We studied patients who had experienced a stroke in the postoperative period of cardiac surgery, aiming to analyse their progression and determine the factors that may influence prognosis and treatment.
MethodsWe established a protocol for early detection of stroke after cardiac surgery and collected data on stroke onset and a number of clinical, surgical, and prognostic variables in order to perform a descriptive analysis.
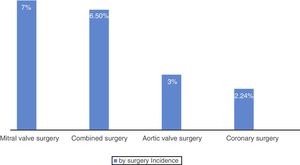
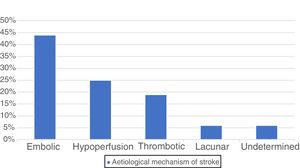
ResultsOver the 15-month study period we recorded 16 strokes, which represent 2.5% of the patients who underwent cardiac surgery. Mean age in our sample was 69±8 years; 63% of patients were men. The incidence of stroke in patients aged 80 and older was 5.1%. Five patients (31%) underwent emergency surgery. By type of cardiac surgery, 7% of patients underwent mitral valve surgery, 6.5% combined surgery, 3% aortic valve surgery, and 2.24% coronary surgery. Most cases of stroke (44%) were due to embolism, followed by hypoperfusion (25%). Stroke occurred within 2 days of surgery in 69% of cases. The mean NIHSS score in our sample of stroke patients was 9; code stroke was activated in 10 cases (62%); one patient (14%) underwent thrombectomy. Most patients progressed favourably: 13 (80%) scored≤2 on the modified Rankin Scale at 3 months. None of the patients died during the postoperative hospital stay.
ConclusionIn our setting, strokes occurring after cardiac surgery are usually small and have a good long-term prognosis. Most of them occur within 2 days, and they are mostly embolic in origin. The incidence of stroke in patients aged 80 and older and undergoing cardiac surgery is twice as high as that of the general population.
Estudiar a los pacientes que tuvieron un ictus en el postoperatorio de cirugía cardiaca, para ver la evolución y determinar los factores que influyen en su pronóstico y tratamiento.
MétodosEstablecimos un protocolo para la detección precoz de ictus en los pacientes tras cirugía cardiaca. Recogimos la aparición de ictus y datos clínicos, quirúrgicos y pronósticos; posteriormente realizamos un análisis descriptivo.
ResultadosDurante los 15 meses del estudio hubo 16 ictus, un 2,5% de los pacientes operados. Edad media 69±8 años, 63% varones. La incidencia de ictus en pacientes octogenarios fue del 5,1%. Cinco (31%) fueron cirugías urgentes. Por enfermedad cardiaca intervenida: un 7% recibió cirugía mitral, 6,5% cirugía combinada, un 3% cirugía valvular aórtica y un 2,24% cirugía coronaria. La mayoría de los ictus (44%) fueron por embolia, seguida por hipoperfusión (25%). El 69% de los ictus ocurrieron en los 2 primeros días de postoperatorio. La media de la puntuación en la escala NIHSS en el ictus fue 9, se activó código ictus en 10 (62%), y se realizó trombectomía en uno de ellos (14%). La evolución fue favourable en la mayoría, con una escala de Rankin a los 3 meses≤2 en 13 (80%). No hubo muertes hospitalarias entre estos pacientes.
ConclusiónEn nuestro medio, los ictus tras cirugía cardiaca son de pequeño tamaño y tienen una buena evolución a largo plazo. La mayoría ocurren en los primeros 2 días de postoperatorio y su mecanismo es principalmente embólico. La incidencia de ictus en los pacientes octogenarios intervenidos fue del doble que en la población general.
Stroke is a severe complication of cardiac surgery. Incidence rates of up to 6% are reported,1–3 with the value varying according to whether studies are prospective or retrospective.4 The annual worldwide volume of cardiac surgery makes it one of the main causes of iatrogenic stroke. Perioperative stroke negatively affects patients’ short- and long-term prognosis.3,5
The population undergoing cardiac surgery has changed in recent decades: the percentage of patients undergoing myocardial revascularisation surgery has decreased, whereas valve or combined surgery are increasingly frequent.6 Furthermore, patients undergoing cardiac surgery are older and present greater levels of associated comorbidity; therefore, they present a higher risk of cerebrovascular disease and undergo more complex surgical procedures.7
Considering the above, our centre decided to perform a prospective study of strokes occurring after cardiac surgery. Multidisciplinary support was provided by the neurology, intensive care, and cardiac surgery services.
