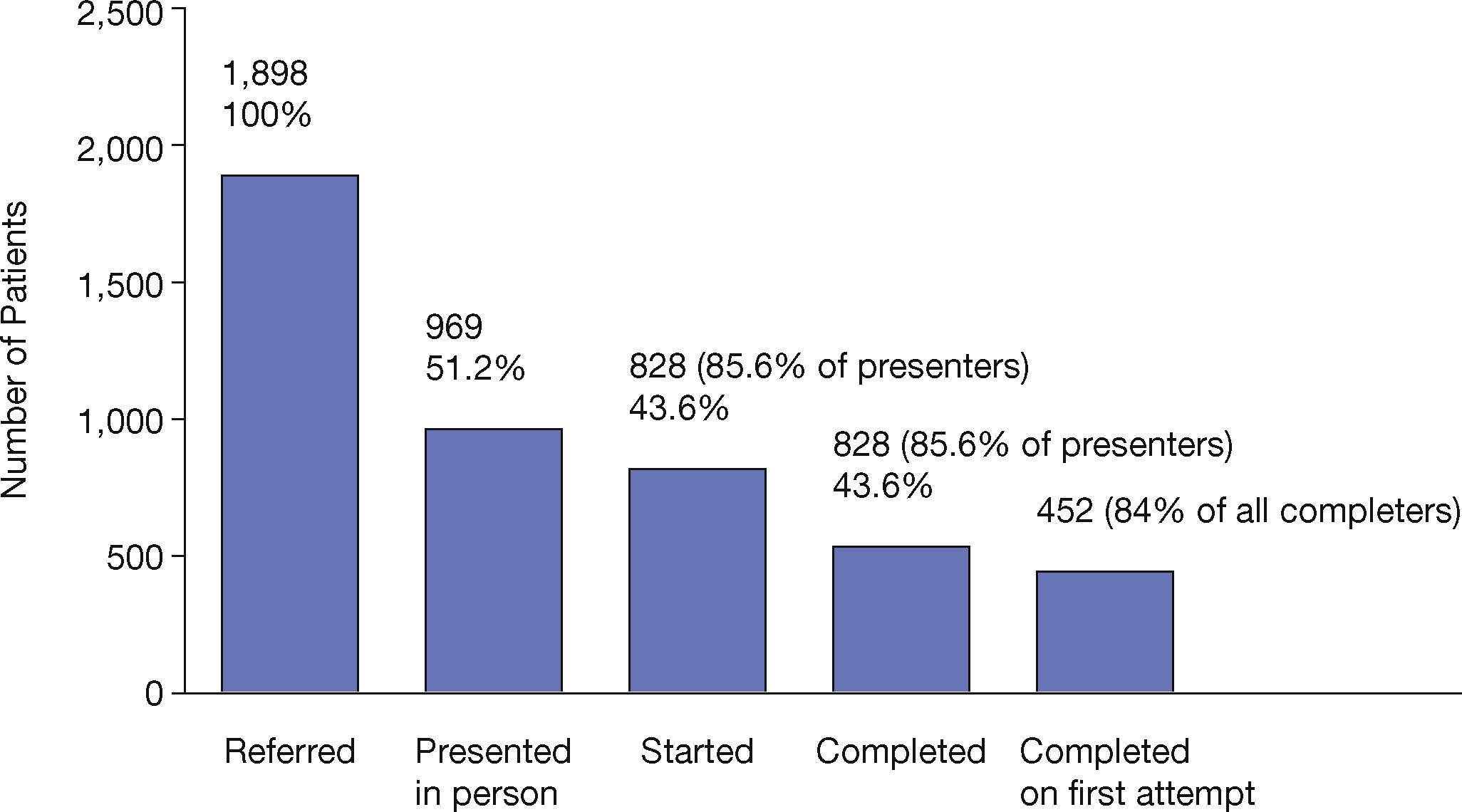
ResultsParticipantsAs noted, 1,898 unique individuals (51% Spanish-speaking, 76% female) were referred or self-referred to the city campus MBSR program between January 1992 and March 1999. Of these, 929 (48.9%) were either not reachable by any available means, or indicated that they were not interested in the program. The remaining 969 individuals (51.2%) physically presented at the clinic in person at least one time (i.e., attended an introductory group meeting or an individual interview, and supplied data consistent with an encounter: i.e., initial data entered for demographic variables or pre-intervention assessment measures). Of these, 124 individuals enrolled the program more than once (some did not complete the eight-week program on their first attempt but re-enrolled for a subsequent cycle; others enrolled in the program and completed it more than one time).
