While conventional wisdom has always affirmed the value of animals in promoting human health and well-being, only recently has their therapeutic role in medicine become a topic for dedicated research. Animal assisted interventions (AAI) can be classified as animal-assisted activities, animal-assisted therapy, and service animal programmes.
ObjectiveThe aim of this review is to analyse original papers addressing AAI and neurological diseases and published in the most influential medical journals between 2001 and 2012, and discuss their findings in the light of what may be of interest in the field of neurology.
DiscussionWe selected a total of 23 articles on neurorehabilitation in cerebral palsy, pervasive developmental disorders, multiple sclerosis, spinal cord injury, stroke, and mental disorders. The main therapeutic results were improvement on the Gross Motor Function Classification Scale and in upper limb dexterity (cerebral palsy); improvement in social functioning and interaction; reductions in stress, anxiety, and loneliness (pervasive developmental disorders and mental disorders); and decreased spasticity with improved balance (multiple sclerosis, spinal cord injury, stroke).
ConclusionThese interventions, performed with highly specialised animals in very specific neurological populations, deliver an increasing body of scientific evidence suggesting that they are an effective complement to other existing therapies. In these diseases, further high-quality studies are warranted in order to define the most appropriate programmes for therapy.
Aunque siempre se ha afirmado el valor de los animales en la promoción del bienestar y la salud del ser humano, solo recientemente su papel terapéutico en medicina se ha convertido en el foco de investigación especializada. Las intervenciones asistidas por animales pueden dividirse en actividades asistidas por animales, terapia asistida por animales y programas de animales de servicio.
ObjetivoEl objetivo de esta revisión es analizar las publicaciones realizadas entre 2001 y 2012 en las revistas médicas más importantes, relacionadas con el campo de la rehabilitación de las enfermedades neurológicas, y discutir estos hallazgos a la luz de lo que pueda ser de interés para la neurología.
DiscusiónSe seleccionaron un total de 23 artículos de intervenciones en el campo de la parálisis cerebral infantil, trastornos generalizados del desarrollo, esclerosis múltiple, lesión medular, accidente cerebrovascular y trastornos mentales. Los principales resultados terapéuticos fueron: mejoría en la Gross Motor Function y en el manejo del miembro superior (parálisis cerebral infantil); aumento de la socialización y el contacto con el medio ambiente, reducción del estrés y la ansiedad y sentimientos de soledad (trastornos generalizados del desarrollo y trastornos mentales); disminución de la espasticidad y mejoría del equilibrio (esclerosis múltiple, lesión medular, accidente cerebrovascular).
ConclusionesEstas intervenciones asistidas con un tipo de animales muy limitado utilizadas en grupos clínicos neurológicos muy específicos muestran cada vez más pruebas científicas, como método complementario a otras terapias ya existentes. En estas enfermedades, se necesitan más estudios de alta calidad metodológica que permitan definir los programas más apropiados para la aplicación terapéutica.
Animal-assisted interventions (AAI) provide a recent treatment alternative which is showing promising results in neurorehabilitation.1–3 Due to lack of formal regulation and the sometimes recreational nature of these activities, many health professionals remain sceptical about their efficacy. Nevertheless, in the United States and most of all in northern Europe this type of therapy has begun to be implemented in a regulated and systematic way to deliver concrete results. Methods specific to health science studies have been used, and the results have been published in scientific journals4 and book chapters.5,6 The term ‘neurorehabilitation’ describes the process aimed at reducing the impairment, limitations on activity, and restrictions experienced by a patient with a neurological disease. Its ultimate objective is reducing that patient's degree of functional impairment. Several therapies can be used to this end, and AAI is only one of the possible options.
At this point, we should clarify the terminology used in this article. AAI techniques can be classified into animal-assisted therapy (AAT), animal-assisted activities (AAA), and service animal programmes (SAP).7 AAT is a formal intervention with precise therapeutic objectives in which the animal acts as a co-therapist. It is targeted for a specific diagnosis and forms part of a rehabilitation programme coordinated by a multidisciplinary team that records the patient's progress in his or her medical history and assesses the results. AAAs are activities that involve support from animals that meet specific requirements. Since activities are informal, they are characterised by a certain degree of flexibility and spontaneity. Their purpose is to achieve interaction between patient and animal, thereby stimulating the patients’ social skills, motivation, learning, and other areas that may have a positive impact on quality of life. Lastly, SAPs use animals trained to help patients with physical disabilities overcome their functional difficulties in performing activities of daily life (ADL).
