Chronic subdural haematoma in adults (CSDH) has a global crude incidence of 14.1/100,000 per year in our institution captive population. There is no single treatment protocol. In our hospital we choose a minimal invasive technique (trans-marrow puncture) without general anaesthesia due to the age of the population. A descriptive study of patients with CSDH and treatment results, including a laterality analysis, is presented.
Material and methodsWe retrospectively searched patients with (CSDH) between January 1998 and May 2009. The diagnosis was made by neuroimaging techniques in all patients. The preferred treatment was trans-marrow puncture; exceptionally some patients were treated by burr holes or craniotomy.
ResultsWe found 127 patients. Age, gender, midline displacement, hospitalisation days, and number of procedures were not predictive factors of mortality in the first month. A slight majority (55%) of CSDH were on the left side, with no statistically significant difference. There were 6 (4.7%) deaths during hospitalisation. In our series cumulative mortality at six months was 11.8%. Markwalder scale at admission was not a predictive factor of statistically significant mortality. An 80% of the patients received trans-marrow puncture as single procedure was performed on 80% of the patients.
ConclusionsThe results of our study suggest that trans-marrow puncture is an acceptable procedure, with low mortality, and less hospitalisation days and complications. Mortality, associated mechanisms, age, gender, midline displacement are no different than that in others previous publications. We found a higher frequency of haematomas to the left, as in other series. Meta-analysis studied need to be performed to determine more accurately the frequency of this dominance.
El hematoma subdural crónico del adulto (HSDCA) tiene una incidencia bruta global en la población cautiva de nuestra institución (pacientes capitados y planes) de 14,1 casos por 100.000 habitantes/año. No existe un protocolo único de tratamiento. En nuestro hospital, dada la edad avanzada de nuestros pacientes, optamos por una terapia mínimamente invasiva (punción transósea [PTO]) sin anestesia general. El objetivo es realizar un estudio descriptivo de pacientes con HSDCA, analizar la lateralidad y los resultados del tratamiento efectuado.
Material y métodosSe detectaron en forma retrospectiva pacientes con HSDCA internados entre enero de 1998 y mayo de 2009 inclusive. El diagnóstico se basó en neuroimágenes. El tratamiento de elección fue la PTO, realizándose por excepción trepanación o craneotomía.
ResultadosSe identificó a 127 pacientes. La edad, el sexo, el desplazamiento de línea media, los días de internación y el número de procedimientos no fueron factores predictivos de letalidad a los 30 días del diagnóstico. Un 80% de los pacientes recibió PTO como único procedimiento. La mediana de internación estos pacientes fue de 4 días. El 55% de los hematomas fueron izquierdos, sin diferencia estadísticamente significativa. Se registraron 6 defunciones en internación (4,7%). La letalidad acumulada a los seis meses fue del 11,8%. La escala de Markwalder al ingreso no fue predictiva de letalidad estadísticamente significativa.
ConclusionesLos resultados de nuestro estudio sugieren que la PTO es un procedimiento aceptable, de baja letalidad, con escasos días de internación y complicaciones. La letalidad, los mecanismos asociados, la edad, el sexo y el desplazamiento de la línea media no difieren de lo publicado en las diferentes series. Encontramos una mayor frecuencia de hematomas hacia la izquierda, al igual que en las diferentes series, debería realizarse un estudio meta-analítico para determinar con mayor precisión la frecuencia de este predominio.
Chronic subdural haematoma (CSDH) is a relatively common condition in adults. In our environment, the raw overall rate observed was 14.1 cases per 100,000 inhabitants/year (CI 95% 10.6–17.6). The specific rate for women was 11.6 cases per 100,000 inhabitants/year (CI 95% 7.6–15.6), 18.1 CSDH cases per 100,000 inhabitants/year (95% CI 11.8–24.5).1There are reports that include chronic alcohol consumption among the predisposing factors in 21% of cases, antiplatelet intake in 11% and oral anticoagulant therapy in 10%.2–4
There are few studies on the laterality of CSDH. One of them reported that 18% of cases presented a bilateral distribution and 82%, unilateral. Among the unilateral, the left side was more frequent in a statistically significant manner (57.2%).5
There is no definitive treatment protocol. There are different techniques for its treatment, such as craniotomy, minicraniectomy or burr holes.4,6–11 These patients can be treated with methods not requiring general anaesthesia that could be called minimally invasive, such as those used at our centre. A novel minimally invasive technique, SEPS (Subdural Evacuating Port System), has been introduced recently. This method employs local anaesthesia connected to a reservoir that uses negative pressure, unlike the method which we apply.12
The mortality rate reported in different series varies from 0.21% to 15.6%.2,3,13
The objective of this study was to describe a series of CSDH patients of advanced age, analyse their risk factors and laterality and evaluate the results of their treatment.
