As a result of neurophysiological injury, stroke patients have mobility limitations, mainly on the side of the body contralateral to the lesioned hemisphere. The purpose of this study is to quantify motor compensation strategies in stroke patients during the activity of drinking water from a glass.
Material and methodsFour male patient with cerebrovascular disease and four right-handed, healthy male control subjects. The motion analysis was conducted using the Vicon Motion System® and surface electromyography equipment ZeroWire Aurion®. We analysed elbow, shoulder and trunk joint movements and performed a qualitative analysis of the sequence of muscle activation.
ResultsTrunk, shoulder and elbow movements measured in the stroke patient along the sagittal plane decreased during the drinking from a glass activity, whilst the movements in the shoulder in the coronal plane and trunk increased. As for the sequence of muscle activation, anterior, middle and posterior deltoid all contracted in the patient group during the task, whilst the upper trapezius activation remained throughout the activity.
ConclusionsQuantitative analysis of movement provides quantitative information on compensation strategies used by stroke patients, and is therefore, clinically relevant.
Consecuentemente a la lesión neurofisiológica, los pacientes con ictus presentan limitaciones motoras principalmente en el hemicuerpo contralateral al hemisferio lesionado. El objetivo de este trabajo es cuantificar las estrategias motoras de compensación que ocurren en la extremidad superior afectada en pacientes con ictus durante la actividad de beber agua de un vaso.
Material y métodosCuatro pacientes con ictus y cuatro sujetos controles, sin patología y diestros. El análisis del movimiento se realizó usando el sistema VICONmotion System® y el equipo de electromiografía de superficie Aurion ZeroWire®. Se analizaron los movimientos articulares del codo, el hombro y el tórax. Se realizó un análisis cualitativo de la secuencia de activación muscular.
ResultadosSe observó una disminución de las amplitudes articulares en el plano sagital del codo y el hombro durante la actividad de beber en el grupo de casos; sin embargo, las amplitudes articulares del tronco y el hombro en el plano frontal fueron mayores con respecto a los sujetos controles. En cuanto a la secuencia de activación muscular, deltoides anterior, medio y posterior, se contrajeron en el grupo de pacientes conjuntamente durante la tarea, mientras que el trapecio superior mantuvo su activación durante toda la actividad.
ConclusionesEl análisis cuantitativo del movimiento ofrece información cuantitativa acerca de las estrategias de compensación que realizan los pacientes con ictus, y por tanto, su relevancia clínica es importante.
Studying upper extremity range of motion using 3D kinematic analysis and surface electromyography (EMG) may come to be an important tool for clinical decision-making and measuring results in patients with cerebrovascular accidents (CVA).1 Compared to gait analysis, 3D analysis of the upper extremities presents an array of difficulties. Firstly, the upper extremities do not engage in only one relevant functional activity. Secondly, the functional activities of upper extremities vary greatly within the general population, unlike gait, which follows a typical pattern. Third, the upper extremities, and the shoulder joint in particular, have a very wide range of motion compared to the lower extremities. All of these factors make movement analysis of the upper extremities very problematic. Upper extremity kinematics have been studied previously.2 Until now, however, no studies have examined the function of the upper extremities using 3D systems. Previous studies have analysed daily life activities (DLA) in healthy subjects3–6 and in patients with various neurological conditions.7–10 Few studies of CVA patients evaluate kinematics in DLA,11,12 and to our knowledge, none of those studies uses EMG activity in its analysis.
This cerebrovascular lesion affects brain areas and structures (the basal ganglia, for example) which are directly involved in performing DLA. Throughout the process of learning to creep, crawl and walk upright, these structures create priority pathways for extremity nerve roots. These pathways will constitute the easiest instructions for synchronising hand movements.13,14 A hand movement to carry out a specific task originates in the cortex, but the position of the wrist, elbow and shoulder is adopted according to the basal ganglia's motor schemas. Additionally, the cerebellum, which is the motor coordination centre, is closely linked to these activities and facilitates cortical activity in distal movement. The motor system's continuous processing of afferent sensory signals prepares for motor actions and refines the performance of fine motor tasks. Through this continuous processing, the central nervous system (CNS) gathers information proceeding from a number of sensory channels, thereby enabling completion of specific tasks.15
Following the physiological brain lesion, CVA patients mainly present motor limitations on the side of the body contralateral to the damaged hemisphere. This means that changes occur in motor patterns for the upper extremity on the affected side, which is contralateral to the damaged brain hemisphere, as well as in the trunk and the upper extremity ipsilateral to the damaged brain hemisphere.16 In any case, the body develops compensatory motor strategies, and repetitive use of these strategies may cause musculoskeletal disorders. Measuring existing motor limitations and compensatory motor strategies lets us target the motor disorder precisely,11 and therefore decreases the need for developing compensatory motor strategies.