The benefits of AAI are still subject to debate. It is therefore important to explain the results of studies conducted to date by professionals in this field.
Our purpose is to present a systematic review of the published articles addressing AAI and discuss their findings with particular attention to what may be of interest for neurorehabilitation. To this end, we included 23 articles meeting the strict inclusion criteria for this review, i.e. having been published in the most influential indexed medical journals between 2001 and 2012.
DevelopmentWe conducted a literature search for only those original clinical studies published between 2001 and 2012 in indexed journals. The search used the databases PubMed and Thomson Reuters Journal Citation Reports (JCR, including Science Edition and Social Sciences Edition). The keywords used in all fields were ‘animal assisted therapy’ OR ‘animal assisted activities’ OR ‘service animals’ OR ‘equine-assisted therapy’ OR ‘hippotherapy’ OR ‘therapeutic horseback riding’ OR ‘pet therapy’ OR ‘service dogs’. We excluded articles published in languages other than English and any whose content was not related to neurorehabilitation. We also excluded articles published in veterinary journals and those exclusively analysing human physiochemical responses or the effect of simulators or virtual animals.
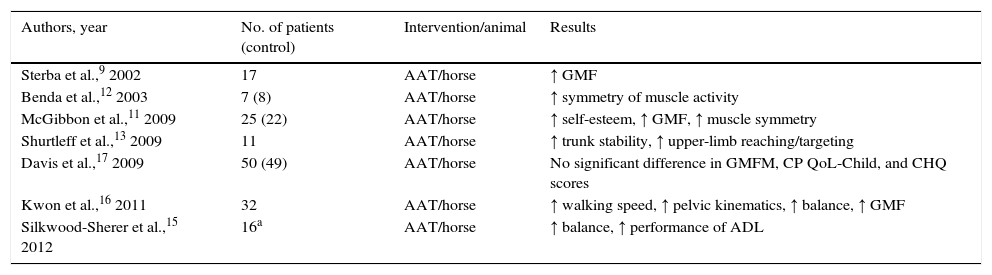
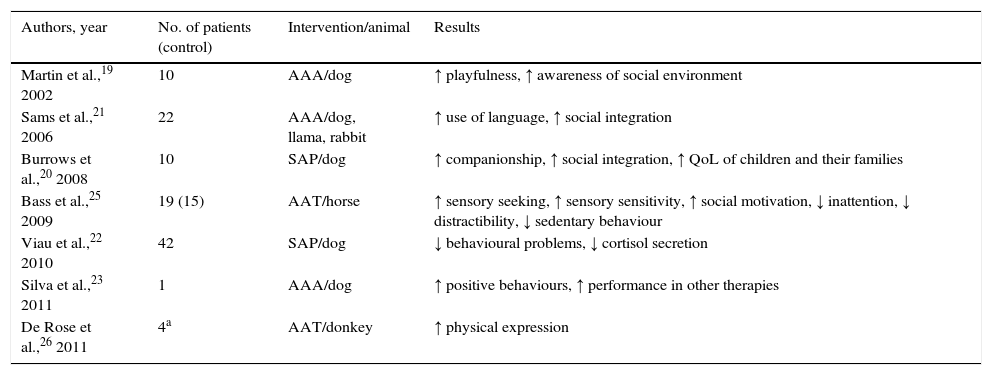
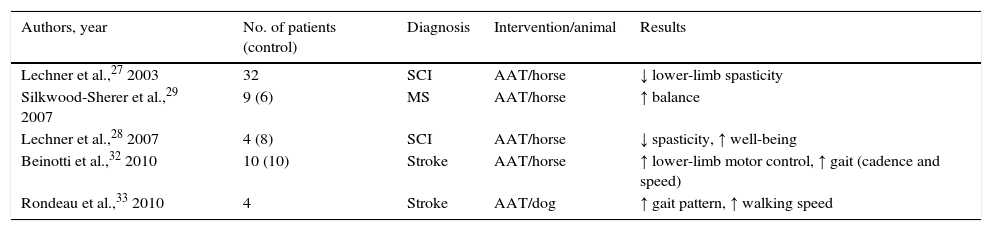
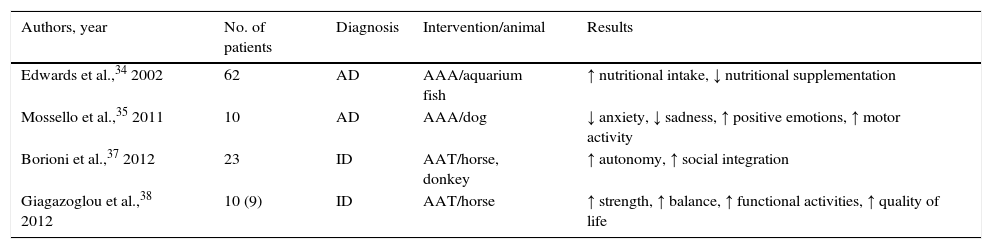
A total of 23 articles met our strict inclusion criteria. Results were grouped according to the type of neurological disease for which participants underwent neurorehabilitation. Table 1 shows the results of 7 articles mainly addressing cerebral palsy (CP). Table 2 lists 7 articles on neurorehabilitation for patients with pervasive developmental disorders (PDD), including autism. In Table 3, we can find 5 articles addressing spasticity-related neurological diseases in adults: multiple sclerosis (MS), spinal cord injury (SCI), and stroke. Lastly, Table 4 presents 4 articles on patients with dementia or intellectual disability (ID).
