Despite recent advances in the management of acute stroke, fewer than 10% of patients receive reperfusion therapy. One of the main reasons for such a low rate of administration is the delay on the part of patients and their families in seeking medical attention. This study aimed to analyse this delay.
MethodsA prospective observational study was conducted on consecutive stroke or transient ischaemic attack. Data on sociodemographic and clinical parameters, decision delay, pre-hospital delay, and first medical contact were collected. Descriptive, bivariate, and multivariate logistic regression analyses were performed to determine factors associated with seeking medical attention within the first 15minutes of stroke or TIA occurrence.
ResultsA total of 382 patients were included, 24.9% of whom had a decision delay of 15minutes or less. Stroke severity (OR 1.08; 95% CI, 1.04-1.13; P<.001), patient's son/daughter witnessing the event (OR 3.44; 95% CI, 1.88-6.27; P<.001), and insulin treatment (OR 2.89; 95% CI, 1.35-6.20; P=.006) were related to an immediate reaction. Lacunar infarcts (OR 0.41; 95% CI, 0.17-0.97; P=.042), partial anterior circulation infarcts (OR 0.43; 95% CI, 0.22-0.85; P=.015), and monosymptomatic events not involving limb paresis or aphasia (OR 0.15; 95% CI, 0.033-0.724; P=.018) favoured delays longer than 15minutes.
ConclusionsSeverity of the event and presence of a son/daughter are the factors most frequently associated with an immediate response to stroke. Future interventions should emphasise the need for an immediate response irrespective of severity and include a wider spectrum of symptoms.
Pese a los recientes avances en el manejo agudo del ictus, se aplican terapias de reperfusión a menos de un 10% de los pacientes. Una de las causas es el retraso en la búsqueda de atención médica por el paciente y sus familiares, que analizaremos a continuación.
MétodosSe realizó un estudio observacional, prospectivo, en pacientes consecutivos con ictus o accidente isquémico transitorio. Se recogieron parámetros sociodemográficos y clínicos, y datos sobre el retraso en la decisión, retraso prehospitalario y el tipo de contacto médico seleccionado. Se realizaron análisis descriptivo, bivariante y multivariante para determinar los factores relacionados con la búsqueda de atención médica en los primeros 15minutos.
ResultadosSe recogieron 382 pacientes. Un 24,9% decidió solicitar atención médica en los primeros 15minutos. Lo favorecieron la severidad del evento (OR: 1,08; IC 95%: 1,04-1,13; p<0,001), estar acompañado de un hijo (OR: 3,44; IC 95%: 1,88-6,27; p<0,001) y el tratamiento con insulina (OR: 2,89; IC 95%: 1,35-6,20; p=0,006). Los infartos lacunares (OR: 0,41; IC 95%: 0,17-0,97; p=0,042), los infartos parciales de circulación anterior (OR: 0,43; IC 95%: 0,22-0,85; p=0,015) y los cuadros monosintomáticos sin afasia o paresia de miembros (OR: 0,15; IC 95%: 0,033-0,724; p=0,018) se relacionaron con retrasos mayores de 15minutos.
ConclusionesLa severidad y estar acompañado de un hijo fueron los principales determinantes de una reacción inmediata. Futuras intervenciones deben promocionar una consulta inmediata independientemente de la severidad, así como incidir en un mayor abanico de síntomas.
Stroke is the leading cause of disability and the second most frequent cause of death worldwide1,2; in Spain, it is the leading cause of death among women.3 The approval of the use of tissue plasminogen activator, and more recently mechanical thrombectomy, has contributed to a paradigm shift in stroke treatment, underscoring the relevance of the time factor in prognosis.4–6 However, despite this, only a minority of patients receive reperfusion treatment. The main reasons are the delay in patients’ response to symptoms and the type of response,7 which have meant that current rates (at about 1%-8%8–10) are far from the minimum needed to decrease the impact of stroke in the population.11
The aim of the present study is to analyse this delay in our setting and the factors associated with seeking medical attention immediately, understood as seeking care in the first 15minutes.
