The overload of the healthcare system and the organisational changes made in response to the COVID-19 pandemic may be having an impact on acute stroke care in the Region of Madrid.
MethodsWe conducted a survey with sections addressing hospital characteristics, changes in infrastructure and resources, code stroke clinical pathways, diagnostic testing, rehabilitation, and outpatient care. We performed a descriptive analysis of results according to the level of complexity of stroke care (availability of stroke units and mechanical thrombectomy).
ResultsThe survey was completed by 22 of the 26 hospitals in the Madrid Regional Health System that attend adult emergencies, between 16 and 27 April 2020. Ninety-five percent of hospitals had reallocated neurologists to care for patients with COVID-19. The numbers of neurology ward beds were reduced in 89.4% of hospitals; emergency department stroke care pathways were modified in 81%, with specific pathways for suspected SARS-CoV2 infection established in 50% of hospitals; and SARS-CoV2-positive patients with acute stroke were not admitted to neurology wards in 42%. Twenty four hour on-site availability of mechanical thrombectomy was improved in 10 hospitals, which resulted in a reduction in the number of secondary hospital transfers. The admission of patients with transient ischaemic attack or minor stroke was avoided in 45% of hospitals, and follow-up through telephone consultations was implemented in 100%.
ConclusionsThe organisational changes made in response to the COVID-19 pandemic in hospitals in the Region of Madrid have modified the allocation of neurology department staff and infrastructure, stroke units and stroke care pathways, diagnostic testing, hospital admissions, and outpatient follow-up.
La sobrecarga asistencial y los cambios organizativos frente a la pandemia de COVID-19 podrían estar repercutiendo en la atención al ictus agudo en la Comunidad de Madrid.
MétodosEncuesta estructurada en bloques: características del hospital, cambios en infraestructura y recursos, circuitos de código ictus, pruebas diagnósticas, rehabilitación y atención ambulatoria. Análisis descriptivo según el nivel de complejidad en la atención del ictus (disponibilidad o no de unidad de ictus y de trombectomía mecánica).
ResultadosDe los 26 hospitales del SERMAS que atienden urgencias en adultos, 22 cumplimentaron la encuesta entre el 16 y 27 de abril. El 95% han cedido neurólogos para atender a pacientes afectados por la COVID-19. Se han reducido camas de neurología en el 89,4%, modificado los circuitos en urgencias para ictus en el 81%, con circuitos específicos para sospecha de infección por SARS-CoV2 en el 50%, y en el 42% de los hospitales los pacientes con ictus agudo positivos para SARS-CoV2 no ingresan en camas de neurología. Ha mejorado el acceso al tratamiento, con trombectomía mecánica las 24 h en el propio hospital en 10 hospitales, y se han reducido los traslados interhospitalarios secundarios. Se ha evitado el ingreso de pacientes con ataque isquémico transitorio o ictus leve (45%) y se han incorporado consultas telefónicas para seguimiento en el 100%.
ConclusionesLos cambios organizativos de los hospitales de la Comunidad de Madrid frente a la pandemia por SARS-Co2 han modificado la dedicación de recursos humanos e infraestructuras de las unidades de neurología y los circuitos de atención del ictus, realización de pruebas diagnósticas, ingreso de los pacientes y seguimiento.
There has been a rapid increase in cases of SARS-CoV-2 infection and the associated disease COVID-19 in the region of Madrid since the first case was detected, surpassing hospital capacity. This has led to the need to reallocate human and material resources and to establish specific inpatient wards for patients with the infection, reducing the number of beds available to other medical and surgical departments.
Acute stroke care has been well established in the region of Madrid since the launch of the Madrid Stroke Care Plan,1,2 which establishes priority care for patients with acute stroke by pre-hospital emergency services and hospital emergency departments, admission of these patients to stroke units, and access to reperfusion treatment (intravenous thrombolysis and mechanical thrombectomy) for patients with cerebral infarction. Hospital overload and the organisational changes implemented in response to the COVID-19 pandemic may have affected stroke care, with these patients taking a back seat in the restructuring of the healthcare system as a whole to prioritise patients with COVID-19. In addition to these organisational changes, fear of contracting the infection during hospitalisation for another disease may also have caused delays in seeking care, and consequently in missed opportunities to receive acute stroke care; this situation has been reported in China.3
Key factors affecting outcomes for patients with stroke in a situation like the current pandemic include the risk of exposure to the virus in hospital and reduced access to diagnostic and therapeutic resources due to organisational changes made in response to the pandemic. In addition to ensuring that patients with stroke receive the best possible care, it is essential to protect healthcare professionals against infection. In the light of the above, scientific associations and expert groups, such as the Madrid Stroke multidisciplinary group and its neurology committee, have issued recommendations on healthcare organisation to ensure the quality of stroke care in this historic moment.4–9
However, the unexpected magnitude of the pandemic in our setting and the prioritisation of daily demand for the care of patients with COVID-19 have meant that these organisational changes have been implemented independently in each centre, without a common roadmap; many general hospitals have practically become specialty hospitals attending patients with COVID-19. In this study, we aim to assess the impact of the pandemic on the resources and care circuits allocated to acute stroke care in the region of Madrid.