Material and methodsUsing the database of Hospital Privado de Comunidad and of the Neurosurgery Service of the centre, we retrospectively identified patients who were diagnosed by computed tomography (CT) and/or brain magnetic resonance imaging (MRI) between 01 January 1998 and 31 May 2009.
Chronic subdural haematoma was defined based on image characteristics. Inclusion criteria for CT were: convex, hypodense, crescent-shaped images adjacent to brain parenchyma. The criteria for MRI were: hyperintense, images on T1 and T2 adjacent to the parenchyma, biconvex, crescent-shaped or multiloculated below the dura mater.
The following independent variables predictive of mortality at the first, third and sixth months were recorded on admission: gender, age, Markwalder scale (MW),14 midline displacement in image, length of hospitalisation, coagulopathy, oral anticoagulation, alcohol intake and number and type of procedures.
The laterality was described and a literature search in PubMed and Lilacs was conducted, from which we selected series of studies on subdural haematoma that had taken laterality into account as a variable to be analysed (search criteria: location, laterality, chronic subdural haematoma, subdural haematoma without limitations of age, time or region).
The surgical treatment of choice was trans-marrow puncture (TMP). Some patients underwent burr holes and/or craniotomy. The trans-marrow puncture technique was performed in a sterile environment, under local anaesthesia with 2cm3 lidocaine, piercing the skull with a catheter over a number 14 needle (Abbocath®), puncture of the haematoma with a number 19 butterfly needle, measuring intracranial pressure and drainage to the exterior connected to a closed collection system without aspiration.
Statistical analysisWe performed a descriptive statistical study of the independent variables through frequencies (absolute and percentage), median (M), quartiles, upper limit and lower limit. We also performed univariate logistic regression analysis to determine the predictive value of MW mortality on the first, third and sixth months after diagnosis. The statistical program used was Arcus QuickStat (Biomedical 1.0).
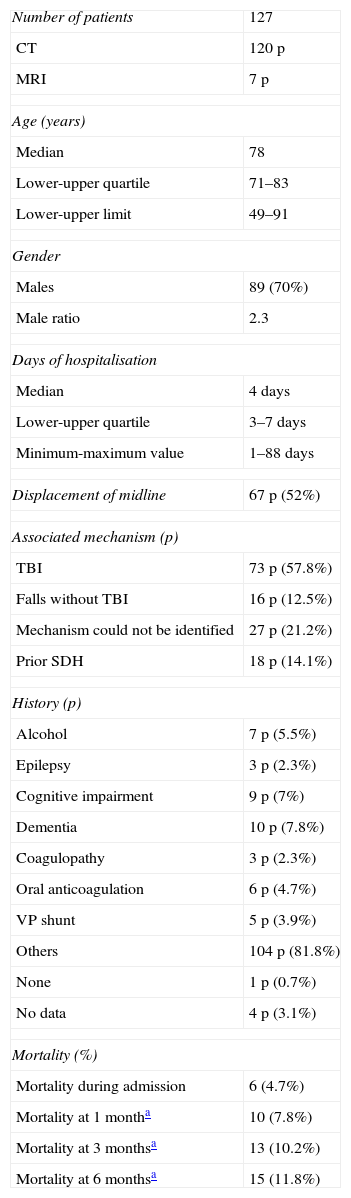
ResultsWe identified 127 patients (p) with a diagnosis of chronic subdural haematoma. The characteristics of the patients upon admission are shown in Table 1. The most commonly associated mechanism was traumatic brain injury (TBI), in 57.8% of cases.
Patient characteristics.