Program AdherenceFigure 1 shows the fate of referrals as a function of stages of the process. Of the 969 individuals who had at least one initial in-person encounter recorded, 828 (85.4%) enrolled in the program (i.e., attended at least class #1 and/or class #2). Of those, 538 (65.0%) completed the program, with 452 individuals completing it only once (84.0% of all completers) and 86 completing it between 2 and 7 times (a completer was defined as an individual who attended at least five classes, including either class #7 and/or class #8 and/or had filled out the post-intervention assessment).
Outcomes for Individuals who Completed the Program on their First Attempt (N=452)Table 3 shows there was an overall reduction of 23.94% in the number of medical symptoms reported on the MSCL for the entire group over the course of the intervention (premean: 37.51, post-mean: 28.53; p<.0001; N=450). Comparable significant changes were observed among subgroups of individuals (e.g., English-class participants, Spanish-class participants, males, females) (see Table 3).
Outcomes on the Medical Symptom Checklist (MSCL).
| N | Pre-MSCL | Post-MSCL | % Change | Sd | p | |
|---|---|---|---|---|---|---|
| Unique Exposure | 450 | 37.51 | 28.53 | −23.94 | 13.41 | 0.0001 |
| Unique Exposure English | 205 | 32.52 | 23.77 | −26.91 | 14.46 | 0.0001 |
| Unique Exposure Spanish | 245 | 41.68 | 32.51 | −22.00 | 12.50 | 0.0001 |
| Unique Exposure English Male | 53 | 26.66 | 19.15 | −28.17 | 14.03 | 0.0003 |
| Unique Exposure English Female | 152 | 34.56 | 25.38 | −26.58 | 14.62 | 0.0001 |
| Unique Exposure Spanish Male | 51 | 39.96 | 34.00 | −14.92 | 10.09 | 0.0001 |
| Unique Exposure Spanish Female | 194 | 42.13 | 32.12 | −23.77 | 12.95 | 0.0001 |
Mean anxiety scores on the Beck Anxiety Index also decreased significantly post-intervention (pre-BAI=21.11; post-BAI=13.56; p<.001; N=241), with an overall reduction of 35.8% (Table 4). Similar results were observed for gender and language subgroups although sample size was considerable smaller for some subgroups (i.e., males in classes delivered in English).
Outcomes on the Beck Anxiety Inventory (BAI).
| N | Pre-BAI | Post-BAI | % Change | Sd | p | |
|---|---|---|---|---|---|---|
| Unique Exposure | 241 | 21.11 | 13.56 | −35.77 | 10.40 | 0.0001 |
| Unique Exposure English | 114 | 17.21 | 10.78 | −37.36 | 10.42 | 0.0001 |
| Unique Exposure Spanish | 127 | 24.61 | 16.06 | −34.77 | 10.33 | 0.0001 |
| Unique Exposure English Male | 31 | 16.55 | 9.52 | −42.50 | 8.24 | 0.0001 |
| Unique Exposure English Female | 83 | 17.46 | 11.25 | −35.54 | 11.16 | 0.0001 |
| Unique Exposure Spanish Male | 28 | 23.68 | 17.11 | −27.75 | 9.29 | 0.0009 |
| Unique Exposure Spanish Female | 99 | 24.88 | 15.76 | −36.66 | 10.58 | 0.0001 |
An 11.87% increase in self-esteem was observed on the Coopersmith Self-Esteem Inventory over the course of the intervention (pre-SEI=51.46, post-SEI=57.57; p<.001; N=119) (Table 5). Similar findings were observed for the English and Spanish classes. There was no statistically significant difference in the degree of change between the English and Spanish cohorts, but the initial level for the former was significantly higher than that of the latter (p=0.024). When stratified by language and gender, a significant pre- and post-increase was observed for both cohorts of females but not for the males, perhaps due to the low sample size of the males (Table 5).