Studies addressing animal-assisted interventions in children with cerebral palsy
| Authors, year | No. of patients (control) | Intervention/animal | Results |
|---|---|---|---|
| Sterba et al.,9 2002 | 17 | AAT/horse | ↑ GMF |
| Benda et al.,12 2003 | 7 (8) | AAT/horse | ↑ symmetry of muscle activity |
| McGibbon et al.,11 2009 | 25 (22) | AAT/horse | ↑ self-esteem, ↑ GMF, ↑ muscle symmetry |
| Shurtleff et al.,13 2009 | 11 | AAT/horse | ↑ trunk stability, ↑ upper-limb reaching/targeting |
| Davis et al.,17 2009 | 50 (49) | AAT/horse | No significant difference in GMFM, CP QoL-Child, and CHQ scores |
| Kwon et al.,16 2011 | 32 | AAT/horse | ↑ walking speed, ↑ pelvic kinematics, ↑ balance, ↑ GMF |
| Silkwood-Sherer et al.,15 2012 | 16a | AAT/horse | ↑ balance, ↑ performance of ADL |
ADL: activities of daily life; GMF: gross motor function; AAT: animal-assisted therapy; ↑: improvement or increase.
Studies addressing animal-assisted interventions in children with pervasive developmental disorders
| Authors, year | No. of patients (control) | Intervention/animal | Results |
|---|---|---|---|
| Martin et al.,19 2002 | 10 | AAA/dog | ↑ playfulness, ↑ awareness of social environment |
| Sams et al.,21 2006 | 22 | AAA/dog, llama, rabbit | ↑ use of language, ↑ social integration |
| Burrows et al.,20 2008 | 10 | SAP/dog | ↑ companionship, ↑ social integration, ↑ QoL of children and their families |
| Bass et al.,25 2009 | 19 (15) | AAT/horse | ↑ sensory seeking, ↑ sensory sensitivity, ↑ social motivation, ↓ inattention, ↓ distractibility, ↓ sedentary behaviour |
| Viau et al.,22 2010 | 42 | SAP/dog | ↓ behavioural problems, ↓ cortisol secretion |
| Silva et al.,23 2011 | 1 | AAA/dog | ↑ positive behaviours, ↑ performance in other therapies |
| De Rose et al.,26 2011 | 4a | AAT/donkey | ↑ physical expression |
AAA: animal-assisted activities; AAT: animal-assisted therapy; SAP: service animal programmes; ↑: improvement or increase; ↓: decrease.
Studies addressing animal-assisted interventions in adults with pyramidal syndrome
| Authors, year | No. of patients (control) | Diagnosis | Intervention/animal | Results |
|---|---|---|---|---|
| Lechner et al.,27 2003 | 32 | SCI | AAT/horse | ↓ lower-limb spasticity |
| Silkwood-Sherer et al.,29 2007 | 9 (6) | MS | AAT/horse | ↑ balance |
| Lechner et al.,28 2007 | 4 (8) | SCI | AAT/horse | ↓ spasticity, ↑ well-being |
| Beinotti et al.,32 2010 | 10 (10) | Stroke | AAT/horse | ↑ lower-limb motor control, ↑ gait (cadence and speed) |
| Rondeau et al.,33 2010 | 4 | Stroke | AAT/dog | ↑ gait pattern, ↑ walking speed |
MS: multiple sclerosis; SCI: spinal cord injury; AAT: animal-assisted therapy; ↑: improvement or increase; ↓: decrease.