MethodsThe neurology committee of the Madrid Stroke multidisciplinary group ran a survey addressing 6 issues: (1) hospital characteristics; (2) changes in neurology department infrastructure and human resources; (3) changes in code stroke care; (4) changes in diagnostic testing; (5) rehabilitation; and (6) outpatient care.
In order to achieve the greatest possible coverage of hospitals in the region, the survey was distributed among members of the Madrid Association of Neurology’s Stroke Forum, a working group that includes neurologists and other professionals specialising or interested in stroke; the group has extensive experience in developing care protocols and training and research activities concerning stroke.
The Research Electronic Data Capture (REDCap) software, installed on the servers of the Hospital La Paz Research Institute (IdiPAZ), was used to design the survey and store results. REDCap is a secure web application designed for collecting data in research studies; it has an intuitive interface for data collection and enables data traceability, exportation of data to various statistical analysis applications, and interoperability with external sources.10
ResultsTwenty-two of the 26 hospitals in the Madrid Regional Health Service that attend adult emergency patients responded to the survey between 16 and 27 April 2020. Of these, 8 had stroke units and the facility to perform mechanical thrombectomy (SU + MT hospitals), 4 had stroke units but could not perform mechanical thrombectomy (SU hospitals), and 10 did not have stroke units; therefore, the overall response rate was 84.6% (100% of SU + MT hospitals, 100% of SU hospitals, and 71.4% of hospitals without stroke units).
Below, we summarise the main organisational changes implemented in the different types of hospitals.
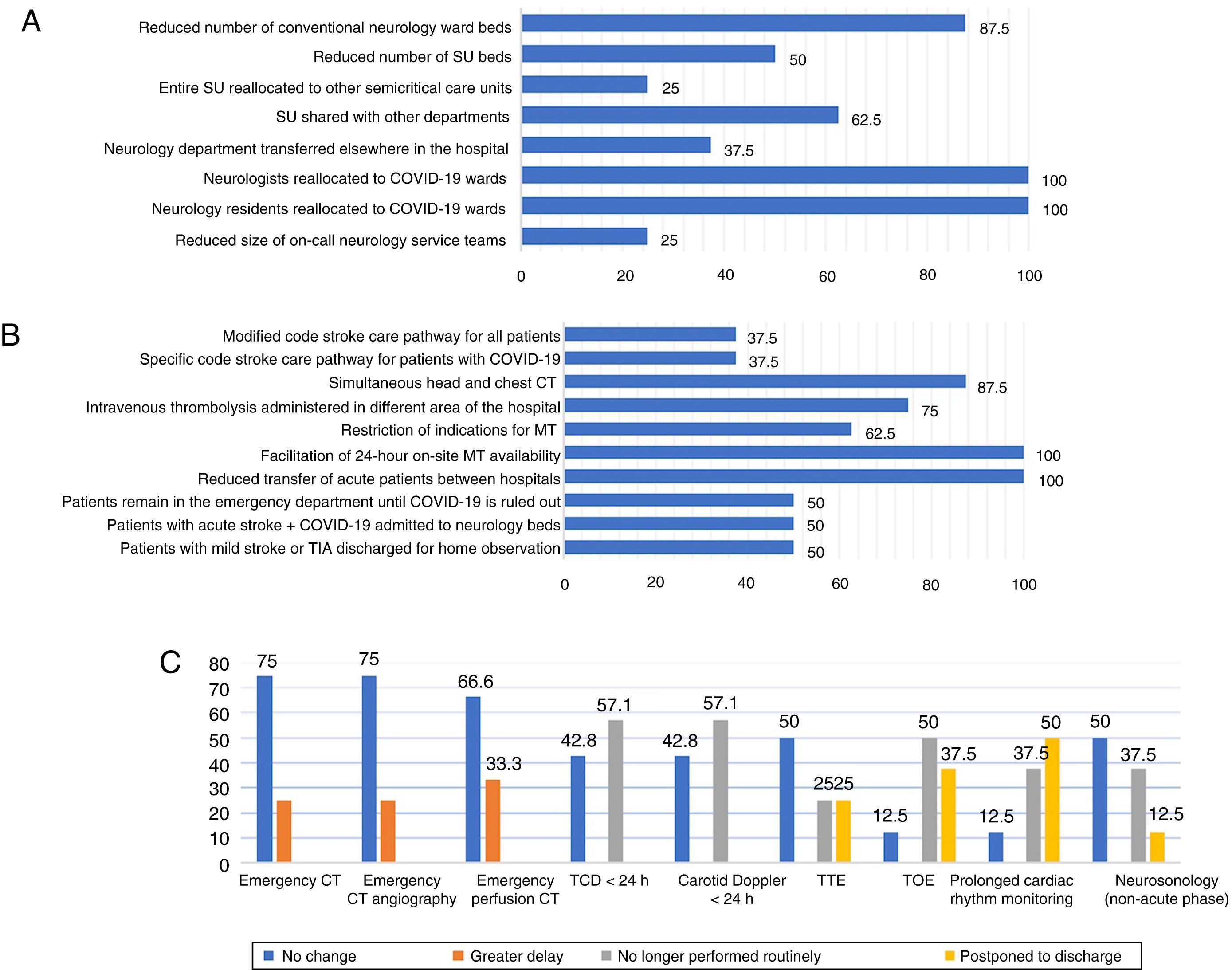
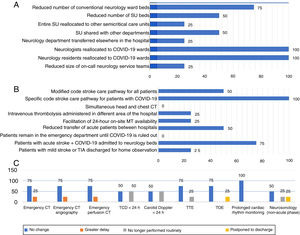
Hospitals with stroke units and mechanical thrombectomy facilitiesIn this group, 87.5% of hospitals reported a reduced number of conventional neurology ward beds; 3 hospitals reallocated the entire department to other areas of the hospital. As is shown in Fig. 1A, 7 hospitals reported changes in the availability of stroke unit beds, either with a reduction in the number of beds, or with beds being shared with other departments; in 2 hospitals, the entire stroke unit was reallocated to other semi-critical care units. Regarding human resources, all SU + MT hospitals reported reallocating staff and residents to COVID-19 wards; the on-call neurology service was run with reduced staff at 2 hospitals.