MethodsWe conducted a prospective, observational study of consecutive patients with stroke or transient ischaemic attack (TIA) attended by neurologists at the emergency department at Hospital Mancha-Centro between 15 November 2013 and 31 January 2015. Diagnosis of stroke was established in accordance with the definition of the World Health Organization; diagnosis was considered to be TIA when symptoms lasted less than 24hours. We excluded patients with subarachnoid haemorrhages, intrahospital strokes, cases with no reliable data on the times analysed, and those where the diagnosis of stroke was not confirmed.
Sociodemographic data and information regarding the prehospital period were obtained by interviewing the patients or their families in the first 3 days. Clinical data were collected from patients’ medical histories. All patients or family members signed informed consent forms. Our study protocol was approved by our hospital's Ethics Committee and complies with the ethical standards of the 1975 Declaration of Helsinki.
We conducted a descriptive analysis using measures of central tendency (mean or median) and dispersion (standard deviation or interquartile range) for quantitative variables and percentages for qualitative variables. We used the chi-square test to analyse differences between groups and the t test or its non-parametric variants to analyse quantitative variables. We performed a multivariate analysis using binary logistic regression; the model included variables showing a P value<.20 in the bivariate analysis as well as those considered especially relevant in decision delay (DD).
All analyses and calculations were performed using the PASW Statistics package (version 21.0; SPSS Inc., Chicago, Illinois) and EPIDAT 4.1.
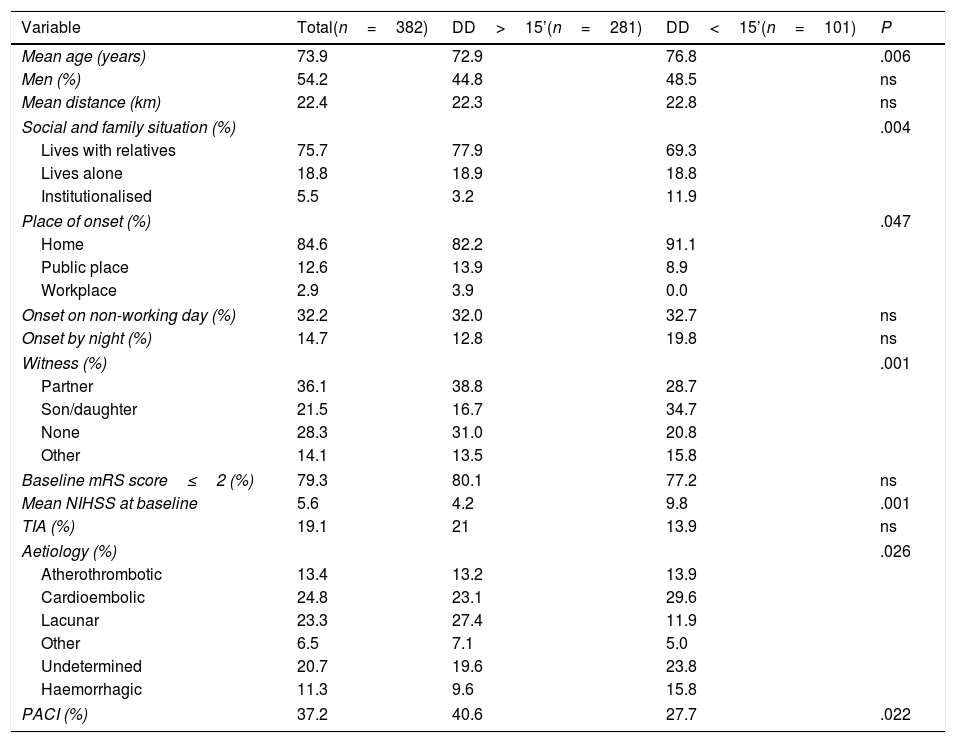
ResultsWe included 382 patients, of whom 73 (19.1%) presented a TIA, 46 (12.1%) a haemorrhagic stroke, and 263 (68.8%) an ischaemic stroke (Table 1).