Studies addressing animal-assisted interventions in adults with dementia or intellectual disability
| Authors, year | No. of patients | Diagnosis | Intervention/animal | Results |
|---|---|---|---|---|
| Edwards et al.,34 2002 | 62 | AD | AAA/aquarium fish | ↑ nutritional intake, ↓ nutritional supplementation |
| Mossello et al.,35 2011 | 10 | AD | AAA/dog | ↓ anxiety, ↓ sadness, ↑ positive emotions, ↑ motor activity |
| Borioni et al.,37 2012 | 23 | ID | AAT/horse, donkey | ↑ autonomy, ↑ social integration |
| Giagazoglou et al.,38 2012 | 10 (9) | ID | AAT/horse | ↑ strength, ↑ balance, ↑ functional activities, ↑ quality of life |
AAA: animal-assisted activities; AAT: animal-assisted therapy; ↑: improvement or increase; ↓: decrease.
Over the last decade, numerous published articles have addressed the therapeutic role of animals in medicine. However, few of them were indexed in both PubMed and JCR databases. The terminology used in the field of AAI is still inconsistent, especially among the first published articles. The classification we have adopted has been widely accepted in recent years, and it seems to avoid the main causes of misunderstandings.
While many factors that can lead to success in AAI, the most relevant ones are proper animal and patient selection, and implementation of the programme by appropriately trained personnel after developing protocols with realistic objectives.8 We should underline here the ethical importance of treating animals appropriately, respecting their rest periods, and avoiding stressful situations.
In this review we present a discussion of the results grouped in the 4 categories already mentioned and reflected in Tables 1–4.
Animal-assisted interventions in children with cerebral palsy (Table 1)Horses (hippotherapy) are the animals preferred for use in the neurorehabilitation of children with CP. An article by Sterba et al.9 found improvements in gross motor function (GMF). In a subsequent review,10 the same author stated that evidence published to date showed improved gross motor function despite the 2 methodological limitations of the articles included in the review (namely small sample sizes and the lack of control groups). These improvements in GMF were corroborated by McGibbon et al.11 These authors pointed out that hippotherapy can help reestablish muscle symmetry, a finding that was also reported in an article by Benda et al.12 Improvements in trunk stability permit patients to free their upper limbs, which they had previously depended on for support. Upper limbs can also be rehabilitated in this way, resulting in improvements in reaching and targeting.13 The positive effects of hippotherapy were also reviewed in a more recent meta-analysis including 8 published articles rated according to methodological quality.14 Conclusions from this meta-analysis are similar to those from our own study: hippotherapy appears to improve postural control and balance. However, these findings cannot be generalised due to the small sample size. One of the main problems in CP is spasticity and how to treat that symptom non-surgically. Hippotherapy in combination with other types of interventions may therefore be a valuable method. Silkwood-Sherer et al. conducted a study on children with different neurological diseases involving movement disorders and balance problems. They reported balance improvements and better functional performance of ADL in children with mild to moderate movement disorders.15 However, the authors indicated that their study had some methodological limitations, mainly the lack of a control group and the short period between baseline assessments. Another study published in 2011 supports these conclusions. This trial, conducted in 32 children with bilateral spastic cerebral palsy, found that hippotherapy (30min twice weekly for 8 consecutive weeks) significantly improved walking speed, pelvic kinematics, balance, and Gross Motor Function Measure (GMFM) scores.16 While some authors were not able to corroborate these findings,17 they attribute the lack of statistically significant results to the poor sensitivity of the measurement instruments. In fact, quality of life and health measurement tools are not yet shown to be sensitive enough to detect changes in children with CP. A review article by Tseng et al.18 also points out the lack of significant differences in the effect of long-term hippotherapy (total riding time: 8-22h) compared to short-term hippotherapy (total riding time: 8-10min).