The aims of this prospective register are:
- 1.
To identify the actual incidence of stroke in patients undergoing cardiac surgery at our centre.
- 2.
To determine whether incidence of postoperative stroke increases as older patients with greater levels of comorbidity are treated.
- 3.
To attempt to determine the causes and mechanisms of stroke after cardiac surgery.
- 4.
To attempt to modify possible risk factors for postoperative stroke.
- 5.
To assess the eligibility of these patients for mechanical thrombectomy for stroke. To determine how many patients in this group may benefit from this treatment in the acute phase, as well as its safety and usefulness.
Since 2010, our hospital has followed a treatment protocol for mechanical thrombectomy for stroke, adopted throughout our region within the framework of the region's stroke care plan; the protocol is recommended by the Spanish Society of Neurology and the stroke strategy of the Spanish National Health System. We considered the possibility of performing mechanical thrombectomy to treat patients presenting stroke upon awakening after cardiac surgery9 (given the inability to treat these patients with fibrinolysis) if the occluded vessel responsible for the stroke was large and fulfilled time or (primarily) imaging criteria.
Patients and methodsWe actively monitored all patients undergoing cardiac surgery at our hospital between October 2014 and December 2015 to enable early detection of any postoperative stroke. Where possible, given their haemodynamic situation, patients were extubated at the postoperative care unit in the first 6hours after surgery. After awakening, they underwent a neurological examination and were assessed daily by trained professionals (physicians and nurses from the unit). If the slightest neurological symptoms were detected, the on-call neurologist was informed and conducted an examination; if he/she considered it appropriate, code stroke was activated and the relevant diagnostic tests were requested (simple head CT scan, CT angiography, and perfusion CT scan),8 and according to the results, we determined whether patients were eligible for acute reperfusion therapy with thrombectomy. Once the neurologist confirmed the diagnosis of stroke, data were entered into a database gathering anonymised data on patient variables (age, sex, body mass index, body surface area, diagnosis, preoperative treatment), surgical procedure variables (use of extracorporeal circulation [ECC], myocardial ischaemia time, ECC time, etc.), stroke clinical variables, aetiological mechanism of stroke, possibility of acute stroke care, and stroke prognostic variables.
Qualitative variables were expressed as frequencies and percentages. Quantitative variables were expressed as means (standard deviation [SD]) and compared with qualitative variables using the t test. We used SPSS® version 20.0 (SPSS, IBM; Chicago, IL, USA) for statistical analysis.
Definition of stroke: perioperative stroke was defined as any new, transient or permanent, global or focal, neurological deficit occurring in the first 30 days after surgery, according to the published guidelines.10 This definition of perioperative stroke therefore includes transient ischaemic attacks (fully reversible neurological deficits lasting less than 24hours with no neuroimaging abnormalities) and stroke, defined as permanent neurological deficits with positive neuroimaging findings.
After determining the aetiological mechanisms of stroke after cardiac surgery, we followed the recommendations of the Northern New England Cardiovascular Disease Study Group,11 who classify strokes after cardiac surgery as haemorrhagic or ischaemic. Ischaemic strokes are subdivided into thromboembolic and hypoperfusion-related. The thromboembolic subtype includes embolic, lacunar, and thrombotic strokes.
EuroScore: the EuroScore is a preoperative surgical risk scale used since the late 1990s, promoted by the European Association for Cardio-Thoracic Surgery, derived from data from more than 19000 patients all over Europe.12 The first version of the scale presented 2 modalities: the additive version, which permitted bedside assessment, and the logistic version, which requires a computer to make the calculation. In this study, we applied the logistic version.