Changes in care provision in hospitals with stroke units and the facility to perform mechanical thrombectomy. (A) Human and material resources. (B) Code stroke. (C) Diagnostic testing. CT: computed tomography; MT: mechanical thrombectomy; SU: stroke unit; TCD: transcranial Doppler ultrasonography; TIA: transient ischaemic attack; TOE: transoesophageal echocardiography; TTE: transthoracic echocardiography.
Emergency department code stroke pathways were modified for all patients at 3 hospitals, and for patients with initial suspected SARS-CoV-2 infection at another 3; 6 hospitals changed the area in which intravenous thrombolysis was administered. At 7 of the 8 SU + MT hospitals, chest CT was performed simultaneously with head CT with a view to early detection of possible SARS-CoV-2 infection. Regarding mechanical thrombectomy, 5 hospitals modified the criteria for indicating the procedure during the pandemic, and all hospitals reported facilitating its performance at the centre, establishing on-call interventional neuroradiology services to be available on-site at all hours during the weeks of greatest COVID-19 incidence in Madrid. This reduced the number of secondary transfers of patients with stroke between hospitals (Fig. 1B).
At half of these hospitals, patients with acute stroke remained in the emergency department until SARS-CoV-2 infection was ruled out with PCR testing. In 4 hospitals, patients with acute stroke and confirmed infection were admitted to the neurology ward. At half of these hospitals, patients with transient ischaemic attack (TIA) or mild stroke meeting criteria for admission were discharged for observation at home (Fig. 1B).
Changes in diagnostic testing of patients with acute stroke are shown in Fig. 1C. Longer door-to-CT and door-to-CT angiography times are reported in 25% of these centres; similarly, one of the 3 centres that routinely obtains CT perfusion imaging reported delays in performing this test. Neurosonology testing was no longer indicated in the first 24 hours in 57.1% of centres. Regarding cardiology studies, routine transthoracic and transoesophageal echocardiography studies were suspended in 2 hospitals, and postponed until after discharge in a further 2. Half of these hospitals stopped performing transoesophageal echocardiograms as part of the aetiological study during hospitalisation, and another 3 postponed this test. Finally, changes were also reported in prolonged cardiac rhythm monitoring, which was no longer indicated routinely in 3 hospitals and was postponed in 4 (Fig. 1C).
