Arterial ischaemic stroke is rare in paediatric patients.1 Nonetheless, it is considered an important cause of disability and mortality in this age group.2 Stroke aetiology in children is generally different from that observed in adult patients.3 Acquired and congenital heart defects are one of the main risk factors for paediatric ischaemic stroke.4
For a number of reasons, paediatric stroke is associated with a considerable diagnostic delay,5 which together with its low prevalence represents an obstacle to performing randomised trials with patients in the acute phase.
We present the case of a 13-year-old patient diagnosed at birth with complete atrioventricular canal, for which she had undergone several surgical interventions during childhood. Due to a prosthetic mitral valve implanted in one of these procedures, she was receiving anticoagulation therapy with acenocoumarol; she had recently been included in an INR self-monitoring programme.
The patient attended our centre due to right hemisphere deficit syndrome of 45 minutes’ progression. In the initial examination at the emergency department, she scored 18 on the NIHSS, with electrocardiography displaying sinus rhythm, and an INR (measured with a CoaguChek® system) of 1.3.
A baseline head CT scan performed 15 minutes after arrival scored 9 on the ASPECTS scale; CT angiography revealed tandem occlusion of the proximal right internal carotid artery and the M1 segment of the right middle cerebral artery.
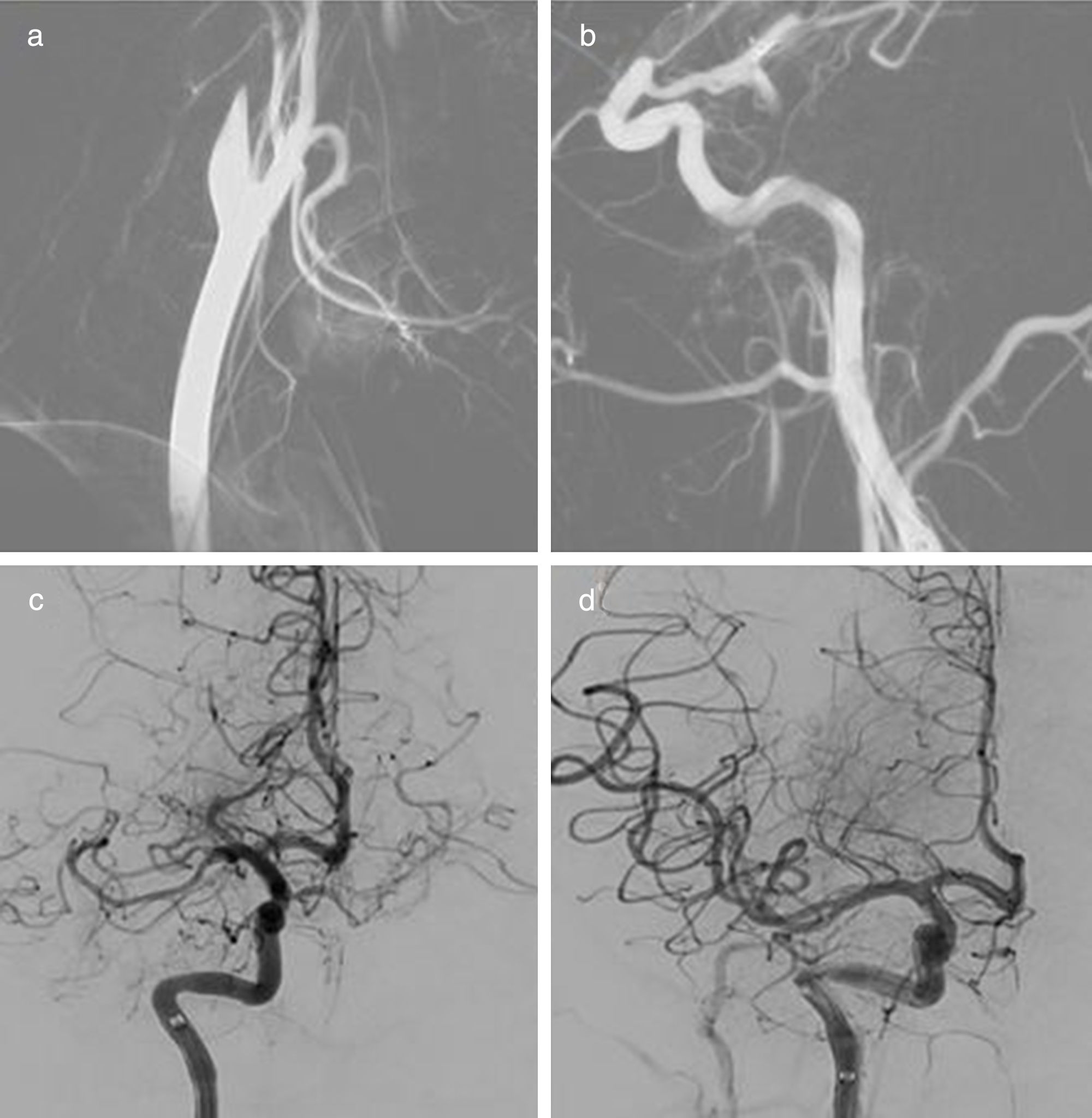
Given the patient's age and the evidence of large-artery occlusion of short progression, we opted for primary endovascular treatment. Primary thrombectomy was performed with a door-to-groin puncture time of 97 minutes. Revascularisation was achieved with 2 passes with a stent retriever, with a final score of 2b on the TICI scale (Fig. 1).
Four hours after the intervention, a head CT scan showed mild contrast enhancement in the basal ganglia and the right Sylvian fissure. Three months after the ischaemic event, the patient presented mild paresis of the left hand, scoring 1 on the modified Rankin Scale.
The treatment of acute stroke in paediatric patients has been subject to discussion in recent years.
The Thrombolysis in Paediatric Stroke study was closed in 2015 due to lack of recruitment, denying us indicative results on the efficacy and safety of this treatment.6
The revised American Heart Association/American Stroke Association guidelines on the early management of acute ischaemic stroke with endovascular treatment,7 published the same year, deem this treatment a reasonable course of action in patients younger than 18 provided that they present symptoms of less than 6 hours’ progression and evidence of large-vessel occlusion (grade of recommendation 2b, level of evidence C).
Until recently, the only evidence supporting endovascular treatment in paediatric patients was based on case reports and literature reviews, with the considerable publication bias this entails.8 However, the journal Paediatric Neurology recently published the first retrospective population study performed in the United States, with a cohort of 3184 paediatric patients with arterial ischaemic stroke. Only 1% of the sample received endovascular treatment; while these were the patients with the most severe symptoms, they did not present poorer prognosis than did patients not receiving this treatment.9
Several studies underscore the fact that the implementation of coordinated care protocols for the treatment of acute paediatric stroke has increased treatment rates for these patients, reducing diagnostic delays and facilitating access to immediate neuroimaging studies.10,11 It would appear, then, that there is a need to dedicate human and economic resources to the development of such protocols, with coordination between centres prior to the performance of new randomised studies.
Please cite this article as: Serra Martínez M, Avellaneda-Gómez C, Cayuela Caudevilla N, Rodríguez Campello A. Tratamiento endovascular del ictus isquémico arterial en edad pediátrica: a propósito de un caso. Neurología. 2020;35:52–54.
This study was presented in poster format at the 21st Annual Meeting of the Catalan Society of Neurology.