We present the clinical case of a 54-year old man with initial symptoms of radicular pain in the lower limbs (LL) which had been progressing for 2 weeks. This was associated with paraesthesia of the hands and feet. The baseline examination showed radicular pain and a tactile and pain sensory deficit with stocking and glove distribution. The gradual progression of bilateral radicular pain symptoms associated with asymmetrical weakness in the LL, which prevented the patient from standing and walking in the following weeks, led to him being hospitalised to undergo a comprehensive evaluation.
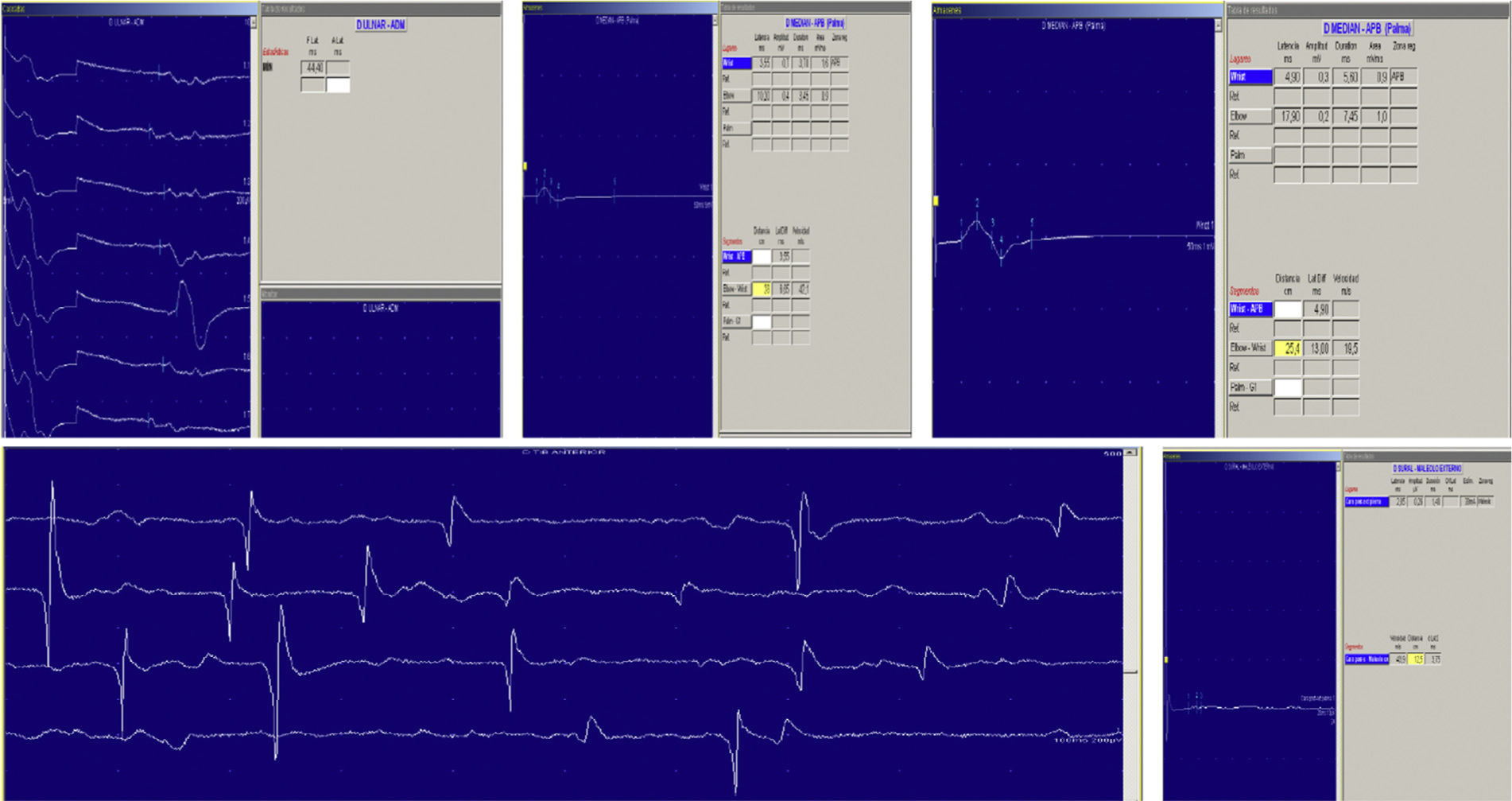
The patient's medical history revealed signs of viral enteritis appearing several days or weeks before pain onset. Neurological examination showed, on the right foot, muscle strength of 0/5 on dorsiflexion and 2+/5 on plantar flexion; on the left foot, muscle strength was 2/5 on dorsiflexion and 3+/5 on plantar flexion. Deep tendon reflexes were also asymmetrical, and patellar reflexes in both legs were present but hypoactive. We recorded abolished right ankle reflex and hypoactive left ankle reflex. The sensory exam showed an asymmetrical sensory deficit. The patient experienced pain when standing and walking was initially impossible; analgesics (including morphine derivatives) were necessary to control pain. Additional laboratory testing included a complete blood test which yielded no relevant findings, and serology tests that were positive for antibodies to Campylobacter jejuni. The cerebrospinal fluid test revealed albuminocytologic dissociation, and the neurophysiological study showed presence of subacute polyradiculoneuritis with sensory and motor impairment that was predominantly axonal and asymmetrical in UL and LL (Fig. 1).