ObjectiveThe purpose of this study is to analyse the kinematic and chronological differences in muscle activation that may be present in CVA patients and healthy subjects in the task of drinking water from a cup. Our study's hypothesis is that the upper extremity limitations in CVA patients will produce a compensatory motor strategy in patients when they drink water from a cup. This compensatory strategy will affect other muscles, mainly those in the trunk. Additionally, we believe that the muscle activation sequence will vary in order to compensate for the muscles specific to the motor pattern.
Material and methodsSubjectsFour male patients aged 42±5.6 years with CVA in the territory of the middle cerebral artery and a predominance of brachial hemiparesis. All patients were right-handed and hemiparetic on the right side. Patients met the following inclusion criteria: ability to manipulate most objects with only minor limitations on task performance quality or speed, spasticity less than or equal to 2 on the modified Ashworth scale, ability to understand instructions and actively participate in tasks and ability to walk upright (Berg score greater than 21). We excluded patients with cognitive decline, sensory aphasia, visual impairment, behavioural disorders, articular rigidity, irreversible contractures and dysmetria, and any subjects who had been treated with botulinum toxin or baclofen less than 3 months before the start of the study. We also recruited 4 healthy right-handed males aged 45±3.8 years as control subjects. All subjects received information about the experimental procedures that would be carried out. Their consent was obtained in order for them to participate in the study.
InstrumentsThe 3D movement analysis was performed using an optoelectronic system with 8 cameras (VICON® Motion System, Oxford Metrics, Oxford, UK). We used passive reflected markers placed at the following validated anatomical locations17: C7, T10, manubrium, xiphoid process, acromion, right scapula, middle third of the upper arm, epicondyle, middle third of the forearm, radial styloid process, ulnar styloid process and third metacarpal head. Movement was registered with a frequency of 100Hz. The muscle activation sequence was analysed using a surface EMG unit (Aurion ZeroWire, 1000Hz). We examined the following muscles: superior trapezius, deltoids (anterior, medial and posterior fibres), biceps brachii and triceps brachii.
Measurements were taken in the laboratory for movement, biomechanics, ergonomics and motor control analysis (LAMBECOM in Spanish) at Universidad Rey Juan Carlos.
Experimental procedureSubjects were instructed to perform the task of drinking water from a cup as a basic daily life activity (BDLA). Materials were an adjustable-height table, an adjustable-height chair with no backrest and a standard cup.
Subjects were seated before the table with knees and hips flexed 90°. The upper extremity was initially placed with the shoulder in a neutral position and the elbow and hand flexed 90° against the table with the forearm pronated. The cup (15cm tall×5.5cm in diameter) was placed on the table in front of the patient's sternum at a distance equal to 75% of the maximum reach of the patient's arm. A small amount of water was added to the cup (100mL).