Animal-assisted interventions in children with pervasive developmental disorders (Table 2)PDDs, also known as autism spectrum disorders (ASD), have a poor prognosis since they cannot currently be cured. A possible therapeutic option can be found in psychoeducational intervention models, which include AAT. Although we found numerous articles describing the beneficial effects of animals on patients with a PDD, only 7 of them met the inclusion criteria for this review. As Martin and Farnum state,19 animals promote communication and awareness of social environment in children with PDD. In their study of children with PDD and dogs, the children were exposed to 3 different conditions: (a) a non-social toy, (b) a stuffed dog, and (c) a live dog. Children were more interested in playing and more focused, and they showed more awareness of their social setting, in the presence of a live dog. According to Burrows et al.,20 service dogs can help autistic children and their families in 3 different ways: (a) in its role as a watchdog, it promotes the child's safety; (b) the feeling of safety allows for more freedom and promotes family outings and activities, and (c) the presence of a service dog increases awareness of autism and social interaction, therefore improving social recognition and status. A study by Sams et al.21 also showed improved social integration and a greater use of language. Service dogs have also been linked to physiological changes, in the form of less stress evidenced by lower cortisol levels. One study22 evaluated cortisol levels in 42 autistic children before and during service dog therapy in families, and after therapy had ended. Two weeks prior to introducing service dogs, peak cortisol levels after awakening reached 58% (maximum levels in non-autistic people range from 30% to 40%). However, once service dogs were introduced in the families, cortisol levels dropped to 10%, and 4 weeks later, when dogs had been removed, morning cortisol levels jumped to 48%. The authors found no changes in diurnal cortisol levels. In addition to this, parents reported fewer behavioural problems in their children after the arrival of the service dogs. Although the underlying mechanism is yet to be understood, scientific evidence suggests that dogs reduce stress in humans. It is clear that these behavioural improvements can have a positive impact on children's performance in other types of therapy. Silva et al.23 conducted study in a single patient, a 12-year-old boy with PDD, who was evaluated in 2 situations: (a) one-to-one structured therapeutic activities with a therapist assisted by a service dog, and (b) one-to-one structured activities with the same therapist alone (control scenario). When performing activities in the presence of the dog, the child showed more positive behaviours (smiling, long-lasting physical contact) and less frequent and shorter-lasting negative behaviours (aggression). Dogs are therefore a potential tool for promoting mental health.24
Hippotherapy has also been used in patients with PDD with satisfactory results. Bass et al.25 conducted a study in 19 autistic children. The group exposed to hippotherapy experienced greater interaction, sensory seeking, and social motivation, and less inattention, distractibility, and sedentary behaviours, compared to the control group. These positive results have also been achieved with donkey-assisted therapy.26 Donkeys help improve psycho-affective and psycho-cognitive skills in autistic children. An added benefit is that compared to horses, their size is less intimidating. This study also showed that participants relied more on physical expression than on verbal language when communicating with the animal.
Animal-assisted interventions in adults with pyramidal syndrome: stroke, multiple sclerosis, and spinal cord injury (Table 3)Hippotherapy was used in 4 of the selected studies (1 on stroke, 1 on MS, and 2 on SCI). These studies evidenced decreased spasticity in the lower limbs after treatment as the main result. The authors hypothesised that the rhythmic flexion and extension of the patient's trunk, along with trunk torsion, have a beneficial effect on spasticity. The overall psychosomatic influence exerted by this type of therapy is also believed to play an essential role. According to 2 studies, the spasticity-reducing effect of hippotherapy on SCI patients was immediate, although of short duration.27,28 Another study found similar results in patients with MS, as well as considerable improvements in balance.29 These studies also suggest that hippotherapy is a multimodal therapeutic option with positive effects on all levels described in the International Classification of Functioning, Disability, and Health. This is especially relevant for patients with MS. Hippotherapy promotes physical activity, therefore improving balance, gait, and performance of ADL.30 It also increases participation and constitutes an alternative for patients with reduced mobility, with the advantage of also being a recreational activity. Hippotherapy also provides substantial psychosocial benefits and improves quality of life significantly.31 In light of the above, hippotherapy seems to be a promising therapeutic tool for patients with MS, although further studies are needed to confirm this conjecture. The study by Beinotti et al. on stroke patients32 showed that hippotherapy can improve gait, especially by increasing independent ambulation, cadence, and speed. These findings coincide with results from patients with MS and appear to be due mainly to improvements in trunk control that contribute to better balance.
The fifth study in Table 3 adopted the innovative approach of using a dog for rehabilitation and gait retraining in stroke patients. This pilot study included 4 patients who underwent a 3-week training period aimed at retraining gait with the aid of a dog.33 The dog served 2 purposes: to retrain gait and to act as a walking aid. Patients had recently suffered a stroke and presented hemiparesis. By the end of the study period, all of them showed improvements in their gait patterns and walked considerably faster with the dog than with a cane.