Only one of the 8 SU + TM hospitals reported no changes in rehabilitation treatment of patients with acute stroke. Onset of physiotherapy was delayed in 2 hospitals; the number of in-hospital rehabilitation beds was reduced in one, and outpatient rehabilitation was facilitated in 3. Five hospitals reported greater difficulty transferring patients to medium- and long-term rehabilitation centres; at 2 hospitals, some patients were discharged to their homes without rehabilitation treatment until the end of the pandemic, if the patient’s social and family circumstances allowed for this.
At 7 of the 8 SU + MT hospitals, in-person follow-up of patients with stroke was completely suspended or appointments were rescheduled. All centres were performing telephone follow-up, with one also using video calls where this was considered necessary. The 6 hospitals with neurosonology laboratories stopped scheduling tests for outpatients. Only one of the 8 hospitals in this group had a clinic for patients with TIA, which had substituted in-person consultations for telephone follow-up.
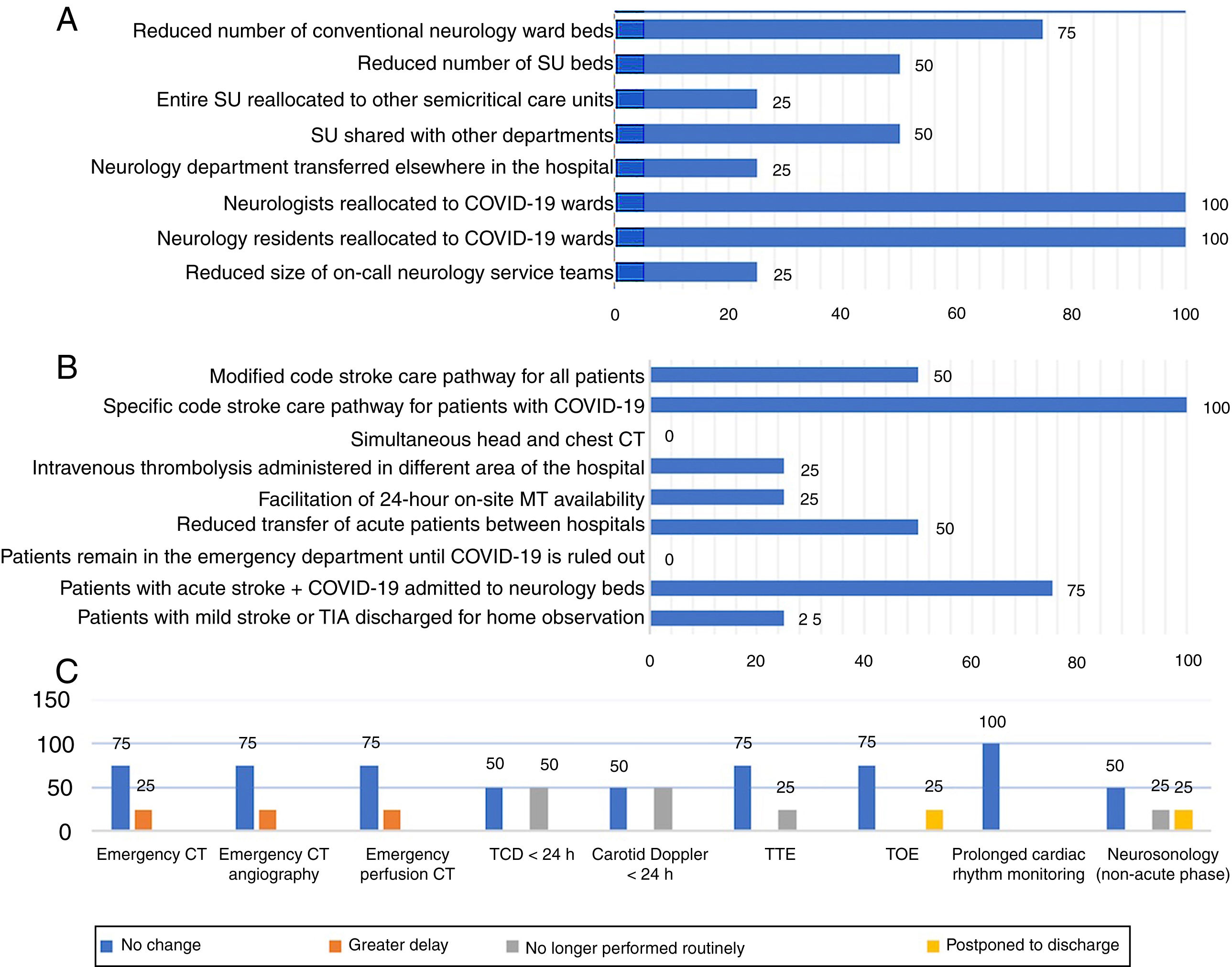
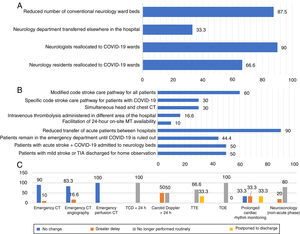
Hospitals with stroke unitsThe COVID-19 pandemic has also led to a reduction in the number of neurology ward beds in hospitals in this group, with neurology department resources being reallocated to other departments in one centre. Stroke unit beds were reduced in half of these hospitals, shared with other departments in 2, and completely reallocated to other departments in one. All 4 hospitals reallocated neurologists to COVID-19 inpatient wards; residents were also reallocated in the 2 hospitals offering neurology residency programmes. Only one of these hospitals reported a reduction in the number of staff on the on-call neurology service (Fig. 2A).
