Choreic syndromes are movement disorders that may be associated with inherited, metabolic, infectious, neurodegenerative, autoimmune, or iatrogenic diseases.1 They are rarely associated with neoplasia and account for 1% of all paraneoplastic processes.2
We present the case of a 62-year-old woman who in the course of one month experienced gait instability, emotional lability, and behavioral disorders, including disinhibition and verborrhea. The patient reported a weight loss of 20kg in the previous 2 months. The examination revealed choreiform movements which distorted voluntary movements symmetrically in the limbs, trunk, and neck. These movements disappeared at rest and were exacerbated by stress. She displayed astasia and unstable gait, but no ataxia or wide-based stance. Muscle tone was normal; no bradykinesia or dystonia were observed. She had preserved reflexes and muscle balance, and there were no signs of pyramidal dysfunction. Likewise, the patient showed no dysmetria or sensory disorders.
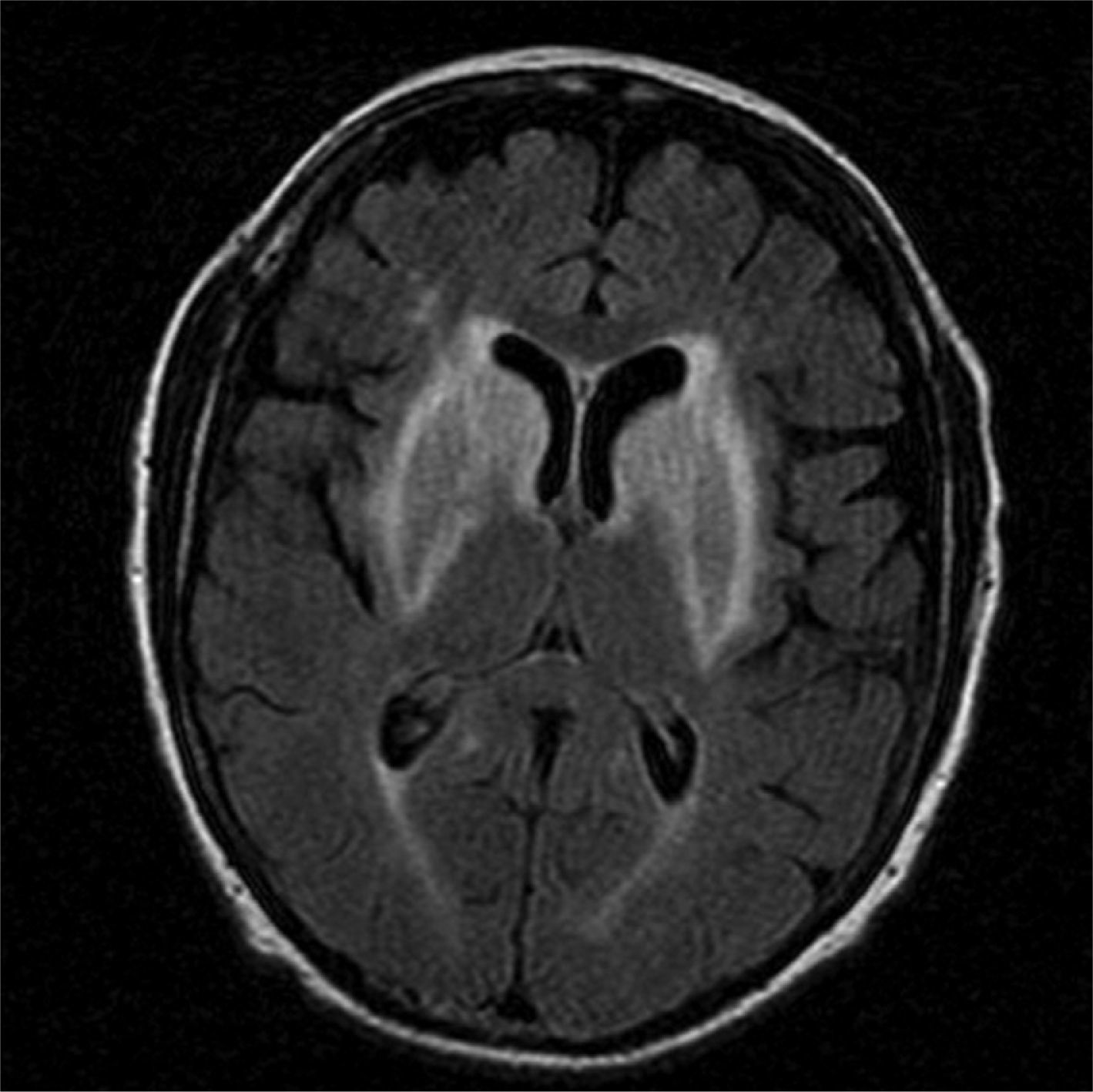
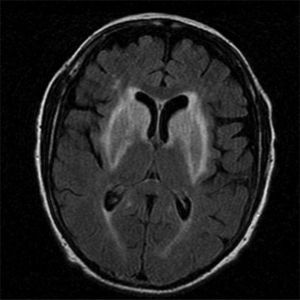
Complementary data included a brain MRI scan showing symmetrical abnormalities in both striate nuclei and the anterior limbs of both internal capsules, appearing as increased signal intensities on FLAIR and T2-weighted sequences. There were no hyperintensities on DWI sequences or signal alterations on T1-weighted sequences (Fig. 1).