Animal-assisted interventions in patients with dementia or intellectual disability (Table 4)Two studies in our selection addressed patients with dementia. The study by Edwards and Beck34 introduced fish aquariums in the setting of patients with Alzheimer disease (AD), and the patients’ nutritional state improved such that they required less nutritional supplementation. Mosello et al.35 conducted another study on the benefits of dogs for AD patients attending a day-care centre. These patients experienced a decrease in anxiety and sadness as well as an increase in positive emotions and motor function. The review by Perkins et al.36 appears to confirm these findings. However, it also indicates the main methodological flaws of the studies included: none of them adopted a randomised design and several potentially important factors were not controlled for, such as the effect of dogs on caregivers, which can in turn influence the way caregivers treat and interact with patients. These authors also postulated that patients’ premorbid relationships with dogs can alter outcomes.
The remaining 2 studies in Table 4 addressed patients with ID. The first one of them proved that equestrian therapy is an effective rehabilitation alternative for patients with intellectual or learning disabilities.37 The movement of the horse or donkey and the non-clinical setting provoke physical, mental, social, communicative, and behavioural improvements. This study also showed that most patients with intellectual and neuromotor disabilities receiving equestrian or donkey-assisted rehabilitation therapy experienced an improvement in autonomy and social integration which persisted over time. These findings are consistent with the results shown in one study by Giagazoglou et al.38 In this study, several adolescents with ID attended a 10-week hippotherapy programme and experienced an improvement in limb strength and balance, which ultimately improved functional activities and quality of life.
ConclusionsThe present review includes only the most recent articles (2001-2012) published in the most influential scientific journals. As a result, our findings are restricted to very specific clinical groups that have interacted with a limited array of animals (mainly horses for AAT and dogs for AAA and SAP).
The main results of this review can be summarised as follows.
The animals most frequently used in AAT programmes were horses. We also found one study using donkeys and another with dogs. Therapy with horses (hippotherapy or therapeutic horseback riding) was shown to temporarily reduce spasticity in patients with MS, SCI, and stroke. It also improved balance in patients with MS. Hippotherapy improved GMF and manual dexterity in children with CP. AAI with both dogs and horses in patients with PDD resulted in better performance in conventional therapies.
The efficacy of AAT depends on the type of animal used, the setting where sessions take place, the duration of the intervention, the type of disorder and age of the patient, and whether sessions are individual or group sessions.39 Evaluating the effects of AAI is not an easy task due to the discrepancies in statistical results and additional feedback reported by parents, animal trainers, and health professionals. We should also mention a review by Pauw40 which states that studies on hippotherapy have important limitations derived from small sample sizes and the frequent lack of standardised measurement instruments.
AAAs, in turn, promote social skills; reduce stress, anxiety, and loneliness; improve mood; increase well-being; and help patients develop leisure skills. This is the result of a natural tendency by which some animals forge strong bonds with humans, thereby creating intense non-verbal communication. The articles assessing AAA included in this review used mainly dogs and fish, although other animals (petting animals, farm animals) may have promising results. Dogs in particular are friendly, they promote communication and interaction, and they also reinforce some positive behaviours in patients, such as throwing a ball, walking, using non-verbal responses, etc.
In general terms, these studies yield heterogeneous results that cannot be easily evaluated due to their small sample sizes, selection biases, and the lack of a control group. Randomised samples, a better selection of measurement tools, and a longer follow-up period after treatment would be advisable. In addition to this, some external factors (for example, other therapies) may have altered the results, although interrupting other therapies during a study would not be an ethical solution. Not all problems can be solved easily. Nevertheless, a deeper understanding of the situation can help us find appropriate solutions.
Our findings derive from the analysis of a list of articles meeting strict inclusion criteria. They are in line with the published literature that can be found in PubMed and Google Scholar and which has been discussed in recent reviews that have examined books, theses, congress papers, abstracts, and articles published in journals not indexed in the most influential scientific databases. Although these findings reflect the results of AAI with a limited array of animals used in therapy for very specific disorders, they also provide increasing scientific proof that these interventions work as complementary tools for other established types of therapy. Further studies with a high methodological quality are necessary to determine the most appropriate therapeutic programmes for the disorders mentioned in this review.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Muñoz Lasa S, Máximo Bocanegra N, Valero Alcaide R, Atín Arratibel MA, Varela Donoso E, Ferriero G. Intervenciones asistidas por animales en neurorrehabilitación: una revisión de la literatura más reciente. Neurología. 2015;30:1–7.