We would like to thank Gelabert et al.1 for their article on our systematic review on the endovascular embolisation of the middle meningeal artery (MMA) to treat chronic subdural haematomas (CSDH).2 We would like to address some of the points raised.
Firstly, we regret the confusion described by Gelabert et al.1 As expressed in the first paragraph of the conclusion, we agree that embolisation of the MMA is not the gold standard for treating CSDH.2 Evacuation via burr hole drainage is considered the primary treatment for this condition due to its low cost, user experience, and ability to rapidly improve the symptoms caused by the mass effect of the haematoma.3 However, CSDH presents a recurrence rate of 6%-25%.4–6 Although this is a technically simple procedure, the frailty of elderly patients with a higher number of comorbidities, associated with this considerable recurrence rate, gives rise to a high risk of complications in some populations.4,6,7 It is also the case that patients with greater risk of complications and recurrence are specifically those who have already presented recurrent CSDH.8 Therefore, after failure of conservative treatment with steroids has been demonstrated,9 it would be useful to find a technique involving lower risk but the highest possible success rate in patients presenting high surgical risk and in patients with CSDH resistant to the primary treatment.
Embolisation of the MMA is associated with a very low recurrence rate in the published series.10 Gelabert et al. highlight that our review does not include randomised prospective studies. This is particularly surprising for us, as our series clearly includes 2 prospective studies, though they are not randomised, as mentioned in the Methods section of the literature review.2 To refute our study, the authors cite another study that presents more, if not the same, limitations, as it is a retrospective study of CSDH cases treated with burr hole drainage. That study includes several selection biases, limited follow-up, no control group, and a poor statistical analysis with no multivariate analysis or controls for confounding factors.11 In fact, series of both surgical and conservative treatment present the difficulty that their results cannot be compared against alternative techniques, as the indications are different for both conservative treatment and embolisation or surgical evacuation of the MMA. However, a recent prospective study showed that endovascular treatment with embolisation of the MMA after surgical treatment increases the volume of reabsorption of the haematoma, as compared to the group of patients who received surgical treatment only.12 The prospective study by Joyce et al.,13 including the largest number of patients to date, reached similar conclusions, reporting a success rate of 94% and a complication rate of 2%.
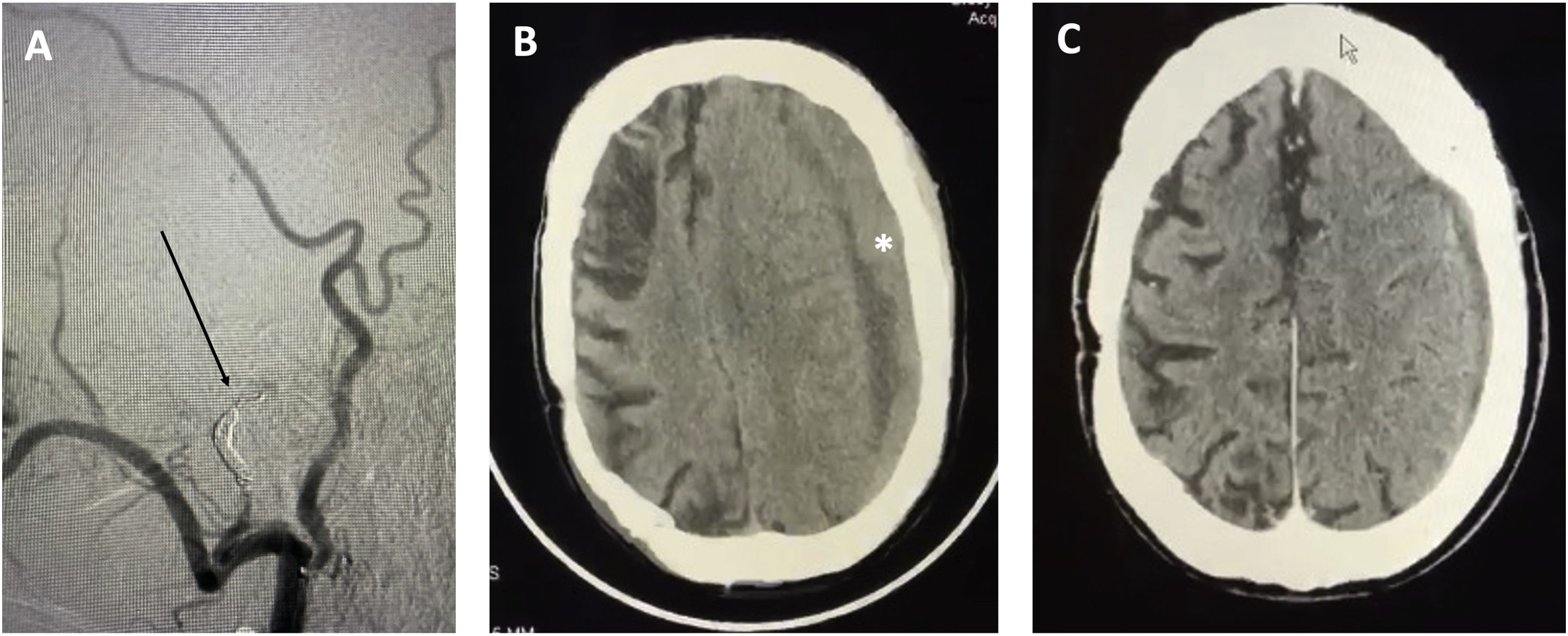
Furthermore, Gelabert et al., perhaps due to lack of knowledge of the current literature and despite the references provided, disagree with our idea that endovascular embolisation of the MMA may be performed under mild sedation. Embolisation with Onyx is a painful procedure that requires orotracheal intubation in most cases.14 This is not the case for embolisation with polyvinyl alcohol, which may be performed with the patient awake, and has been shown to be safe and efficacious.14,15 In our practice, we also opted for distal coil embolisation of the MMA at the entry of the foramen spinosum, under mild sedation (Fig. 1). This procedure enables us to achieve proximal control and to avoid complications derived from occlusion of the branches supplying the Meckel cave and the geniculate ganglion of the facial nerve. After this, controlled embolisation of distal branches with polyvinyl alcohol provides long-term stability. Our series of 12 patients with 20 CSDHs (in press) showed resolution of the haematoma in all cases, finding no such complications as bleeding, infection, recurrence, or visual impairment. We should underscore that the procedure was indicated in all our patients after failure of surgical treatment, and was aborted in one case due to the detection of anomalous origin of the ophthalmic artery from the meningeal artery. Thus, we may conclude that embolisation of the MMA is an effective therapy for CSDH resistant to surgical treatment or in patients with a high level of comorbidity and high risk of complications of anaesthesia.2,9,10
Representative case of an elderly patient with a high comorbidity index (Charlson index > 2, previous history of infarction of the middle cerebral artery), and risk of anaesthesia complications. A) The patient underwent coil embolisation of the middle meningeal artery and polyvinyl alcohol embolisation of the distal branches (arrow). B) Preoperative CT scan after surgical treatment failure showing a subdural haematoma measuring 20 mm, mass effect, and significant midline shift (> 5 mm) (asterisk). C) CT findings at 4 weeks after endovascular treatment, showing complete resolution of the haematoma. The patient was able to resume his previous functional activity (score of 2 on the modified Rankin Scale).
Please cite this article as: Martinez-Perez R, Rayo N, Tsimpas A. Terapia endovascular para el manejo de hematomas subdurales crónicos tras el fracaso de tratamiento quirúrgico evacuador. Neurología. 2022;37:157–158.