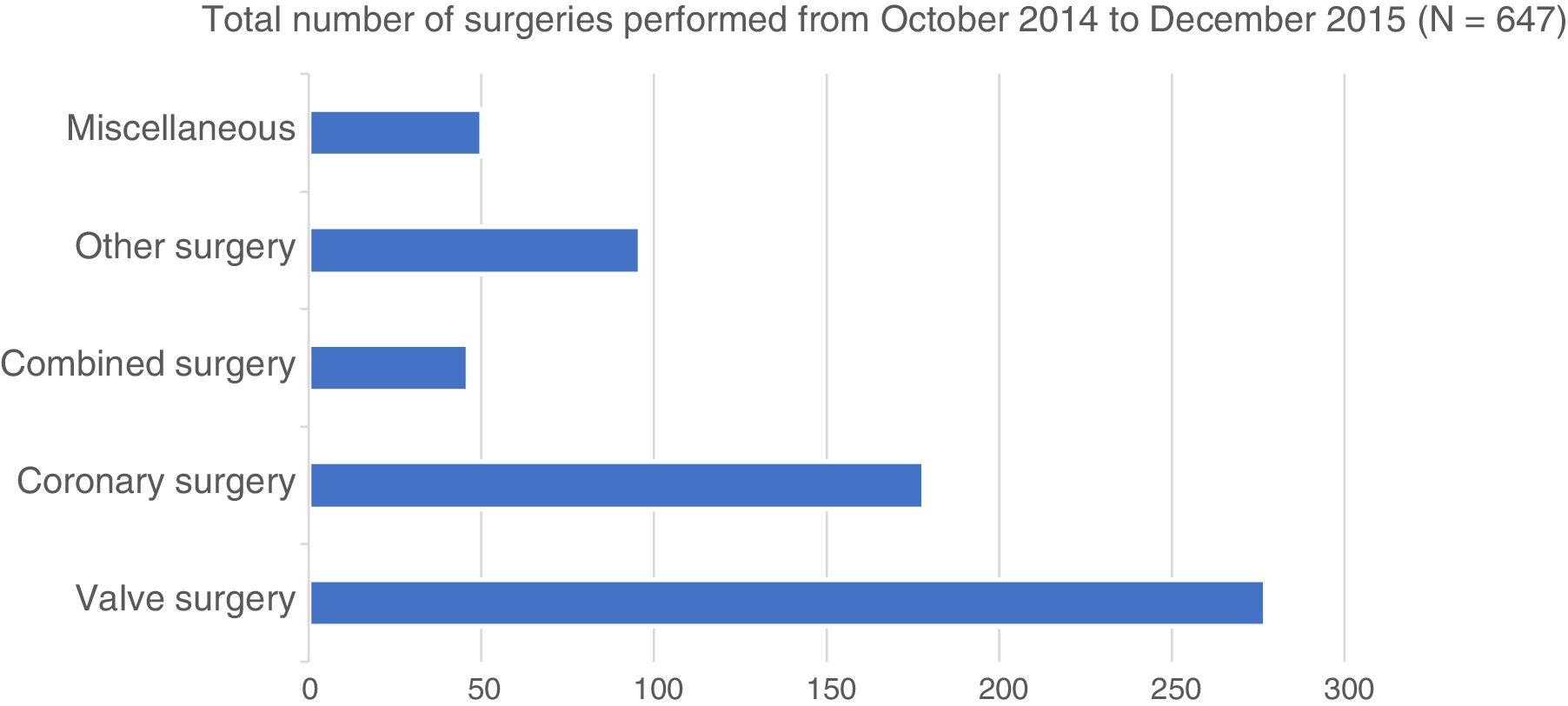
ResultsBetween October 2014 and December 2015 (15 months), 647 patients underwent cardiac surgery at our centre. Mean age (SD) was 65 (12) years; 67% were men, 252 patients (39%) were older than 70, and 39 (6%) were older than 80. Valve surgery was performed in 277 cases (43%), coronary surgery in 178 patients (27%), combined surgery (valve and coronary) in 46 (7%), other surgery (aortic, adult congenital heart disease, transplant, heart tumours, etc.) in 96 (15%); finally, 50 patients were included in a miscellaneous group (8%) (Fig. 1).
Of these 647 patients, 16 (2.5%) presented a stroke after cardiac surgery. Sixty-three percent of this group (10) were men; mean age was 69 (8) years (P=.571).