Outcomes on the Coopersmith Self-Esteem Inventory (SEI).
| N | Pre-SEI | Post-SEI | % Change | Sd | p | |
|---|---|---|---|---|---|---|
| Unique Exposure | 119 | 51.46 | 57.57 | 11.86 | 16.88 | 0.0001 |
| Unique Exposure English | 54 | 56.22 | 61.54 | 9.47 | 17.63 | 0.0308 |
| Unique Exposure Spanish | 65 | 47.51 | 54.27 | 14.21 | 16.34 | 0.0014 |
| Unique Exposure English Male | 16 | 57.05 | 60.55 | 6.13 | 20.04 | 0.50 (ns) |
| Unique Exposure English Female | 38 | 55.86 | 61.96 | 10.97 | 20.59 | 0.0309 |
| Unique Exposure Spanish Male | 15 | 52.88 | 56.44 | 6.73 | 10.60 | 0.21 (ns) |
| Unique Exposure Spanish Female | 50 | 45.91 | 53.61 | 16.79 | 17.68 | 0.0034 |
Pre- and post-scores on the SF-36 show statistically significant across-the-board improvements on all subscales (Table 6). However, when subscale results were expressed as physical (PCS) and mental (MCS) component summary scores, only the mental component was significant (Table 6). When English and Spanish cohorts were compared (data not shown), there were no significant pre- to post-intervention differences in the degree of change on any of the subscales or summary scales on the SF-36 except for the General Health Percepts subscale, where the change in the Spanish cohort on this subscale (20.29% increase; pre-mean: 39.61; post-mean: 47.65) was much greater than that for the English cohort (7.97% increase; pre-mean: 51.84; post-mean: 55.97), potentially due to the much higher initial mean score for the English-speaking group and a possible ceiling effect. Analysis by language and gender of both the MCS summary measure and the mental health (MH) subscale showed no remarkable features, except that the Spanish females showed a 47.7% increase on the MH subscale, dramatically and statistically significantly higher than for any of other cohort.
Outcomes on the Subscales of the S F-36.
| N | Pre | Post | % Change | Sd | p | |
|---|---|---|---|---|---|---|
| Physical Functioning | 177 | 59.03 | 64.29 | 8.91 | 24.09 | 0.0041 |
| Role Physical | 162 | 41.98 | 52.11 | 24.14 | 41.36 | 0.0022 |
| Body Pain | 176 | 46.77 | 53.56 | 14.52 | 21.92 | 0.0001 |
| Gen Health Percepts | 168 | 45.80 | 51.86 | 13.23 | 17.12 | 0.0001 |
| Vitality | 173 | 39.46 | 50.83 | 28.81 | 23.35 | 0.0001 |
| Social Functioning | 177 | 50.21 | 62.50 | 24.47 | 26.77 | 0.0001 |
| Role Emotional | 160 | 38.96 | 55.42 | 42.25 | 50.57 | 0.0001 |
| Mental Health Index | 176 | 43.69 | 58.11 | 33.00 | 20.64 | 0.0001 |
| PCS* | 149 | 40.27 | 41.13 | 2.15 | 8.11 | 0.20 (ns) |
| MCS** | 149 | 35.05 | 42.71 | 21.85 | 10.84 | 0.0001 |
On the Outcome Questionnaire, the mean Outcome Average (N=441) post-intervention was 3.88, indicative of a moderate degree of overall positive change among completers (3.0=no change). Seventy-five percent of completers had an outcome average score of 3.44 or above, and 25% had an outcome average score of 4.25 or above. There was no significant difference between English (mean: 3.82) and Spanish (mean: 3.92) cohorts although a trend towards significance (p=0.06) was observed. On the Importance Score (rating of the importance of the program to each individual, where 1=“not important at all” and 10=“very important”) there was a significant difference between Spanish and English cohorts (English mean: 8.96; Spanish mean: 9.65, p<.0001). On the summary Health Attitudes and Behavior Change index, there was also a significant difference between English and Spanish cohorts, although both scored in the moderate to high positive change range (English mean: 1.78; Spanish mean: 1.67, p=0.016).
Follow-up AssessmentA total of 36 people participated in the follow-up assessment. Participants were equally divided between English speaking (N=18) and Spanish-speaking (N=18). There were 8 men and 28 women. The gender by language distribution of the follow-up participants was representative of the overall distribution of graduates. Follow-up times varied widely, as the graduates came from as early as Cycle 3 (1993) to as late as Cycle 19 (1999). As a cohort, the participants in the follow-up assessment showed statistically significant pre- to post-intervention changes on five SF-36 subscales: vitality, social functioning, role emotional, mental health, as well as on the mental component summary scale (data not shown). The change pattern over the course of the intervention period for these individuals is qualitatively and quantitatively consistent with changes observed for the entire population of program completers as shown in Table 6. At follow-up, no statistically significant changes were observed between post and follow-up scores for this cohort of 36 individuals, suggesting that the positive changes observed immediately following the eight-week intervention were maintained for extended periods of time ranging from several months to seven years following completion of the program.