Baseline characteristics of the sample and bivariate analysis.
| Variable | Total(n=382) | DD>15’(n=281) | DD<15’(n=101) | P |
|---|---|---|---|---|
| Mean age (years) | 73.9 | 72.9 | 76.8 | .006 |
| Men (%) | 54.2 | 44.8 | 48.5 | ns |
| Mean distance (km) | 22.4 | 22.3 | 22.8 | ns |
| Social and family situation (%) | .004 | |||
| Lives with relatives | 75.7 | 77.9 | 69.3 | |
| Lives alone | 18.8 | 18.9 | 18.8 | |
| Institutionalised | 5.5 | 3.2 | 11.9 | |
| Place of onset (%) | .047 | |||
| Home | 84.6 | 82.2 | 91.1 | |
| Public place | 12.6 | 13.9 | 8.9 | |
| Workplace | 2.9 | 3.9 | 0.0 | |
| Onset on non-working day (%) | 32.2 | 32.0 | 32.7 | ns |
| Onset by night (%) | 14.7 | 12.8 | 19.8 | ns |
| Witness (%) | .001 | |||
| Partner | 36.1 | 38.8 | 28.7 | |
| Son/daughter | 21.5 | 16.7 | 34.7 | |
| None | 28.3 | 31.0 | 20.8 | |
| Other | 14.1 | 13.5 | 15.8 | |
