Charcot-Marie-Tooth disease (CMT) is one of the most complex neurological syndromes, and presents a prevalence of 28.2 cases/100 000 population in Spain. CMT type 4C, which accounts for 18% of cases, is characterised by clinical symptoms of demyelinating neuropathy following an autosomal recessive inheritance pattern, and is more prevalent among people of Roma descent.2,3,6,8 It is caused by a biallelic mutation of the SH3TC2 gene, located on chromosome 5q32, which participates in encoding a membrane protein of Schwann cells, involved in endocytic recycling through the Rab11 GTPase system.2–4,7,8 PCR and ELISA studies have detected the SH3TC2 protein in the tissues of the brain, spinal cord, cardiac muscle, testes, lungs, liver, skeletal muscle, kidneys, pancreas, ovaries, and spleen.4,7 We describe the case of a patient with CMT type 4C and vertebral artery dissection.
The patient was a 37-year-old woman of Roma descent, born to consanguineous parents, who was under follow-up due to diagnosis of CMT type 4C (SH3TC2 mutation p.R1109X in homozygosis). She visited the emergency department due to neck pain and sudden worsening of gait instability, a week after undergoing a cervical traction manoeuvre due to moderate cervical pain.
Neurological examination revealed severe dysarthria; persistent horizontal nystagmus in all gaze positions; right-sided trigeminal hypoaesthesia and facial palsy; deviation of the tongue to the right side; paresis and dysmetria of the right arm; and unstable, wide-based gait with a tendency to veer to the right. The patient scored 6 on the National Institutes of Health Stroke Scale. We initially suspected vertebrobasilar stroke presenting as right bulbo-pontine syndrome.
An emergency blood analysis (complete blood count, coagulation profile, electrolyte study, glycaemia, and kidney and liver function), ECG, and head CT identified no alterations. A CT angiography of the supra-aortic arteries (Fig. 1) identified reduced calibre of the right V2 and left V3 segments of the vertebral artery, without filling of the posterior inferior cerebellar artery (PICA), and a filling defect in the proximal third of the basilar artery, with distal filling; these findings are compatible with bilateral vertebral artery dissection and non-occlusive thrombosis of the proximal basilar artery.
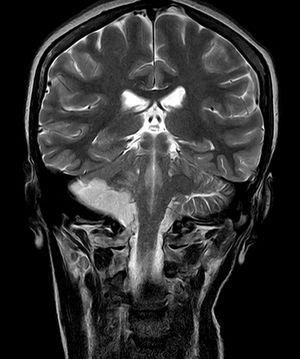
We requested further testing, including a lipid profile, vitamins, thyroid function, total protein test, autoimmunity, and serology studies, as well as a transoesophageal echocardiography study and 24-hour Holter ECG monitoring; all studies yielded normal results. A follow-up head CT study performed at 24 hours identified subacute infarction in the territory of the right anterior-inferior cerebellar artery (AICA) and PICA, with no haemorrhagic transformation or mass effect. The brain MRI (Fig. 2) and angiography studies detected infarction at different times of the AICA and PICA territories, affecting the fifth, seventh, and eighth cranial nerve nuclei, and mural thrombosis of the right proximal basilar artery and vertebral artery segments V3 and V4 (stenosis of 50% and 75%, respectively), and confirmed vertebral artery dissection, with arterial wall irregularities compatible with dysplasia in the left V2 segment.
The patient progressed favourably, with persistence of the right hypoaesthesia and facial palsy, and scored 1 on the modified Rankin Scale at discharge. We prescribed 100 mg acetylsalicylic acid and 80 mg atorvastatin for secondary prevention of ischaemic stroke. A thrombophilia study performed at 3 months of follow-up detected no alterations, and an MRI angiography study performed at 6 months identified no new lesions and no signs of dissection.
DiscussionLittle evidence is available on the relationship between CMT variants and arterial wall abnormalities. The only association reported to date is the involvement of mutations of SMAD3 (15q22), COL3A1 (2q32), and TNXB (6p21), participating in TGF-beta signalling pathways and the synthesis of type III collagen and tenascin X, which are related to Ehler-Danlos syndrome.1 These mutations are associated with dissections, dilation, and tortuosity of the cervical arteries in up to 78% of cases, and of the thoracic aorta in up to 75%, with only 68% of patients presenting neurological symptoms. Studies of related patients describe CMT2-like sensory-motor axonal neuropathy in fewer than 50% of cases.1,5 None of these present the typical mutations associated with CMT2 (GJB1, MPZ, and GDAP 1).1,5
A systematic literature review identified no reports of CMT type 4 associated with arterial wall abnormalities or detection of the SH2TC2 protein in the peripheral nerves with the tests used. However, given the evidence of other CMT-like variants and the importance of differential diagnosis in young patients with stroke due to the special management required, we deem it important to report this case within such a heterogeneous disease as CMT, which suggests the possibility that structural alterations to the walls of the cervical arteries may play a causal role.
Please cite this article as: López Anguita S, Iglesias Mohedano AM, Palacios Mendoza MA, Muñoz Blanco JL. Charcot-Marie-Tooth 4C y disección vertebral bilateral: ¿relación causal o coincidente? Neurología. 2021;36:643–644.