| Number of patients | 127 |
| CT | 120 p |
| MRI | 7 p |
| Age (years) | |
| Median | 78 |
| Lower-upper quartile | 71–83 |
| Lower-upper limit | 49–91 |
| Gender | |
| Males | 89 (70%) |
| Male ratio | 2.3 |
| Days of hospitalisation | |
| Median | 4 days |
| Lower-upper quartile | 3–7 days |
| Minimum-maximum value | 1–88 days |
| Displacement of midline | 67 p (52%) |
| Associated mechanism (p) | |
| TBI | 73 p (57.8%) |
| Falls without TBI | 16 p (12.5%) |
| Mechanism could not be identified | 27 p (21.2%) |
| Prior SDH | 18 p (14.1%) |
| History (p) | |
| Alcohol | 7 p (5.5%) |
| Epilepsy | 3 p (2.3%) |
| Cognitive impairment | 9 p (7%) |
| Dementia | 10 p (7.8%) |
| Coagulopathy | 3 p (2.3%) |
| Oral anticoagulation | 6 p (4.7%) |
| VP shunt | 5 p (3.9%) |
| Others | 104 p (81.8%) |
| None | 1 p (0.7%) |
| No data | 4 p (3.1%) |
| Mortality (%) | |
| Mortality during admission | 6 (4.7%) |
| Mortality at 1 montha | 10 (7.8%) |
| Mortality at 3 monthsa | 13 (10.2%) |
| Mortality at 6 monthsa | 15 (11.8%) |
SDH: subdural haematoma; TBI: traumatic brain injury.
p: patients.
There were 6 (4.7%) hospital deaths, 2 due to respiratory infection, 1 from heart disease and prolonged mechanical ventilation, 1 due to coagulopathy, 1 due to intracranial haemorrhage and 1 due to general deterioration and sepsis.
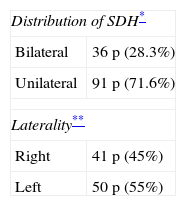
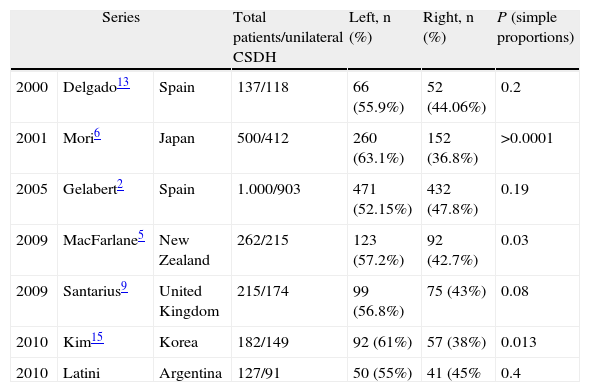
We found 91 patients with unilateral distribution; 41 (45%) presented haematoma on the right side and 50 (55%) on the left side. We did not find statistically significant differences (Table 2).
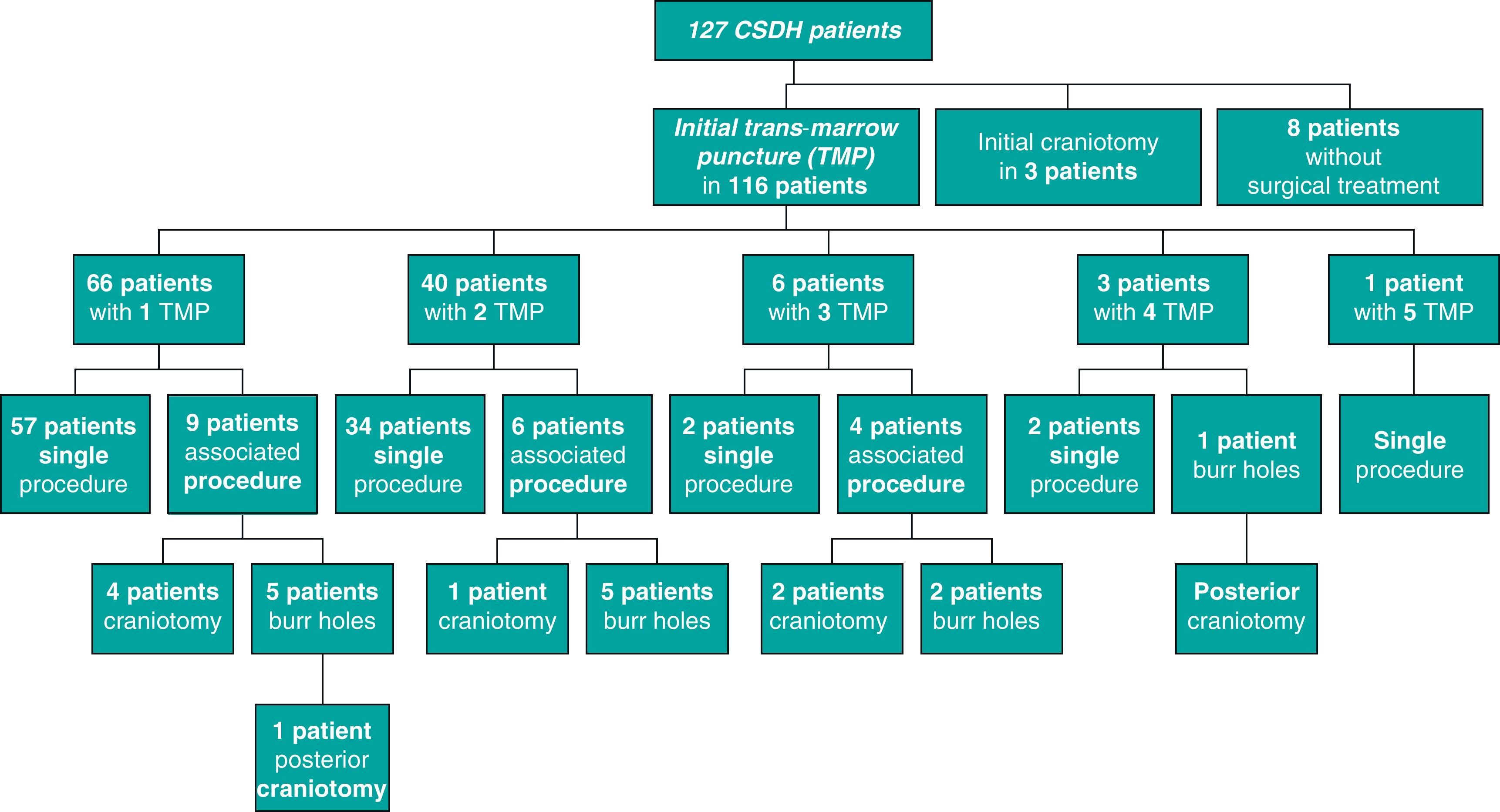
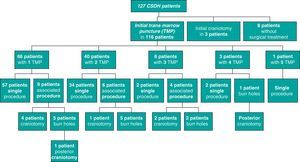