| Baseline mRS score≤2 (%) | 79.3 | 80.1 | 77.2 | ns |
| Mean NIHSS at baseline | 5.6 | 4.2 | 9.8 | .001 |
| TIA (%) | 19.1 | 21 | 13.9 | ns |
| Aetiology (%) | .026 | |||
| Atherothrombotic | 13.4 | 13.2 | 13.9 | |
| Cardioembolic | 24.8 | 23.1 | 29.6 | |
| Lacunar | 23.3 | 27.4 | 11.9 | |
| Other | 6.5 | 7.1 | 5.0 | |
| Undetermined | 20.7 | 19.6 | 23.8 | |
| Haemorrhagic | 11.3 | 9.6 | 15.8 | |
| PACI (%) | 37.2 | 40.6 | 27.7 | .022 |
DD: decision delay; mRS: Modified Rankin Scale score; NIHSS: National Institutes of Health Stroke Scale score; ns: not significant; PACI: partial anterior circulation infarct; TIA: transient ischaemic attack.
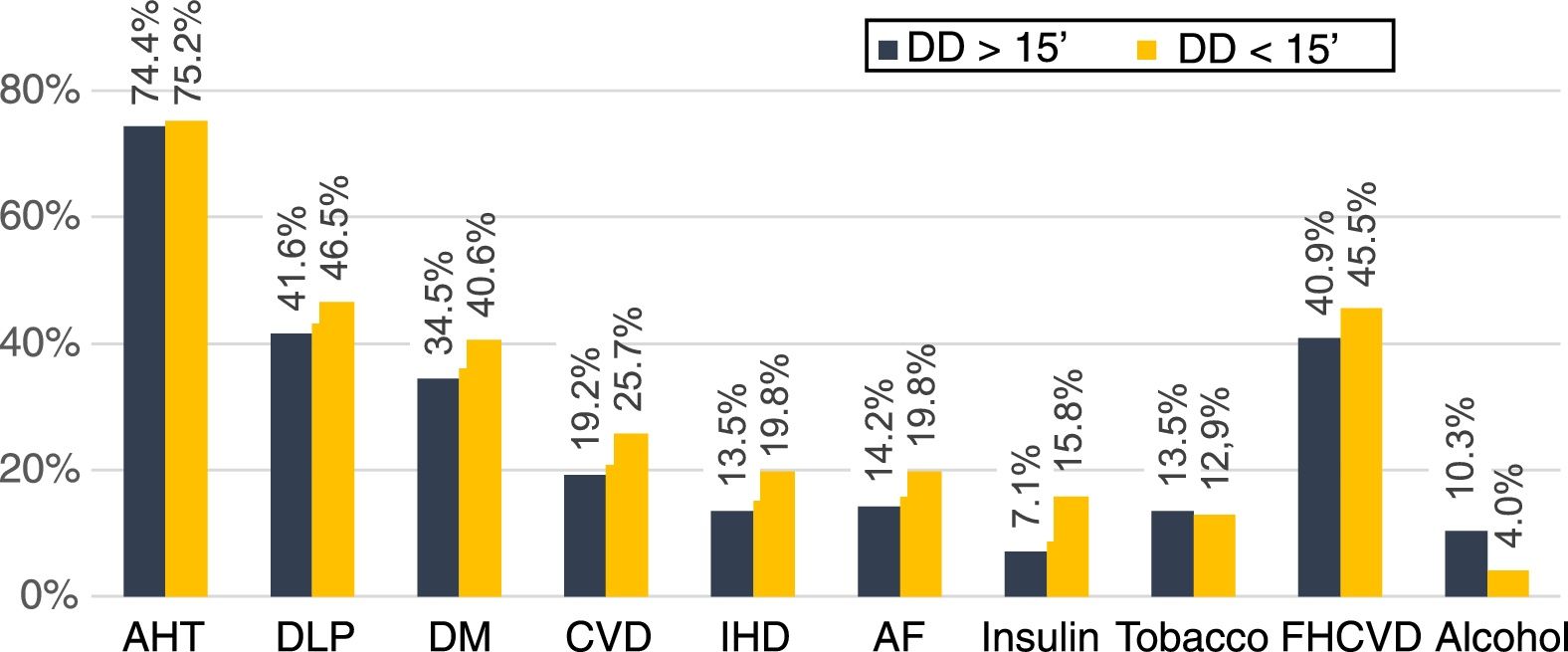
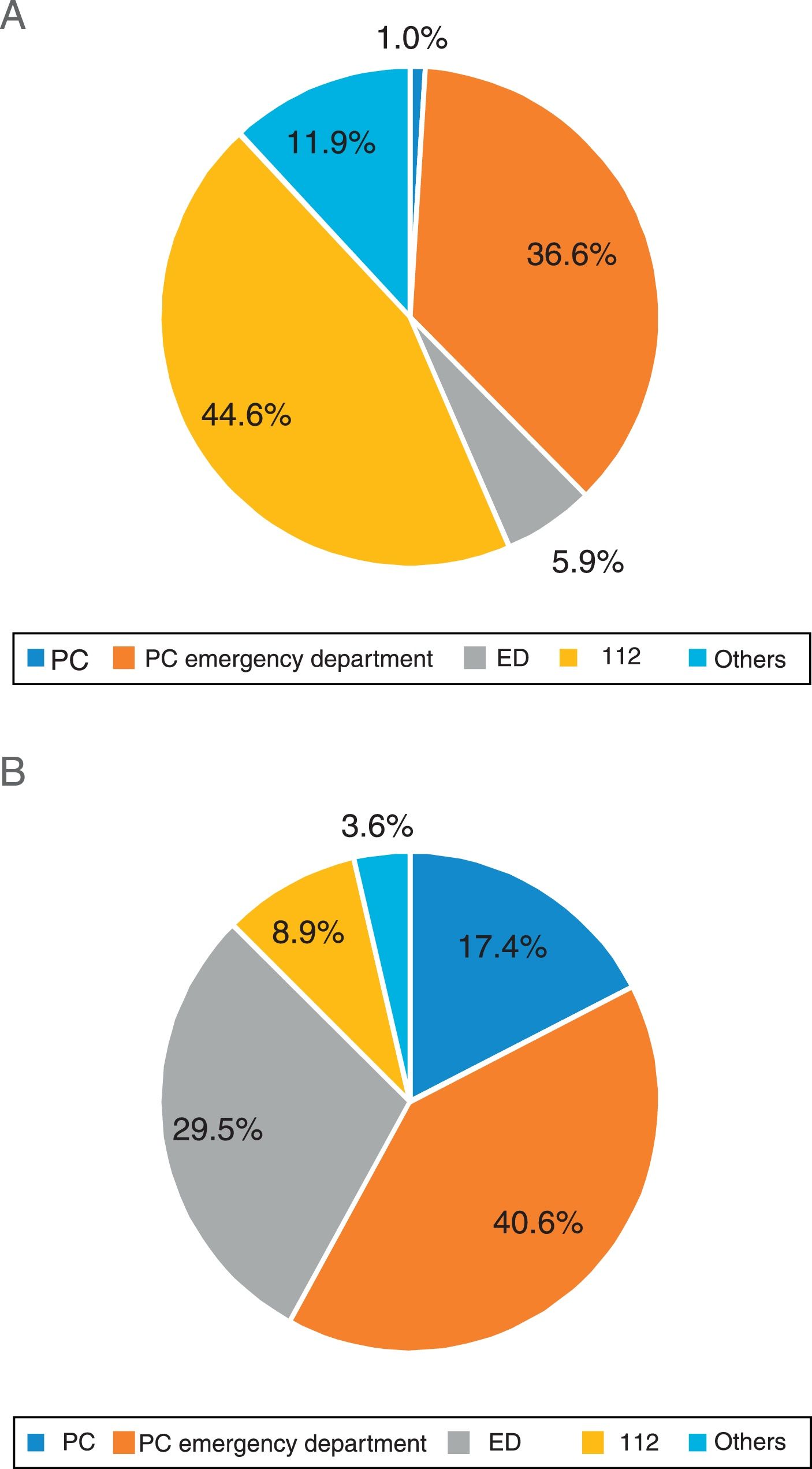
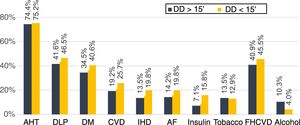
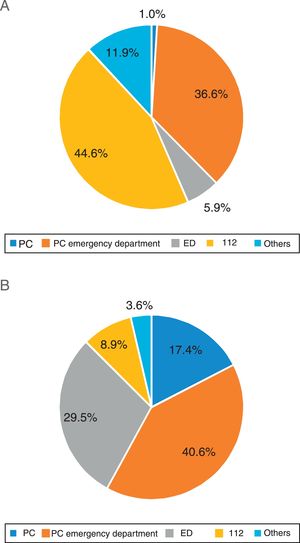