Changes in care provision in hospitals with stroke units. (A) Human and material resources. (B) Code stroke. (C) Diagnostic testing. CT: computed tomography; MT: mechanical thrombectomy; SU: stroke unit; TCD: transcranial Doppler ultrasonography; TIA: transient ischaemic attack; TOE: transoesophageal echocardiography; TTE: transthoracic echocardiography.
Half of the SU hospitals modified their code stroke care pathways, and all 4 had developed an independent pathway for patients with suspected SARS-CoV-2 infection. Unlike in the SU + MT hospitals, none of these centres performed chest CT simultaneously with head CT. In 75% of hospitals in this group, SARS-CoV-2–positive patients were admitted to the neurology ward; no hospital reported that patients with acute stroke remained in the emergency department until results confirming the infection were available. Half of these hospitals reported reduced numbers of interhospital transfers of acute patients; in one hospital, patients with TIA or mild stroke were referred for observation at home (Fig. 2B).
The impact on diagnostic testing was similar to that reported in SU + MT hospitals. Increased door-to-imaging times were reported in one of the 4 hospitals. Half of the hospitals in this group had suspended routine performance of emergency neurosonology studies; one had postponed these tests until after discharge. Cardiology studies were also affected at one of these hospitals: routine transthoracic echocardiography studies were suspended and transoesphageal echocardigrams were postponed. However, none reported changes in the use of prolonged cardiac rhythm monitoring (Fig. 2C).
Only one SU hospital reported no impact on rehabilitation treatment. In 2, onset of physiotherapy had been delayed; one hospital had facilitated outpatient rehabilitation; and one reported exceptional cases of patients being discharged without immediate rehabilitation, where the patient’s social and clinical situation permitted this. Two hospitals reported greater difficulty accessing beds at medium- and long-term rehabilitation facilities.
Regarding outpatient follow-up, in-person consultations were completely suspended in 75% of SU hospitals, and rescheduled in 50%; all centres provide telephone consultations. The 2 hospitals in this group with neurosonology laboratories stopped scheduling these tests for outpatients during the pandemic. Only one hospital has a clinic for patients with TIA, and reported that its activity had not changed.
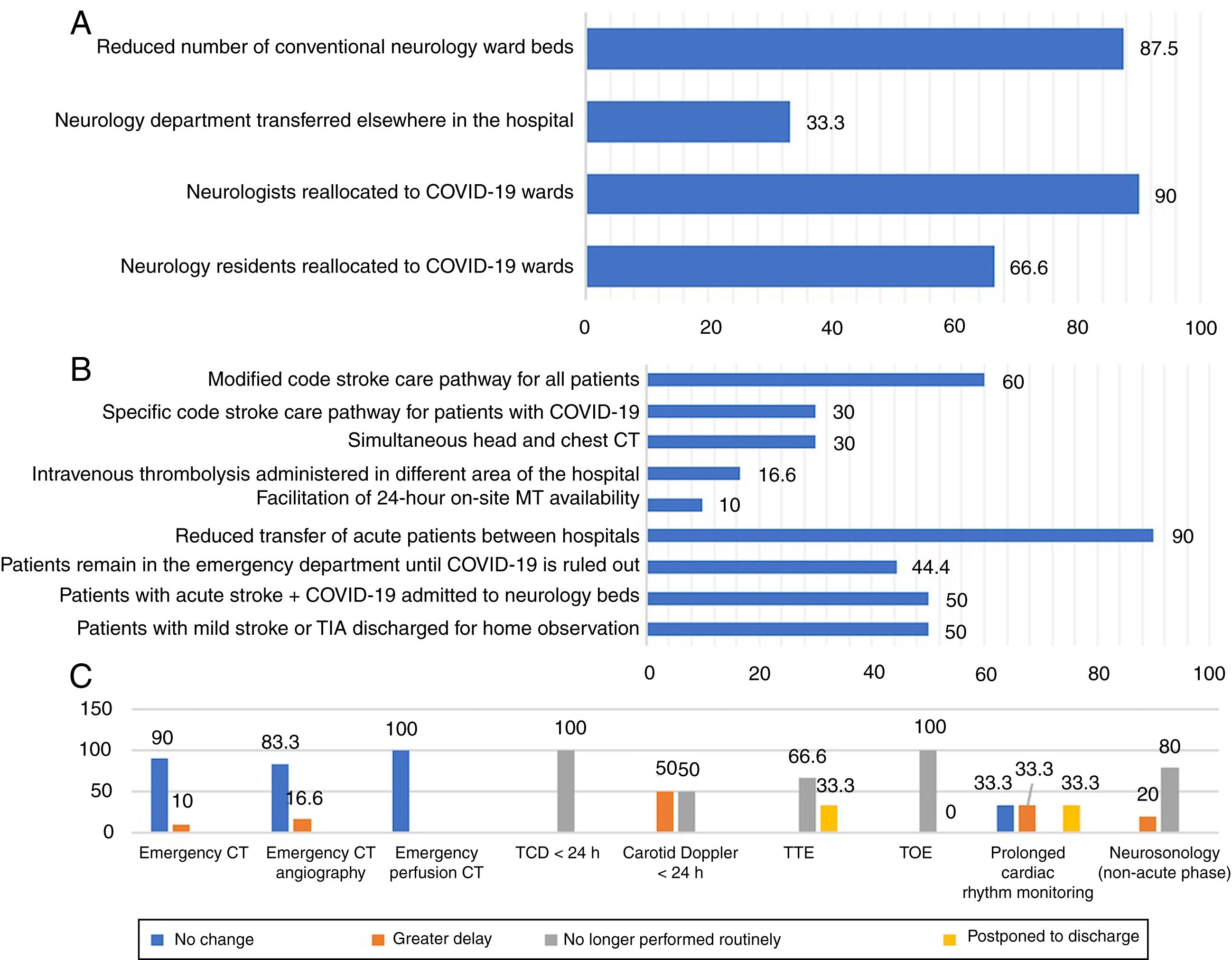