As for the type of treatment, 116 patients received TMP as initial treatment, 3 underwent craniotomy and an expectant attitude was maintained with 8; all data are presented in Fig. 1. Only 57/116 patients (49%) required a TMP as a final procedure; 39/116 (33%) required more than 1 TMP, without the need for other, more invasive techniques such as burr holes or craniotomy; 20/116 patients (17%) required another procedure due to failure of the TMP (burr holes [8 patients] and/or craniotomy [5 patients]). Since the TMP was associated with local anaesthesia and the burr hole-craniotomy was associated with general anaesthesia, 96/119 patients (80.6%) did not require the latter.
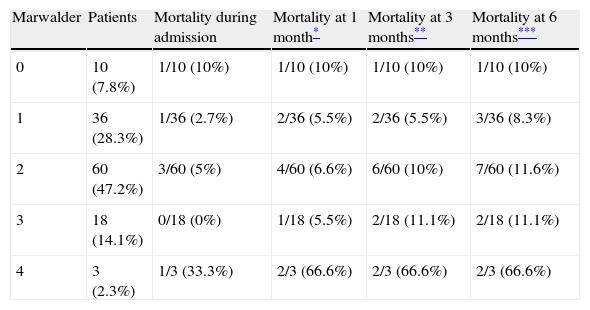
Age, gender, midline displacement, days of hospitalisation and number of procedures were not predictors of mortality at 1 month of discharge. The MW scale at admission was not predictive of mortality in a statistically significant manner (Table 3).
Accumulated mortality by Markwalder scale on admission.
| Marwalder | Patients | Mortality during admission | Mortality at 1 month* | Mortality at 3 months** | Mortality at 6 months*** |
| 0 | 10 (7.8%) | 1/10 (10%) | 1/10 (10%) | 1/10 (10%) | 1/10 (10%) |
| 1 | 36 (28.3%) | 1/36 (2.7%) | 2/36 (5.5%) | 2/36 (5.5%) | 3/36 (8.3%) |
| 2 | 60 (47.2%) | 3/60 (5%) | 4/60 (6.6%) | 6/60 (10%) | 7/60 (11.6%) |
| 3 | 18 (14.1%) | 0/18 (0%) | 1/18 (5.5%) | 2/18 (11.1%) | 2/18 (11.1%) |
| 4 | 3 (2.3%) | 1/3 (33.3%) | 2/3 (66.6%) | 2/3 (66.6%) | 2/3 (66.6%) |
Logistic regression.
In our series, the MW scale was not predictive of cumulative mortality at 1, 3 and 6 months after discharge. The most commonly associated mechanism was TBI without loss of consciousness level; it was found in 57.8% of cases, with a similar frequency to that reported in different series. Falls without TBI as an associated mechanism were found in 12.5% of cases. We believe that patients should be questioned on this particular background during the neurological consultation because it is often not mentioned spontaneously during the anamnesis.
