The effectiveness of endovascular treatment for acute stroke is well established.1 International treatment guidelines recommend endovascular treatment for patients with proximal intracranial artery occlusions and NIHSS scores≥6.2 However, patients with proximal occlusions may initially score low on the NIHSS before the collapse of compensatory mechanisms and the onset of the severe symptoms usually associated with large-vessel occlusions.
We present the case of a patient arriving at the emergency department with ischaemic stroke, scoring 1 on the NIHSS. She had a thrombus in the terminal segment of the right internal carotid artery (ICA) and extending up to the M1 segment of the middle cerebral artery (MCA), which was extracted by mechanical thrombectomy.
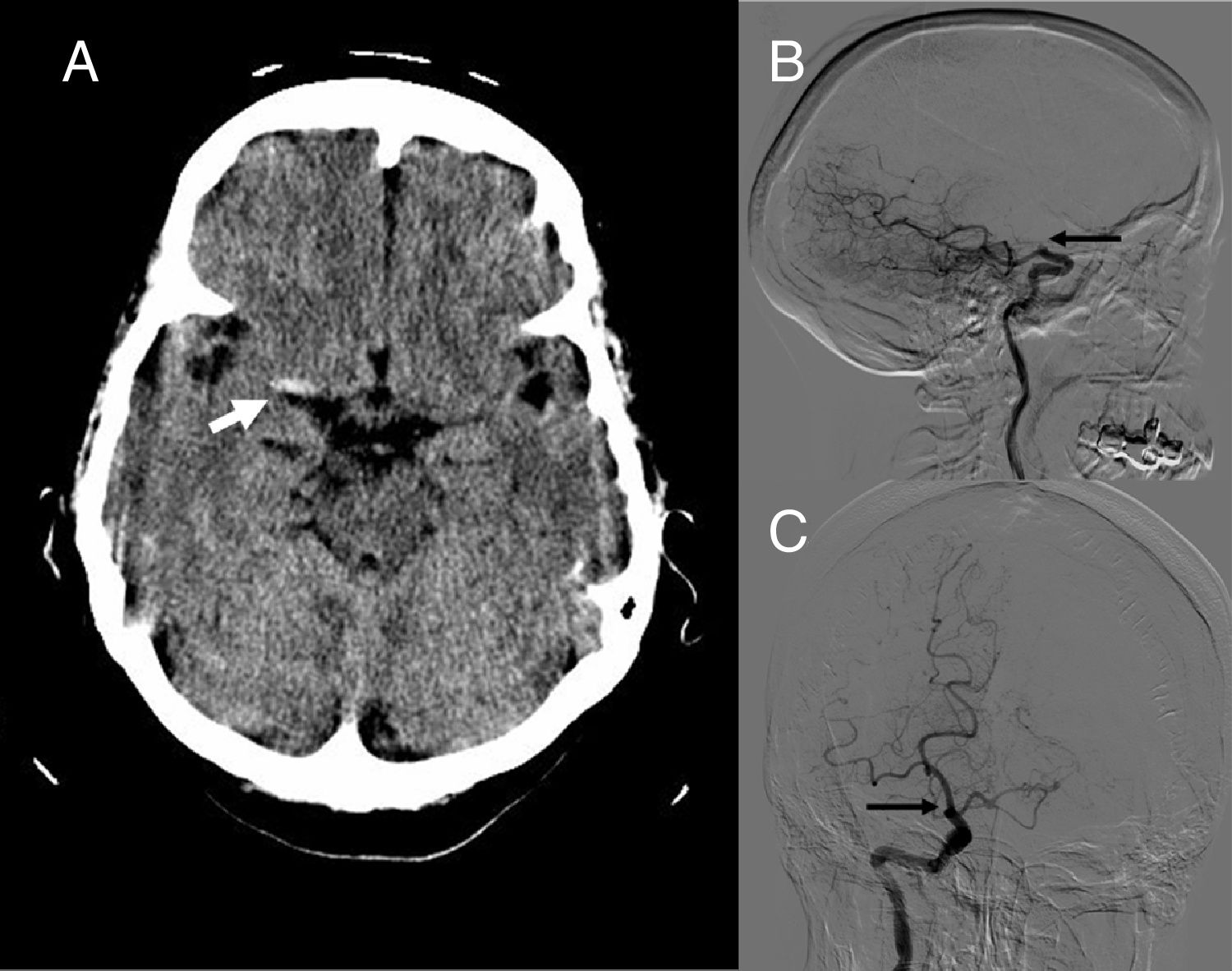
Clinical caseThe patient was a 71-year-old woman with arterial hypertension and a history of atrial fibrillation managed with acenocoumarol. She was transported to the emergency department due to sudden onset 2h earlier of difficulty uttering words, a tingling sensation in the left leg, and mild weakness in the left arm and leg. The neurological examination revealed mild paresis of the left leg and an NIHSS score of 1. A blood analysis showed an INR of 2.07. An emergency head CT scan revealed a hyperdense area in the right MCA (Fig. 1A), with no other signs of acute ischaemia or intracranial haemorrhage (ASPECTS score of 10). CT angiography revealed occlusion of the terminal segment of the right ICA.