DiscussionOur experience revealed that this multicultural population of low-income and ethnically diverse individuals, 86% of whom have an annual income below $15,000, 68% of whom are receiving government assistance, and 19% of whom work outside the home (see Table 1) face many challenges in attending and staying in the MBSR program, in spite of the reduction of some of the common barriers to attending. Forty-eight percent of the 1,898 individuals referred to the program did not come in for an initial interview (individual or group) compared with only 25% in studies of program compliance in the parent clinic (Kabat-Zinn, & Chapman-Waldrop, 1988). The 65% program completion rate of program enrollees was also markedly lower than the 84% completion rate observed in the parent program (Kabat-Zinn, & Chapman-Waldrop, 1988). We interpret these findings as evidence of a greater burden on this population to adhere to the program in spite of the clinic's efforts to support attendance and program completion through making the program free of charge and offering free transportation and child care. Nevertheless, the 65% overall completion rate observed is in itself remarkable, given the duration and high demands of the program coupled with the high levels of psychosocial stress and low formal educational experience characteristic of this population. It is noteworthy that 84% of all the program completers completed it on the first attempt.
We found a significant reduction in symptom reporting (MSCL and BAI) among all sub-cohorts (English/Spanish; Male/Female; and Language by Gender) (Tables 3 and 4). Symptom reporting (MSCL and BAI) was highest among women in the Spanish-speaking classes; nevertheless, they were as successful in symptom reduction as women in the English-speaking classes. Pre-intervention symptom reporting (MSCL and BAI) was greater among Latino men than for English-speaking cohorts, and they were less successful in reducing symptoms than were other cohorts. However, the Spanish-speaking men demonstrated notable and statistically significant improvement over initial values on all indices, with the exception of the Self-Esteem Inventory, where statistical significance was not attained for males in either the English-language or Spanish-language classes, perhaps due to small sample size. It remains to be seen if the gains observed among the Latino men can be enhanced through further intervention.
The Spanish-speaking cohort had lower initial self-esteem scores than the English-speaking cohort (Table 5), but both cohorts showed a post-intervention improvement. However, post-intervention, the Latino women had attained only the initial self-esteem levels of their English-speaking counterparts. This may be an indication that the Latino women suffer from social obstacles not faced by the English-speaking women, such as the language barrier and lower education levels, obstacles that may affect self-esteem through preventing them from feeling completely integrated into mainstream culture (Vasquez, 2002). The small number of men made it impossible to determine any degree of change on this index with adequate statistical confidence.
Outcomes on the SF-36 (Tables 6) also demonstrated significant improvement on all the subscales and the Mental Health Summary (MCS) measure but not on the Physical Health Summary (PCS) measure for all participants. The low initial overall level on the MCS (mean: 35.05) compared to the national norm (50.00) (Ware, Kozinski, & Keller, 1994) indicates a high initial degree of emotional distress in this population, consistent with the fact that most individuals were referred by health professionals for conditions associated with endemic depression, life stress, and anxiety. Given this baseline status, it is noteworthy that the Mental Health Index, Role Emotional, and Vitality scales showed major improvements over the course of the intervention. The changes observed on the MCS and MH indices were comparable for both the English-speaking and Spanish-speaking cohorts (data not shown), except that the Latino women showed a significantly greater improvement on the MH subscale (47.7% change in the mean) compared with the English-language female cohort (28.4% change in the mean). Given the high and statistically significantly different level of initial anxiety reported by the Spanish-speaking women on the BAI (mean: 24.88), compared with the English-speaking women (mean: 17.46) (p=.0001), the results suggest that the Spanish-speaking women effectively used the intervention to optimize their mental health in spite of high initial levels of emotional distress.