We performed a complete metabolic study including the ischaemic lactate-ammonia test, copper and ceruloplasmin tests, and a liver function test. All results were normal. The patient underwent several serology tests. The FTA test displayed high antibody titers; results were negative for RPR. Findings from HIV and hepatitis B and C serology tests were also negative.
CSF revealed pleocytosis (38 lymphocytes/mL); glucose, protein, ADA, and lactic acid levels were within normal ranges. Findings from a CSF culture and VDRL test were negative. Cytology and flow-cytometry showed no neoplastic cellularity. The Western blot test revealed presence of a band corresponding to anti-CV2/CRMP5 antibodies; the test was negative for anti-Hu antibodies.
A thoracic-abdominal CT showed presence of mediastinal, right paratracheal, subcarinal, and left hilar adenopathies suggesting infiltrative tumors. The anatomical pathology study of a sample obtained with endobronchial ultrasound-guided transbronchial needle aspiration indicated small-cell lung cancer.
Due to symptom progression, the patient was treated with IV benzylpenicillin and methylprednisolone 500mg/24hours. Given that results from the RPR test in serum and the VDRL test in CSF were negative, neurosyphillis was considered to be unlikely. As a result, after 3 days of IV benzylpenicillin, treatment was changed to 3 doses of intramuscular benzylpenicillin per week. Choreic symptoms worsened with treatment with IV benzylpenicillin. The patient was subsequently treated with chemotheraphy and symptoms improved significantly, although mild chorea persisted.
In cases of a choreic syndrome with bilateral lesions in basal ganglia, hyperintensities in T2-weighted images, and normal signal intensities in T1-weighted images, the differential diagnosis should cover Wilson disease, Huntington disease, Huntington disease-like syndromes (prion disease or HDL1, spinocerebellar ataxia type 17 or HDL3, and dentatorubral-pallidoluysian atrophy), hypoxic-ischaemic encephalopathy, hypoglycaemia episodes, CO or cyanide intoxication, mitochondrial diseases, infectious diseases, and Creutzfeldt–Jakob disease, among others.1,3 However, these diseases were ruled out since the patient had not been exposed to toxins, had no prior episodes that might have caused hypoxic-ischaemic encephalopathy, displayed normal findings in the metabolic study, and showed subacute and progressive symptoms. Based on paraclinical findings, no tests measuring the blood acanthocyte level were necessary to rule out chorea-acanthocytosis. Although the literature describes cases of chorea associated with neurosyphilis responding well to IV penicillin,4 syphilis in our patient was regarded as a casual finding; neurological impairment was unlikely given the results from the serology tests and progression of symptoms despite treatment with IV benzylpenicillin.
Symptoms were secondary to a paraneoplastic syndrome caused by onconeural anti-CV2/CRMP5 antibodies; these antibodies are most frequently described in patients with paraneoplastic choreic syndrome (64%).2 These antibodies are sometimes associated with anti-Hu (ANNA1) antibodies (12%), or the latter may be expressed alone (19%).2 There are some cases in which no associated onconeural antibodies were present.2 Chorea is the key symptom in this entity. It can present in the absence of other common manifestations including opsoclonus-myoclonus, polyneuropathy, cerebellar ataxia, psychiatric alterations, limbic encephalitis, or other symptoms associated with anti-CV2/CRMP5 antibodies such as visual disturbances or a Lambert–Eaton-like myasthenic syndrome associated with thymoma.2,5–8
The type of tumor most frequently associated with this disease is small-cell lung cancer, although several cases of colon carcinomas, renal cell carcinomas, non-small-cell lung cancer, germinomas, and lymphomas have also been described.2,9
A brain MRI test does not rule out this disease. In fact, in one of the most comprehensive case series on paraneoplastic choreic syndromes in the literature, 7 out of the 12 patients undergoing an MRI scan showed normal results. The remaining 4, however, presented diffuse white matter alterations and developed basal ganglia anomalies during the follow-up period, with 2 displaying hyperintensities in T2-weighted and FLAIR sequences.2 Other authors have described cases of initially isolated anomalies in the basal ganglia that disappeared over time.7 The amygdalar lesions typical of limbic encephalitis are infrequent; only one case was observed among the 12 participants, and it was associated with anti-Hu antibodies.2 Another case in a series of 29 patients was secondary to anti-CV2/CRMP5 antibodies.2,10 Damage to the ventral nucleus of the striatum secondary to diffuse lesions in this area may be the reason for our patient's behavioral changes. However, unlike the chorea symptoms, behavioral changes did not improve with treatment.
Although immunomodulator treatments7 may provide some benefit, the prognosis depends on tumor progression.2 The literature reports several cases in which patients responded well to symptomatic treatment with haloperidol, clonazepam, or tiapride.2 Our patient showed a good initial response to diazepam, although symptoms progressed until onset of chemotherapy.
Our findings are in line with those described in other case reports. In patients older than 40 presenting an acute-onset choreic syndrome and showing striatum anomalies in brain MRI sequences, a paraneoplastic process should be suspected when other diseases have already been ruled out. The possibility of non-small-cell lung cancer associated with anti-CV2/CRMP5 and/or anti-Hu antibodies should be examined first of all.
Please cite this article as: Crespo-Burillo JA, Hernando-Quintana N, Ruiz-Palomino P, Martín-Martínez J. Corea secundaria a encefalitis estriatal por anticuerpos CV2/CRMP5. Descripción de un caso y revisión de la literatura. Neurología. 2015;30:451–453.