DD was <15minutes in 24.9% of patients; mean DD was 60minutes and the mean prehospital delay (PD) 201minutes (48.6% of patients arrived in the first 3hours and 13.4% in the first hour). In the bivariate analysis, no vascular risk factor was associated with higher probability of seeking medical care in the first 15minutes (Fig. 1). The initial medical contact was with prehospital emergency services (112 emergency telephone service) in 44.6% of patients with DD<15minutes vs 8.9% in those with DD>15minutes (P<.001) (Fig. 2).
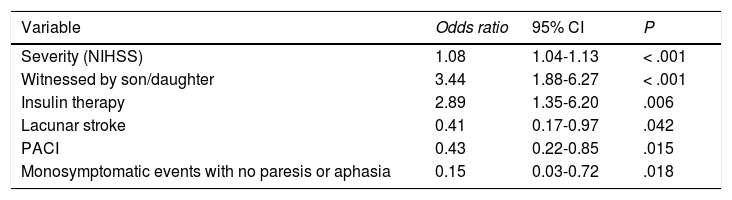
In the univariate analysis, higher severity as measured with the NIHSS scale, the presence of a son/daughter as a witness, and history of diabetes treated with insulin were associated with a DD≤15minutes. On the other hand, factors related to a DD>15minutes were lacunar stroke, partial anterior circulation infarct (PACI), and a monosymptomatic event without limb weakness or aphasia (Table 2).