In 10 of the 16 patients with stroke, the on-call neurologist was notified. Of these 10, code stroke was activated in 7 cases (70%). One patient (15%) underwent mechanical thrombectomy; this represents 6% of all patients with postoperative stroke. Before the procedure, all patients were studied with echocardiography and Doppler ultrasound of the supra-aortic trunks. Stroke was confirmed by MRI in 13 of the 16 cases (80%).
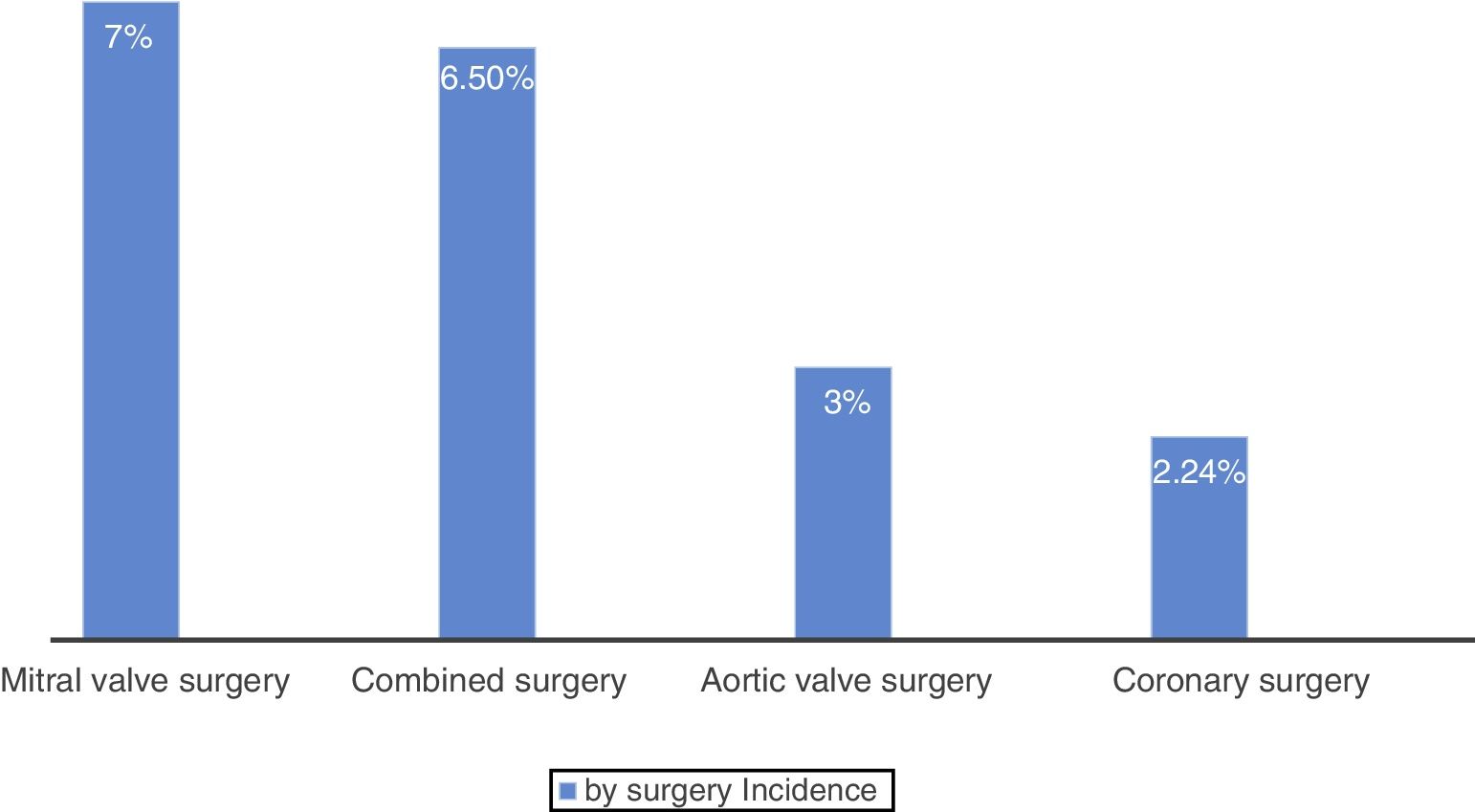
By type of surgical procedure, postoperative stroke occurred in 4 of the 178 patients who underwent myocardial revascularisation (2.24%), 6 of the 232 patients who underwent aortic valve surgery (3%), 3 of the 45 patients who underwent mitral valve surgery (7%), and 3 of the 46 patients who underwent valve and coronary surgery (6.5%) (Fig. 2). Five patients presenting stroke in the postoperative period (31%) underwent emergency surgery.