Hospitals without stroke unitsReductions in the number of ward beds assigned to the neurology department were reported by 7 of the 8 hospitals with this resource; in 2 hospitals, beds were reallocated to other departments. In 90% of hospitals without stroke units, neurologists were reallocated to care for patients with COVID-19; residents were also reallocated to COVID-19 wards in 2 of the 3 hospitals offering neurology residency programmes (Fig. 3A). One hospital established a 24-hour on-call neurology service at the beginning of the pandemic.
Changes in care provision in hospitals without stroke units. (A) Human and material resources. (B) Code stroke. (C) Diagnostic testing. CT: computed tomography; MT: mechanical thrombectomy; TCD: transcranial Doppler ultrasonography; TIA: transient ischaemic attack; TOE: transoesophageal echocardiography; TTE: transthoracic echocardiography.
Six hospitals without stroke units modified emergency department care pathways for patients with stroke; however, only 3 established new pathways for patients with acute stroke and suspected SARS-CoV-2 infection. Simultaneous chest and head CT scanning was implemented in 30% of hospitals. In 4 hospitals, patients with stroke remained in the emergency department until results were available from testing for the infection. In half of the hospitals with ward beds assigned to the neurology department, patients with acute stroke and SARS-CoV-2 infection were admitted to these wards. Like at other types of hospital, a reduction was reported in transfers of acute patients between hospitals, and patients with TIA or mild stroke were discharged for home observation (Fig. 3B).
Diagnostic testing and aetiology studies of acute stroke were also affected, but to a lesser extent than in the other types of hospital. For example, only one hospital reported longer delays in performing neuroimaging studies. Transcranial Doppler ultrasound studies were suspended in the 2 hospitals that performed these studies habitually; one of these reported delays in carotid Doppler ultrasound studies. In 3 of these hospitals, routine cardiology studies were suspended or postponed until after discharge. Routine (non-acute–phase) neurosonology studies were suspended in 4 hospitals and delayed in one (Fig. 3C).
Ninety percent of these hospitals reported changes in access to rehabilitation services, with delayed onset of physiotherapy in 60%, reduced numbers of rehabilitation beds and restricted access to medium- and long-term rehabilitation facilities in 20%, and discharges without rehabilitation treatment until the end of the pandemic in 30%.
Finally, 100% of hospitals had suspended in-person follow-up consultations, replacing these with telephone consultations, and 60% had rescheduled consultations for which it was considered necessary for the patient to attend hospital. The only hospital without a stroke unit that had a TIA clinic had suspended this activity.