We observed a very slow initial improvement after medical treatment and rehabilitation. Symptoms later relapsed with exacerbated motor impairment associated with autonomic dysfunction (tachycardia, excessive sweating), in addition to abdominal symptoms with bloody diarrhoea and a parallel increase in acute-phase reactants (PCR, VSG). We performed a colonoscopy that showed presence of non-necrotising epithelioid microgranulomas and deep ulcer compatible with Crohn disease-type inflammatory bowel disease (IBD).
A new course of immunotherapy and rehabilitation was started, as well as symptomatic treatment with mesalazine, which delivered limited improvements. Another neurological relapse associated with abdominal symptoms raised questions about a possible association between the two entities (acute sensory motor axonal neuropathy [ASMAN] and IBD). To investigate a potential common pathogenic factor, we performed a biopsy of the peripheral nerve to study the myelin sheath and complete a histochemical study and blood vessel assessment.
We observed a very severe loss of myelinated nerve fibres in all fascicles, with scarcely any intact myelinated axons and extensive Wallerian degeneration. There were no alterations in the myelin sheath, and epineural medium-sized vessels presented a normal appearance.
Six months later, symptoms remained more or less unchanged, and doctors performed new neurophysiological and intestinal studies. An electromyography was compatible with severe chronic motor sensory polyradiculoneuritis that was predominantly axonal and distal, with little reinnervation. Follow-up colonoscopy showed colonic mucosa with a normal appearance. Biopsies confirmed mild non-specific colitis, showing no activity or evidence of previous symptoms.
This clinical case is interesting because its course was marked by neurological relapses associated with digestive problems, as well as colonoscopy abnormalities typical of Crohn disease-type IBD which disappeared as the patient's condition improved. Also to be highlighted is the chronic course followed by the peripheral nervous system disorder.
Cases in which C. jejuni infection is associated with Guillain–Barré syndrome have been linked to an immunological basis.1,2
This infection can lead to symptomatic acute inflammatory disease. Some studies mention its relationship with IBD, since it is frequently isolated in patients with a recent diagnosis of Crohn disease. This point remains to be clarified, since other studies did not find any significant differences in Campylobacter presence between patients and healthy subjects.3
IBD can be associated with neurological manifestations, which are usually caused by the activity of the intestinal disease but may also be independent from that entity. Some animal studies mention the theory that presence of bacterial infection may act as an immunological trigger.4
Lastly, autoimmune diseases involving organs not belonging to the nervous system have been known to remit with immunomodulatory treatments, such as immunoglobulins, for autoimmune polyradiculoneuropathies.5
In our hypothesis, C. jejuni infection plays a fundamental role since it would be responsible for the immune dysregulation which can cause both neurological and intestinal involvement. Remission of intestinal involvement might have been the result of overdiagnosis (diagnosing an acute infectious intestinal disease as IBD) or of immunotherapy.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Gabaldón-Torres L, Jordan M, Osorio-Caicedo P, Badía-Picazo MC, Salas-Felipe J. Polirradiculoneuritis aguda sensitivo-motora axonal autoinmune en el seno de una enfermedad inflamatoria intestinal. Neurología. 2015;30:586–587.
This study was partially presented at the SEN Annual Meeting, November 2012.