As for the background in our series, alcohol intake had a frequency of 5.5% and anticoagulation of 47%. Both values were below those reported in other series.
The literature search found 6 studies from the year 2000 to the present day, from which we could obtain data on laterality.2,5,6,9,13,15 Of the selected studies, there were 2 Spanish works with 500 and 137 patients, 1 British with 215 patients, 1 Japanese with 500 patients, 1 Korean with 182 patients and 1 from New Zealand with 262 patients. All of them found a higher frequency of left haematomas. Data analysis found a statistically significant difference in laterality in the studies from New Zealand, Korea and Japan, with P=.03, P=.013 and P<.0001, respectively. The 2 Spanish series and the British one did not present statistically significant differences for right and left haematomas. Our series behaved like the other European series (Table 4).2,9,13
Laterality in the different series.
| Series | Total patients/unilateral CSDH | Left, n (%) | Right, n (%) | P (simple proportions) | ||
| 2000 | Delgado13 | Spain | 137/118 | 66 (55.9%) | 52 (44.06%) | 0.2 |
| 2001 | Mori6 | Japan | 500/412 | 260 (63.1%) | 152 (36.8%) | >0.0001 |
| 2005 | Gelabert2 | Spain | 1.000/903 | 471 (52.15%) | 432 (47.8%) | 0.19 |
| 2009 | MacFarlane5 | New Zealand | 262/215 | 123 (57.2%) | 92 (42.7%) | 0.03 |
| 2009 | Santarius9 | United Kingdom | 215/174 | 99 (56.8%) | 75 (43%) | 0.08 |
| 2010 | Kim15 | Korea | 182/149 | 92 (61%) | 57 (38%) | 0.013 |
| 2010 | Latini | Argentina | 127/91 | 50 (55%) | 41 (45% | 0.4 |
Mortality during admission in our series was 4.7% and cumulative mortality at 6 months was 11.8%, similar to some publications.3,8 A recent study of patients with ages similar to those in our series reported a mortality rate of 26.3% at 6 months.16 We believe that the mortality rate is low, taking into account our sample age.
A recent randomised controlled study that compared 2 cases treated with burr holes with and without subsequent drainage found that the recurrence rate in the drainage group was 9% versus 24% in the control group, with a statistically significant lower mortality for the first group.9 A recent study found a lower rate of recurrences with longer drainage time.17
With respect to minimally invasive techniques, a study in 85 patients showed that the failure rate for SEPS was 26%.18 A second case-control study comparing treatment via SEPS (28 patients) and burr holes (57 patients) found no statistically significant differences between the mortality or recurrence rates of the 2 groups.18
In our series, the failure rate for TMP was 17%. Given that TMP is a simpler and less invasive technique that avoids general anaesthesia in all cases, we understand that the requirement of more than 1 puncture involves no greater risk or complications for the patient.
Trans-marrow puncture is a safe treatment with low morbidity, which we believe should be used in elderly patients.
ConclusionsCase mortality, associated mechanisms, age, gender and midline displacement did not differ from those published in different series.
In our series we found left haematomas more often, as was also the case in other publications.
A meta-analytical study should be conducted to determine the frequency of left predominance more accurately. Possible factors proposed to explain this phenomenon include the mechanism of production and a higher rate of events on the left side and/or less clinical suspicion and therefore fewer diagnosed cases of chronic subdural haematomas on the right side. A recent Korean study suggests that laterality could be related to the asymmetry of the skull.
While there are less randomised controlled trials regarding the best treatment for CSDH, the results of our study suggest that TMP is an acceptable, low cost technique, with low mortality and complication rates and with few days of hospitalisation.
Recent publications found that drainage without aspiration was associated with lower mortality and recurrence rates; although the technique is different, TMP also involves placement of drainage without aspiration, suggesting that it might be more beneficial than other techniques without drainage. The SEPS technique showed a higher failure rate than reported in our series and uses negative pressure drainage. The TMP technique has a minimal cost and can be performed with items routinely used in hospitals.
We suggest the need for a randomised controlled study that compares this technique with SEPS and burr holes with drainage.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Latini MF, et al. Tratamiento mínimamente invasivo del hematoma subdural crónico del adulto. Resultados en 116 pacientes. Neurología. 2011;27:22–7.
Presented as a poster at the Congreso Argentino de Neurología, in 2009.