DiscussionThis study demonstrates the considerable organisational changes implemented in stroke care due to the COVID-19 pandemic in the region of Madrid. With the exception of one hospital without a stroke unit, all hospitals reallocated neurologists to treat patients with COVID-19, either in dedicated wards or in emergency departments. Neurology ward beds were reduced in 89.4% of hospitals. Code stroke protocols were modified in 81% of centres, with the creation of specific pathways for patients with suspected SARS-CoV-2 infection in 50%, and hospitalisation of patients with acute stroke and SARS-CoV-2 infection in beds outside the neurology ward in 42%. In addition to these limitations on care provision, it should be noted that additional resources enabled hospitals to mitigate the difficulties in treating patients with stroke, such as the creation of on-call neurology services at hospitals without stroke units, and increased 24-hour access to mechanical thrombectomy both at the 7 public hospitals with stroke units and facilities to perform this treatment and at another 3 private non-profit hospitals (one in each group). These measures reduced the number of secondary transfers of patients between hospitals.
According to official data from the Madrid regional health ministry, on the last day that surveys were returned (27 April 2020) the cumulative total number of hospital admissions due to COVID-19 since the beginning of the pandemic was 39 634, with 3338 requiring intensive care.11 The region’s health service has a total of 14 334 hospital beds,12 and the maximum number of patients hospitalised at one time reached 15 227 (on 30 March–1 April); this demonstrates the significant organisational effort made, with redistribution of hospital staff to treat patients with SARS-CoV-2 infection, the allocation of the majority of public and private hospital beds for these patients, and the creation of field hospitals and medicalised hotels to absorb the increased demand for admissions. This situation affected the care provided to patients with stroke, as shown by our survey findings.
Some authors have noted a reduction in the number of hospital admissions of patients with stroke as a result of the pandemic,8,13,14 although a 41% increase in mechanical thrombectomy procedures has also been reported.14 Fear of contracting SARS-CoV-2 may explain the reduced rate of code stroke activation by patients.3,8,13 However, unpublished data from the pre-hospital emergency services code stroke registry for the region of Madrid show that in the period from 14 March (declaration of the state of alarm) to 22 April (most recent data available at the time of writing), 167 of these patients were attended: 23 (12%) fewer than in the previous 2 years (185 in 2018 and 195 in 2019). This figure falls within the standard deviation of the mean monthly figure for the last 2 years.
Therefore, pending the results of epidemiological studies confirming whether there truly has been a reduction in the number of hospital admissions due to stroke, we may note another 2 factors contributing to this image. Firstly, patients presenting both stroke and SARS-CoV-2 infection would be admitted to isolation wards and not be recorded as having stroke, as they would not be included in the habitual care pathways for this diagnosis. Secondly, the efforts to avoid admission of patients with TIA or mild stroke, who were discharged home for observation after diagnosis in the emergency department, would mean that they were not recorded on hospital stroke registries. One of our most significant findings is the fact that both of these circumstances occurred in approximately half of hospitals in the region of Madrid. The purpose of these decisions is to minimise the risk of patients with stroke being infected by SARS-CoV-2, which may be an additional risk for poor progression.15 Similar measures have been taken in other countries and healthcare systems.16 However, it is noteworthy that despite recommendations to avoid patients with acute stroke and SARS-CoV-2 infection sharing wards with patients without the infection,9 58% of hospitals admitted these patients to neurology ward beds. This result may be explained by a possible ambiguity in the wording of the questionnaire, which asked whether patients with the infection were admitted to neurology beds; some respondents may have interpreted this as referring to patients admitted under the responsibility of the neurology department, even if the bed was in an isolation ward for patients with COVID-19. Furthermore, while the survey did not specifically address this question, many neurology units created teams of neurologists to care for patients with acute stroke in COVID-19 wards; ad hoc stroke units were even created for patients with COVID-19.
Another interesting finding is the reduction in transfers between hospitals due to stroke: assuming that stroke incidence has not changed, the number of admissions to hospitals with stroke units may have decreased because patients were treated in hospitals without these units. As well as potentially explaining the perceived reduction in incidence during the pandemic, this reduction is the result of an organisational decision intended to decrease the spread of COVID-19 and improve the treatment of patients with severe stroke. This measure was made possible by the general directorate of the Madrid Regional Health Service, which facilitated 24-hour availability of mechanical thrombectomy in the 7 hospitals that normally participate on a rotating weekly schedule to provide emergency mechanical thrombectomy treatment at 3 centres; and centralised the management of medium- and long-term rehabilitation and continued care centres. We should also underscore the efforts of private non-profit hospitals in the care of patients with acute stroke, facilitating access to mechanical thrombectomy.