Although only a small group of individuals responded to our invitation to participate in the follow-up assessment, this cohort appeared to be representative of the larger group of program completers in terms of outcome. Follow-up findings suggested that the initial improvements in medical symptoms (MSCL score) and the mental health (MH) subscale and mental component summary (MCS) measure of the SF-36 were all maintained for a period of up to seven years post-intervention. Follow-up studies of MBSR from the larger parent clinic (Kabat-Zinn et al., 1985; Kabat-Zinn et al., 1986; Miller et al., 1995) have found that up to 93% of individuals referred continue to adhere to at least some elements of the program and maintain their initial improvements.
The results reported here, taken in toto, suggest that the participants in the inner city MBSR program, in both the English and Spanish-language classes, experienced significant positive changes in both physical and mental health indicators over the period of the intervention. The mental health outcomes suggest that the majority of participants were able to change their relationships with their interior mental processes, especially with their thoughts and disturbing emotions, as taught and emphasized by the various mindfulness meditation practices that formed the heart of the intervention, even in the face of high levels of psychosocial stress and health problems. The improvements observed in symptoms and in self-esteem, along with the positive changes reported retrospectively in health attitudes and behaviors among the participants, may stem in part from an experience of greater self-efficacy (Bandura, 1982), the confidence in one's ability to learn and grow and make important and desired changes in one's life, a theme emphasized by the MBSR program in working in a disciplined and regular way with the various meditation practices and their applications to everyday life (Kabat-Zinn, 1990, 1994; Santorelli, 1999).
Combined with the program adherence data, the overall thrust of these observations is that MBSR can be effectively delivered in a multiethnic low-income inner city community, resulting in significant changes in a range of measures of psychosocial and physical well-being among those who enroll in and complete the eight-week program. These results replicate and extend those reported by Roth and colleagues (Roth and Creaser 1997). They confirm that MBSR can be delivered in Spanish as well as in English, and show that it can have a profound impact on people's lives and health in ways that may be sustained well beyond the brief period of the intervention. Our findings also suggest that the mindfulness practices themselves are culturally acceptable and effective in an ethnically diverse population with no prior exposure to the meditation-based methods and learning environment characteristic of MBSR training. They also suggest that MBSR can be delivered effectively in the context of neighborhood health centers, and that it meets a significant need that is often unaddressed in health services for low-income social strata. Our anecdotal and clinical impressions of delivering MBSR in this community over an extended period of time suggest that the intervention clearly promotes increased satisfaction with their health care among patients as they learn to participate more fully in it through self-regulatory practices such as meditation and yoga, as a complement to the care their receive from their various health providers. Although we did not study it systematically, we observed that the availability of MBSR for their patients also increased satisfaction among health care providers, because it offered them a referral option through which patients with the most intractable and difficult to manage medical and psychosocial conditions could: (a) be challenged to assume some degree of responsibility for their own health; (b) achieve important health-related goals; and (c) improve their capacity for recognizing and dealing effectively with psychosocial stress.
Challenges and limitations of the present studyThis study was designed as a descriptive evaluation of the feasibility of delivery and of the potential therapeutic outcomes of a well-established mind/body intervention offered to a population that rarely has exposure to such clinical options. The interpretation of our results is necessarily limited by a number of methodological and social challenges we faced in attempting to characterize and document various aspects of the total referral population, as well as in characterizing the program participants and documenting their short and long-term outcomes: (a) we were only able to contact and engage about half of the referral population; (b) we encountered difficulty obtaining complete data on all individuals who presented at the clinic at all times, perhaps due to unusually high levels of social instability and its consequent effects on program adherence, in addition to literacy issues; (c) we modified the outcome assessment battery at different times (Table 2), we abandoned the Self-Esteem Inventory in Cycle 7 and the Beck Anxiety Inventory in Cycle 11 and added the SF-36 in Cycle 10, all in an effort to obtain broader and more reliable measures of health status and change while seeking not to overload participants with too many complex questionnaires; (d) these modification of the assessment battery limited statistical power and thus our ability to evaluate change and make comparisons on specific change measures in subcohorts of participants; (e) we learned that working with the non-English-speaking Latino population requires careful evaluation of assessment instruments, as many of the instruments we routinely employed in other venues were not available in Spanish or lacked culture-specific normative data. Although we had the assessment measures used in this study translated professionally, with the exception of the SF-36, for which a Spanish version was available, no norms were available to compare the results of our population to an appropriate normative sample; (f) the study lacks an appropriate comparison control group from the same community.