The mean logistic EuroScore12 for the 16 patients with postoperative stroke was 6.4 (5); the mean EuroScore for the population receiving surgery and not presenting stroke was 6.9 (8) (P=.75). The mean myocardial ischaemia and ECC times in the patients with stroke were 71 (41) and 104 (61) minutes, respectively, vs 67 (42) and 89 (58) minutes in those not presenting postoperative stroke during the study period (P=.370 and P=.123, respectively). The mean stay at the preoperative intensive care unit and at hospital was 4 (5) and 18 (15) days, respectively, for patients with stroke, vs 3.45 (6.5) and 15 (15) for patients not presenting stroke (P=.001 and P=.03, respectively).
Of the 16 patients who presented postoperative stroke, half were older than 70 years and 2 (12.5%) were older than 80; this translates to a stroke incidence of 3.1% in patients older than 70 and 5.1% in patients older than 80.
Regarding comorbidities, 38% of patients with stroke (6) were diabetic and in 7 patients (44%) stroke was related to atrial fibrillation (AF) (6 cases with preoperative AF and one case of postoperative AF). In the preoperative Doppler ultrasound study, 2 patients (12%) displayed normal results, 10 (62%) presented non-significant atheromatosis, one (6%) showed 50%-70% stenosis, and 3 (19%) showed > 50% stenoses bilaterally. Thus, 4 of the patients with postoperative stroke (25%) had existing carotid artery disease; 3 (19%) had a history of cerebrovascular accident.
Patients presenting postoperative stroke (n=16) in the 15-month study period received the following surgeries: 6 (38%) received aortic valve surgery, 4 (25%) coronary surgery, 3 (19%) mitral valve surgery, and 3 (19%) combined surgery. ECC was used for 15 of these patients (94%). In 7 patients (44%), transfusions of red blood concentrates were used.