Factors associated with a decision delay≤15minutes in the multivariate analysis.
| Variable | Odds ratio | 95% CI | P |
|---|---|---|---|
| Severity (NIHSS) | 1.08 | 1.04-1.13 | < .001 |
| Witnessed by son/daughter | 3.44 | 1.88-6.27 | < .001 |
| Insulin therapy | 2.89 | 1.35-6.20 | .006 |
| Lacunar stroke | 0.41 | 0.17-0.97 | .042 |
| PACI | 0.43 | 0.22-0.85 | .015 |
| Monosymptomatic events with no paresis or aphasia | 0.15 | 0.03-0.72 | .018 |
95% CI: 95% confidence interval; NIHSS: National Institutes of Health Stroke Scale score; PACI: partial anterior circulation infarct.
Our data on DD are consistent with those reported in most published studies, with medians of 120-240minutes and rates of 40%-60% of patients presenting DD<180minutes and 15% with DD<60minutes.12–16 Published studies reporting medians below 2hours or rates of over 70% of patients being attended in the first 180minutes17,18 are scarce, or limited to patients attended in the first 24-72hours.19 Other study groups, such as Ashraf et al.20 and León-Jiménez et al.,21 report more prolonged median values than ours. These data support the idea that despite stroke awareness campaigns, the decrease in DD has slowed in the past few years.22
Studies analysing DD show great methodological variability, which makes comparison difficult. We found median delays of 15-60minutes in studies including only patients assessed within 36-48hours of symptom onset,16,19 or with high percentages of patients with response times considered “early” or “immediate” but not detailing the precise times,14,15 and even studies with longer mean delays than ours.13 In the Spanish setting, Geffner et al.23 in Castellón obtained the same median as ours.
In our sample, we identified 2 factors associated with a DD<60minutes: history of treatment with insulin, and monosymptomatic events with no limb paresis or aphasia. The first may be due to knowledge of the risks associated with diabetes, or an increased perception of frailty. In the case of monosymptomatic events, these are probably associated with decreased perception of severity, which may also be considered a weakness of campaigns such as FAST (Face, Arm, Speech, Time), focusing attention in a limited set of symptoms.23 Severity is a factor frequently associated with DD.24 In our study, severity is expressed as a decreased DD in patients with higher scores on the NIHSS scale, as well as in a higher probability of DD>15minutes in patients with lacunar stroke or PACI. Finally, the presence of a son/daughter witnessing the event was associated with decreased delay. This seems to be related to the witness taking an active role in response to stroke symptoms.25
The main limitation of our study is that it was performed at only one centre, which limits its applicability to other areas. Another limitation may be the lack of data on perception of the event by the patient or witnesses. However, we believe that their responses might be distorted during admission, since they receive information on diagnosis, therapeutic options, etc. One of the strengths of our study is the wide range of factors studied in association with DD, which have enabled us to find several associations for the first time.
We might underscore several aspects to be considered in future studies. Firstly, we deem it necessary to inform potential patients of the need to react immediately, regardless of severity. Secondly, we highlight the need to assess the inclusion of additional symptoms of stroke in future awareness campaigns. Lastly, considering the high prevalence of vascular risk factors in patients with stroke, which was not associated with a better response to symptoms, we propose that awareness campaigns should be run, targeting patients at higher risk (hypertension, diabetes, atrial fibrillation, etc.). These strategies should also include the family members of these patients, considering the important role they play when stroke symptoms present.
Conflicts of interestThe authors have no conflicts of interest that may affect the content of this manuscript.
Please cite this article as: García Ruiz R, Silva Fernández J, García Ruiz RM, Recio Bermejo M, Arias Arias Á, Santos Pinto A, et al. Factores relacionados con una respuesta inmediata a los síntomas en pacientes con ictus o accidente isquémico transitorio. Neurología. 2020;35:551–555.