Directions for further researchOur findings and those of Roth and Creaser (1997) suggest a number of fruitful lines for further investigation. These include: (a) the evaluation of the effectiveness of MBSR in this population by means of a well-designed and well-executed randomized clinical trial; (b) the investigation of pathways by which mindfulness-based interventions may improve mental health in this population, building on studies of MBSR (Davidson et al., 2003, in press) and MBCT (Teasdale et al., 2000; Segal et al., 2002) suggesting specific roles for mindfulness in countering dispositional negative affect and chronic depressive rumination; (c) the development and testing of a range of strategies to enhance health care provider receptivity and referrals to MBSR programs in inner city health centers.
ConclusionsIn spite of the obvious limitations of the present study, our findings demonstrate that MBSR can be delivered successfully in both English and Spanish in an inner city environment in conjunction with a single neighborhood health center, supported by additional referrals from other centers and community service organizations. An overall program completion rate of 65% suggests a high degree of motivation on the part of the majority of enrollees, in spite of significant psychosocial pressures that make compliance with and completion of any extended behavioral intervention difficult. The majority of participants experienced notable physical and emotional symptom reduction, and increases in self-esteem and mental health.
Future efforts to implement the MBSR program model in inner city healthcare settings are faced with challenges related to the lack of reimbursement for mind/body-oriented interventions by Medicare and Medicaid and other providers who set the agenda for the delivery of social and medical services in neighborhood clinics. We were able to offer the program to participants free of charge because it was supported first by grants and then by operating revenues from other programs conducted by the Center for Mindfulness. This was not a strategy for long-term self-sufficiency, but for facilitating a time-limited demonstration project and then attempting to keep a program that was clearly contributing to the local community alive for as long as possible. The worsening fiscal environment in healthcare ultimately required the closing of the inner city MBSR program in July of 2000.
As noted, our original impetus for establishing the inner city clinic was in large measure to offer MBSR to a low SES, multiethnic, multiracial population that would ordinarily not be exposed to opportunities to learn, practice, and incorporate mind/body self-awareness strategies into the conduct of their highly stressful lives as a complement to the more traditional medical care they were receiving. We wished to test the feasibility and effectiveness of delivering such an intervention and demonstrate its potential universality beyond the population in which it was first developed. Our experience over the past seven years has shown that such a group-based intervention, delivered in conjunction with a neighborhood health center, can be well-received by this population when the barriers to attendance and to learning are reduced. Such a program also served as a “laboratory” for the exploration of cultural differences within a diverse population, and how such differences might affect or not affect the participants’ ability to make maximum use of the intervention. It also allowed us to test the value of MBSR as a referral destination to which overextended and overwhelmed healthcare professionals within neighborhood health centers could send their patients and clients. It afforded their patients an opportunity to develop confidence in their own abilities for learning, growing, healing, and coping more effectively with the spectrum of inner and outer difficulties they faced through, training in the meditation practices themselves and the life-skills, health attitudes and behaviors that stem from such training. The degree to which this diverse population of individuals experienced greater self-regulation and self-efficacy is reflected in the improvements in the various physical and psychological outcome measures reported in Tables 3-6 and on the various components of the Outcome Questionnaire.
The authors wish to extend their thanks for the work of Rafaela Morales as administrator of the inner city clinic; Barbara Stone for her work as an instructor in the English-speaking classes in several cycles; Carol Hester for organizing the childcare space and delivering the childcare with great devotion for five years; Janet Báez and Sonia Vélez, both graduates of the program, for their devotion and work in the childcare program; Carmen Torres for secretarial support; Delia Ramos for keeping the childcare rooms and the MBSR classroom spotless; Tamara Parvizi and Michael Bratt, Ph.D., for data entry and management; and George Reed, Ph.D., for statistical advice.
The inner city MBSR program was based at the Medical Center's City Campus, and operated in conjunction with the Family Health and Social Services Center, a long-standing neighborhood health center located within that complex. Other inner city health and social service centers referring to the clinic included: Great Brook Valley Health Center; Community Health Link; Worcester Aids Project; UMass Medical Center; UMass Interpreter Services; Catholic Charities; Worcester Youth Guidance; Day Break Shelter for Battered Women (YWCA); D.S.S. (Department of Social Services); Worcester Department of Corrections; Centro Las Americas; Salvation Army; Lipton Center (Fitchburg); Private health care providers and social workers. The first three were the source of eighty percent of all referrals.