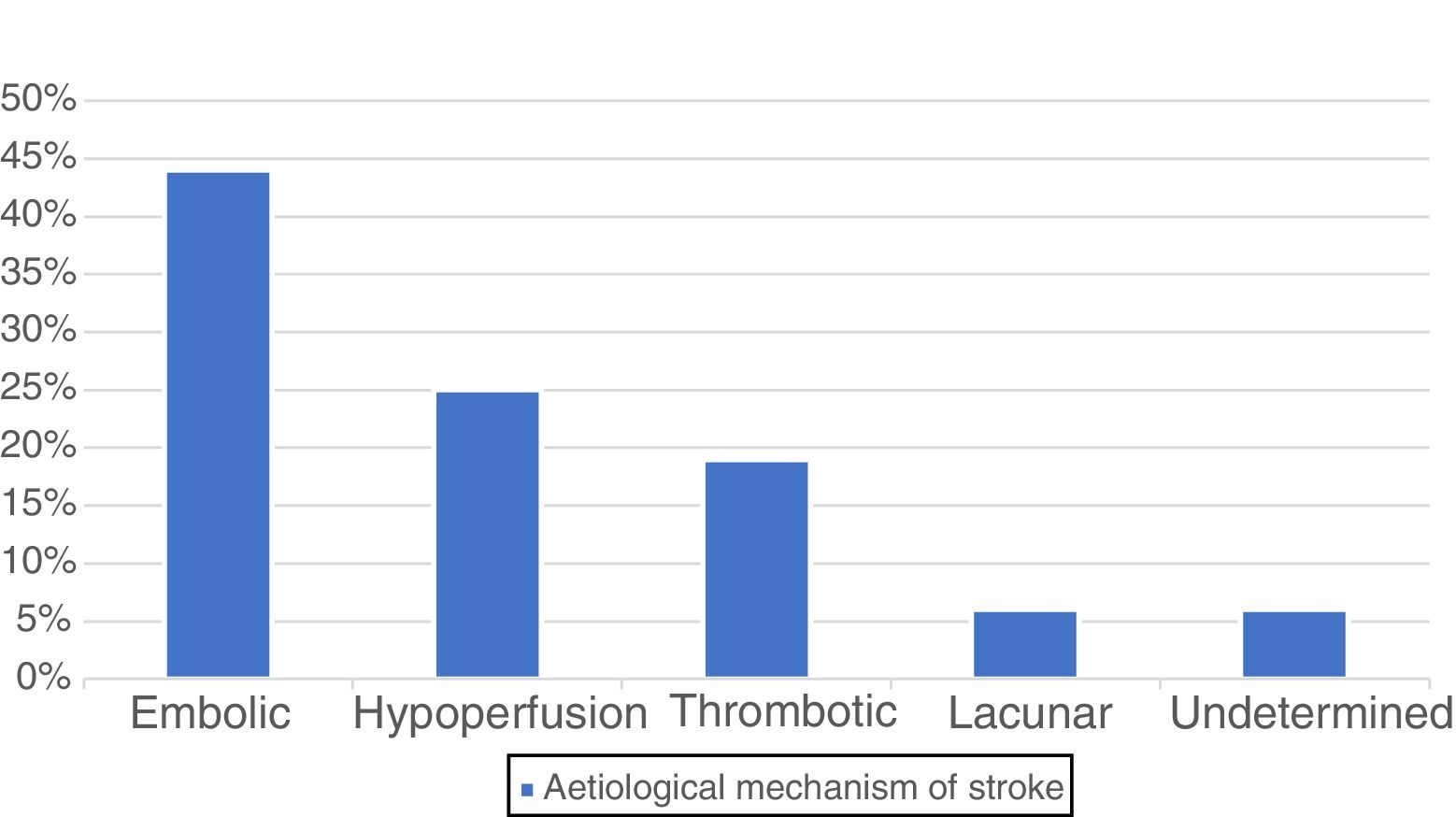
By aetiology,11 postoperative stroke was embolic in 7 patients (44%), caused by hypoperfusion due to hypotension at the operating theatre or postoperative care unit in 4 cases (25%), thrombotic in 3 (19%), and lacunar in one case (6%); no aetiological diagnosis was established in the remaining strokes, which were classified as undetermined (6%) (Fig. 3).
Regarding anatomical location, stroke was located in the right hemisphere in 5 patients (31%), in the left in another 5 (31%), and was bilateral in one patient (6%); stroke involved the posterior fossa only in 2 patients (12%) and no lesion was found on the CT scan or MRI study in 3 cases, which were classified as postoperative transient ischaemic attacks. The anterior circulation was affected in 8 patients (50%), the posterior circulation in 3 (19%), and 2 patients (12%) presented watershed territory impairment.
Mean time of stroke onset after surgery was 37 (SD: 37) hours after patient-out-of-room time (range, 2-120), with a median of 17hours (interquartile range, 7-72). Fifty-six percent of postoperative strokes (9) occurred in the immediate postoperative period (first day after surgery, range, 2-22hours after surgery), whereas in the remaining 44% (7 patients) stroke occurred after the first day of the postoperative period (range, 34-120hours). In the first 48hours after surgery, 11 patients (69%) presented stroke.
None of the patients who presented stroke after cardiac surgery during the study period died. These patients presented a mean NIHSS score13 at stroke onset of 9.
Eighty per cent of these 16 patients (13) presented a modified Rankin Scale score14 of 2 or less at 3 months after stroke. One patient (6%) died due to heart failure 14 months after a procedure to treat prosthetic valve thrombosis.