(A) Non-contrast head CT scan showing the “hyperdense middle cerebral artery sign” (arrow), suggestive of a thrombus at this level. Sagittal (B) and coronal (C) sections from the digital subtraction angiography study, revealing an obstruction to contrast flow in terminal internal carotid artery above the exit of the posterior communicating artery (arrow).
Symptoms worsened during the patient's transfer to the operating theatre for neurointerventional surgery: she displayed left inferior homonymous quadrantanopia, left supranuclear facial palsy, left arm hypoaesthesia, and mild left-sided hemiparesis (NIHSS 5). Angiography confirmed the results of the CT angiography study (Fig. 1B and C); the thrombus was extracted by stent-retriever mechanical thrombectomy, achieving complete recanalisation (TICI 3) after a single pass.
The patient was asymptomatic (NIHSS 0) the following day and remained so until discharge.
DiscussionThe American Heart Association clinical guidelines establish a minimum NIHSS score of 6 for patients with acute ischaemic stroke to be eligible for endovascular treatment (class I, level of evidence A).2 However, occlusions of large intracranial arteries may be associated with low NIHSS scores. In the study by Maas et al.,3 29% of patients with an initial NIHSS score of 0 had proximal occlusions. This may be due to the fact that symptoms of ischaemic stroke appear when cerebral blood flow drops below 18-22mL/100g/min,4 but such dynamic systems as arteriolar vasodilation and collateral circulation maintain cerebral blood flow above that threshold.
In 62%-71% of cases, these mechanisms eventually fail if blood flow is not restored in the artery involved, leading to symptom worsening and an increase in the size of the infarction.5–7
Intravenous fibrinolysis only achieves complete recanalisation of proximal occlusion in up to 30% of cases; the likelihood of spontaneous recanalisation is even lower. Bhogal et al.8 and Pfaff et al.9 studied the effectiveness of mechanical thrombectomy in patients with low NIHSS scores and report a median thrombus length of 12mm (interquartile range, 10-12) and a mean length of 10mm (range, 4.6-23.1), respectively. There is an extremely low likelihood of achieving recanalisation with intravenous fibrinolysis for thrombus lengths exceeding 8mm.10
Performing mechanical thrombectomy in patients with proximal occlusion and presenting low NIHSS scores would improve outcomes: once collateral circulation collapses, symptoms worsen and infarction size increases at a faster pace than at stroke onset, since compensatory mechanisms are already exhausted.
Our patient's symptoms worsened during transfer to the operating theatre: she had an NIHSS score of 5 in the minutes before the intervention, probably since compensatory mechanisms were collapsing.
Regarding functional prognosis, in the study by Bhogal et al.8 (patients with M1 MCA occlusion and NIHSS scores≤5 receiving endovascular treatment), around 75% of patients scored≤2 on the modified Rankin Scale (mRS) at 3 months. A good functional prognosis is to be expected in our patient, since she was asymptomatic at discharge (mRS 0).
Revascularisation should be considered in all patients with proximal occlusions arriving early at the hospital, regardless of NIHSS score.
Please cite this article as: Tejada Meza H, Martínez García R, Capablo Liesa JL, Marta Moreno J. Anticipándonos al desastre: trombectomía mecánica en paciente con NIHSS bajo. Neurología. 2019;34:350–351.