Multiple system atrophy (MSA) is a sporadic neurodegenerative disease characterised by the association of parkinsonism with autonomic failure, cerebellar ataxia and pyramidal signs. It typically begins at about 60 years of age and affects men and women equally. Mean survival is 6–9 years. According to the predominant clinical characteristics, it can be further categorised as MSA-P when parkinsonian clinical features predominate, MSA-C when cerebellar ataxia predominates, and MSA-A when autonomic failure predominates.1 MSA is mainly diagnosed based on clinical findings. Cranial magnetic resonance images may show putamen atrophy and infratentorial abnormalities such as the hot cross bun sign due to pontocerebellar degeneration.2 When associated with atrophy of the cerebellar vermis and hemispheres, this image is also known by the name “signo de santiaguiño” in Spanish literature, due to its resemblance to a type of crustacean.3
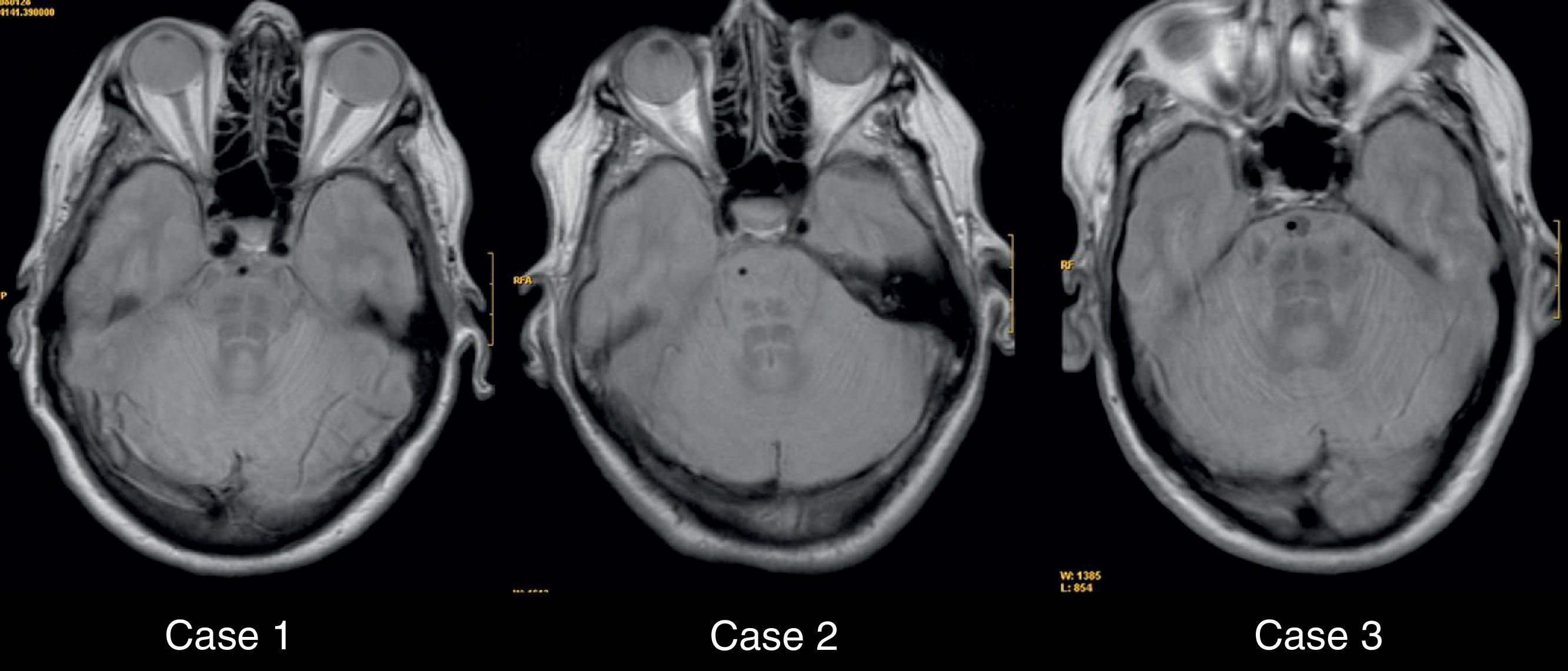
In this letter, we describe 3 clinical cases of cerebellar-type MSA (MSA-C) with typical MR images showing a hot cross bun sign. Of these 3 patients, 2 met diagnostic criteria for probable MSA while the third met criteria for possible MSA. The first patient is a 62-year-old woman evaluated due to symptoms of postural instability/falling and difficulty articulating speech which had been evolving over 3 years. At a later point, she also developed urinary urgency with occasional incontinence. Examination revealed hypomimia, dysarthria, persistent horizontal nystagmus, and bilateral bradykinesia along with ataxic gait and pyramidal signs. Results from a genetic study for ataxias were negative. In light of this clinical profile, we established a suspected diagnosis of probable MSA-C. In the second case the patient was a woman aged 74 years being monitored for possible MSA-C. Symptoms initiated as an akinetic-rigid, tremor-free syndrome with poor response to L-DOPA and poor tolerance for dopamine antagonists, instability due to ataxic gait and scanning dysarthria evolving over 6 years. Our third case was that of a male patient aged 85 years who was monitored for symptoms of akinetic-rigid parkinsonism, rapidly evolving postural instability and urinary incontinence, evolving over 3 years. Response to L-DOPA was poor. Examination revealed ataxic gait, horizontal-rotary nystagmus at extreme lateral gaze and bradykinesia. In these 3 cases, neuroimaging studies showed a hot cross bun sign on the pons.
We described 3 patients diagnosed with MSA-C and typical neuroimaging findings. Finding the hot cross bun sign in the imaging study supports our diagnosis of this entity, which is essentially diagnosed on a clinical basis.
In MSA-C (historically known as olivopontocerebellar atrophy), we can observe radiological changes, mainly in T2-weighted sequences in brain MRI (Fig. 1). Changes are mostly infratentorial,4 and include the typical hyperintense hot cross bun sign in the pons and other anomalies, such as putamen atrophy, putamen hypointensity and hyperintense putaminal rim.2–5 The hot cross bun sign is the result of the degeneration of pontine neurons and transverse pontocerebellar fibres. This could be considered an expression of degeneration and neuronal loss in the brain stem, and serves as a parameter for measuring disease progression.6 While the hot cross bun sign is typical, it is not pathognomonic to MSA.7 It has also been observed in cases of spinocerebellar ataxia (SCA) types 2 and 3, and in parkinsonism with cerebellar and brain stem alterations, presumably secondary to vasculitis.8 In our opinion, this radiological sign is not specific to MSA, but it does support that diagnosis when clinical symptoms are compatible with that entity.
Please cite this article as: Recio Bermejo M, et al. Signo de la cruz (hot cross bun sign) en la atrofia multisistémica. A propósito de 3 casos. Neurología. 2012;27:314–5.