DiscussionIn the 15 months of our study, the incidence of postoperative stroke after cardiac surgery in our centre amounted to 2.5%; this figure is lower than that reported in larger series,1 which report an incidence of 4.6%. The rate of postoperative stroke-associated hospital mortality was zero. We believe that these findings might be explained by a series of factors, such as the selection and screening of patients prior to surgery; the development of improved anaesthetic techniques, such as continuous cerebral monitoring during the surgical procedure; improved surgical and ECC techniques; better postoperative care with a view to early extubation and close monitoring to detect any neurological damage as soon as possible; and effective communication between the different professionals caring for these patients in the different stages of the postoperative period. We should also mention that the series published in the literature1–5 date from the first decade of the 21st century; slow but constant improvements in the medical care of these patients have been observed in recent years.
Among the cardiac diseases treated, we found the highest incidence of postoperative stroke in patients undergoing isolated mitral valve surgery (7%), a figure that coincides with that reported by Bucerius et al.1 in 2003 in a series of more than 16000 patients treated in Leipzig (almost 9%). The higher incidence of postoperative stroke after isolated mitral valve surgery might be due to the higher presence of AF in patients with this condition, the use of a cardiopulmonary bypass, and the need to open large cavities of the left side of the heart, which increases the likelihood of air embolism in these patients. Isolated mitral valve surgery is followed by combined valve and coronary surgery, with an incidence of postoperative stroke of 6.5%; this figure coincides with the findings of previous studies,1,2 which also consider this population to be at a high risk of postoperative stroke. Isolated aortic valve surgery shows a postoperative stroke incidence of 3%, slightly lower than the figures reported by previous studies1; isolated coronary surgery presents an incidence of postoperative stroke of 2.24%, a slightly higher figure than the mean reported by the Spanish multicentre study (PACK2 model) published in 2014 (1.4%), but within the interval found at different centres (0.3%-2.5%).15 This may be explained by the neurological examination protocol applied after surgical interventions, which enables detection of even the mildest postoperative strokes, which may go unnoticed in other studies that only detect more severe strokes; these series present a lower incidence of stroke but poorer outcomes.
These preliminary results encourage us to continue with the protocol implemented in our centre, despite the on-call neurologist not having been contacted in 38% of cases of postoperative stroke (6 patients). This was because these cases were not considered acute strokes. In these patients, the cardiovascular surgery department consulted with the neurology department through a consultation sheet and not through the on-call neurologist, since stroke had gone unnoticed until that time, appearing when the patient was already on the ward with minor symptoms, or being detected after a long progression time. Mechanical thrombectomy was performed in only one case (14%). There is room for improvement in this area, but once the procedure is shown to be possible and feasible, more patients with stroke and cerebral large vessel disease will benefit from this treatment in the postoperative period after cardiac surgery.9
Patients presenting stroke after cardiac surgery had a mean age of 69 (8) years, 4 years older than the mean age of all patients surgically treated (65 [12] years); this difference was not statistically significant (P=.571). Half of the patients with stroke were older than 70 years and 12% were older than 80; these percentages are higher than those observed in the total treated population (39% older than 70 and 6% older than 80); furthermore, incidence of stroke in patients older than 80 was 5.1%, double the incidence for all ages (2.5%). Our findings support the hypothesis that stroke is more frequent in older surgically treated patients, and that as more old patients are undergoing these procedures, this complication will become more frequent.
Furthermore, the patients with stroke presented significant comorbidities, as shown by the mean logistic EuroScore of 6.4 (5). However, this is slightly lower than the mean logistic EuroScore of the population surgically treated during the study period (6.9 [8]), although the difference was not statistically significant (P=.75). Myocardial ischaemia and ECC times were slightly longer in patients with postoperative stroke than in those without, suggesting that these surgical interventions were more complex or presented unexpected intraoperative complications; again, this difference was not statistically significant (P=.370 and P=.123, respectively). Stays at the postoperative care unit and total hospital stays were also significantly longer in these patients than in those without postoperative stroke (P=.001 and P=.03). This translates into more complex and costly healthcare.