Given the magnitude of the pandemic and the likelihood that many patients with acute stroke will have SARS-CoV-2 infection at the time of symptom onset, these patients should be treated as possible sources of infection, both for other patients and for hospital staff. Therefore, another recommendation is that chest CT scans should be performed at the same time as the head CT; this may provide data supporting suspicion of SARS-CoV-2 infection before PCR results are available.7,9 This measure was implemented to different extents in different types of hospital: it was adopted in 87.5% of SU + MT hospitals, compared to 0% of SU hospitals and 30% of hospitals without stroke units.
Rehabilitation treatment for stroke was also affected by the pandemic, with delayed onset of physiotherapy in the acute phase, reduced numbers of rehabilitation beds, and the need to discharge patients without completing rehabilitation treatment until this could be done safely, in order to protect patients and staff against the infection. A similar impact on access to rehabilitation treatment has been reported in other countries, including the United States.8
It should also be noted that the pandemic has led to a paradigm shift in the organisation of outpatient care, forcing neurologists to reinvent ourselves, changing our techniques from those of a specialty fundamentally based on direct clinical examination to incorporate telephone consultations and telemedicine.17,18 Another challenge in the management of patients with stroke during the pandemic has been complementary testing in the aetiological diagnosis of ischaemic stroke, particularly in the areas of neurosonology and echocardiography. Nearly half of the hospitals surveyed, regardless of the complexity of stroke care they provide, had stopped performing these tests routinely. This was particularly the case for transoesophageal echocardiography, which had almost completely disappeared during the hospitalisation of patients with stroke.
The main strength of this study is that responses were received from 100% of hospitals participating in code stroke care pathways and 71.4% of hospitals without stroke units (but which receive patients with stroke who arrive by their own means or who present stroke during hospitalisation). In terms of hospital capacity, the survey respondents account for 95.6% of beds at level 1, 2, and 3 hospitals in the Madrid Regional Health Service.
The main limitation is that the results reflect the changes made in a very specific period during the pandemic, when hospital admissions due to SARS-CoV-2 infection began to decrease in the region, and the study does not record the organisational changes currently being made in preparation for potential new outbreaks and the return to normal service in these hospitals.
Therefore, our study group intends to run a second survey at the end of the pandemic to provide an overview of the progression and the results of the organisational changes made in the care of patients with acute stroke in this context. We were also unable to analyse the direct impact on the prognosis of patients attended for stroke during the study period; this should be addressed by future studies based on case registries, differentiating between patients with and without concomitant SARS-CoV-2 infection.
In conclusion, the organisational decisions made in hospitals in the region of Madrid in response to the COVID-19 pandemic have changed the normal functioning of neurology units, in terms of both the allocation of human resources and the availability of hospital infrastructure. Regarding code stroke protocols, hospitals implemented changes in care pathways, diagnostic testing, the wards receiving hospitalised patients, and outpatient follow-up. The lessons learned from this situation should inform contingency plans to provide the best possible care to patients with stroke during similar healthcare emergencies to the COVID-19 pandemic.
FundingThis study has received no specific funding from any public, private, or non-profit organisation.
Conflicts of interestNone.
We would like to thank the Madrid Association of Neurology for distributing the questionnaire, and the neurologists at the following hospitals: Hospital Universitario 12 de Octubre, Hospital Universitario Clínico San Carlos, Hospital Fundación Jiménez Díaz, Hospital General Universitario Gregorio Marañón, Hospital Universitario La Paz-Carlos III-Cantoblanco, Hospital Universitario de La Princesa, Hospital Universitario Puerta de Hierro-Majadahonda, Hospital Universitario Ramón y Cajal, Hospital Central de la Defensa Gómez Ulla, Hospital Universitario de Fuenlabrada, Hospital Fundación Alcorcón, Hospital Universitario de Getafe, Hospital Universitario Infanta Leonor-Hospital Virgen de la Torre, Hospital Universitario Infanta Sofía, Hospital Universitario Príncipe de Asturias, Hospital Universitario Rey Juan Carlos, Hospital Universitario Severo Ochoa, Hospital Universitario de Torrejón, Hospital General de Villalba, Hospital Universitario Infanta Elena (Valdemoro), Hospital Universitario del Henares, Hospital Universitario El Escorial, and Hospital Universitario Infanta Cristina.
Please cite this article as: Fuentes B, Alonso de Leciñana M, Calleja-Castaño P, Carneado-Ruiz J, Egido-Herrero J, Gil-Núñez A, et al. Impacto de la pandemia de COVID-19 en la organización asistencial del ictus. Plan Ictus Madrid Neurología. 2020;35:363–371.