In terms of the aetiological mechanism of postoperative stroke,11 most cases (44%) were of embolic cause originating in heart cavities or large arteries, which coincides with previous studies11; 29% were classified as being secondary to hypoperfusion caused by significant hypotension, whether in the operating theatre or the postoperative care unit, or associated with stenosis of extracranial large arteries. Almost 20% of strokes had a thrombotic origin due to stenosis of the intracerebral vessels, ruptured plaques in intracerebral vessels, associated with an inflammatory response, or more rarely, due to haematological alterations. Only one stroke (6%) was classified as lacunar, and was secondary to atherosclerosis induced by hypertension or stenosis of the arteries penetrating the white matter. No cases of haemorrhagic stroke were reported during our study period, despite the fact that brain haemorrhages represent 10% to 15% of all strokes in the general population.16
Other noteworthy elements include the direct or indirect role of AF (pre- or postoperative) in 44% of postoperative strokes, especially in mitral conditions; the use of an ECC device in almost all patients (94%) who presented postoperative stroke; and the fact that one-third of the patients with stroke were surgically treated on an emergency basis.
In our series, unlike in previous ones,17,18 the anatomical localisation of postoperative strokes did not predominantly affect either hemisphere (31% affected the right hemisphere and 31% the left, with one patient presenting stroke affecting both hemispheres, and 2 patients presenting only posterior fossa involvement). No lesions were found in brain CT or MRI studies in 18% of postoperative strokes (3 cases). The anterior circulation was affected in 50% of postoperative strokes, whereas the posterior circulation was affected in 19% and watershed territories in 12%; this percentage is similar to the anterior/posterior ratio reported in the general population with stroke.19
Regarding time of onset, 56% of postoperative strokes occurred in the first day after surgery, with the remaining 44% occurring after the first day, which coincides with previous studies2; median time of postoperative stroke onset was 17hours after surgery (interquartile range, 7-72hours). More than two-thirds (69%) of postoperative strokes after cardiac surgery in these 15 months occurred in the first 48hours after surgery, which underscores the importance of the first 2 days after surgery in the diagnosis and prevention of this complication.
Knowing the different aetiological mechanisms and the temporal distribution of stroke after cardiac surgery is necessary to any attempt to decrease its incidence.11
An important factor in our series is that there were no hospital deaths associated with postoperative stroke; other published series1–4 report mortality rates of up to 30% in patients presenting stroke in the postoperative period. One patient died due to heart failure associated with prosthetic valve thrombosis at 14 months of follow-up. Furthermore, patients with postoperative stroke in our series presented good medium- and long-term prognosis: the modified Rankin Scale score was lower than or equal to 2 in 80% of patients 3 months after the procedure. Therefore, we can state that most strokes occurring after cardiac surgery in our series were small and presented good prognosis. These data somewhat contradict the idea held by many surgeons that in many cases, stroke is worse than death. It will be interesting to observe the progression of this series in the longer term.
Our study is a retrospective analysis of data collected prospectively over 15 months at a single centre, and therefore, it is limited in time and sample size. We did not include cases of encephalopathy with disorientation, which may have had an ischaemic cause in some patients.
However, while we consider the incidence of postoperative stroke observed in our series to be very real, we also deem it necessary to keep thorough records in order to gather all strokes occurring after cardiac surgery, since many are small, easily curable, and may go unnoticed given the lack of an exhaustive detection process including appropriate clinical history-taking and a detailed neurological examination.
In our setting, stroke after cardiac surgery does not increase mortality or dependence in the majority of patients. Strokes after cardiac surgery were small and mild; at 3 months, prognosis was good and most patients presented no sequelae. The main aetiological mechanism is embolism, followed by cerebral hypoperfusion, and more than two-thirds of all strokes occurring after cardiac surgery appear in the first 2 days. Incidence of stroke in patients aged over 80 was double than that in the general population undergoing surgery (5.1% vs 2.5%).
Therefore, hospitals should implement a multidisciplinary protocol involving the different departments treating these patients to enable early detection of any stroke after cardiac surgery, as strokes affecting large cerebral blood vessels may benefit from mechanical thrombectomy.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Arribas JM, Garcia E, Jara R, Gutierrez F, Albert L, Bixquert D, et al. Incidencia y mecanismo etiológico de ictus en cirugía cardiaca. Neurología. 2020;35:458–463.