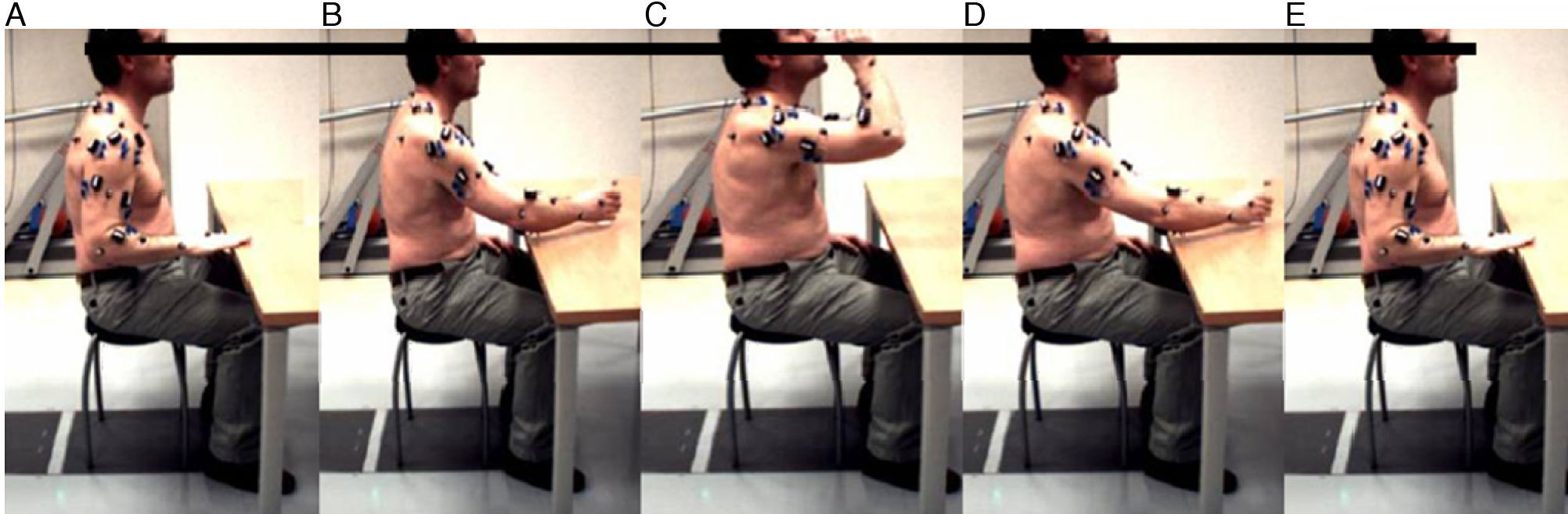
The activity was divided into 5 tasks or events. Starting at the initial position, the patient began capture by moving the hand to the cup, grasping the cup, lifting the cup to the lips, returning the cup to the table, releasing the cup, and returning the hand to its original position (Fig. 1).
(A) From the initial position, the subject begins the capture process by moving the hand to the cup. (B) Subject captures the cup, (C) subject lifts the cup to the lips, (D) subject returns the cup to the table and (E) subject releases the cup and the hand resumes its initial position.
We analysed the articular movements of the elbow, shoulder and thorax. The maximum and minimum angular range of motion (ROM) was calculated for each articulation. The non-parametric Mann–Whitney test was used to compare the 2 groups; the significance level was P<0.05. We performed a qualitative analysis of the muscle activation sequence during the task of drinking (contraction–no contraction). Results were obtained by averaging 5 completed tests.
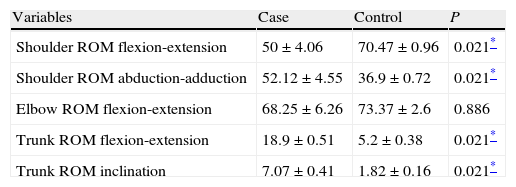
ResultsWe observed a decreased range of motion along the sagittal plane of the elbow and shoulder during a drinking task in CVA patients with respect to healthy subjects. These differences had a significant effect on the shoulder joint range of motion. Trunk articulation ranges of motion were significantly larger in patients than in control subjects. This was also true for shoulder range of motion along the frontal plane (Table 1).
Articular range of motion of the upper extremity and trunk during the drinking task.
| Variables | Case | Control | P |
| Shoulder ROM flexion-extension | 50±4.06 | 70.47±0.96 | 0.021* |
| Shoulder ROM abduction-adduction | 52.12±4.55 | 36.9±0.72 | 0.021* |
| Elbow ROM flexion-extension | 68.25±6.26 | 73.37±2.6 | 0.886 |
| Trunk ROM flexion-extension | 18.9±0.51 | 5.2±0.38 | 0.021* |
| Trunk ROM inclination | 7.07±0.41 | 1.82±0.16 | 0.021* |
Data are presented as mean±standard deviation. ROM: range of movement (degrees).
The most significant differences observed in the muscle activation sequence were in the superior trapezius, which was activated during the entire task in the CVA patient group. However, in healthy subjects, it was only activated during the steps of lifting the cup to the lips and returning it to the table. The anterior, medial and posterior deltoid fibres were activated and co-contracted in CVA patients during the first 3 steps of the drinking task: beginning the capture process by moving the hand from its initial position to the cup, grasping the cup, and lifting it to the lips. In control subjects, deltoid activity was more specific. Anterior fibres were mainly activated in 2 steps of the activity: beginning the capture process by moving the hand from its initial position to the cup, and grasping the cup. Medial fibres were activated during the steps of transporting the cup to the lips and returning it to the table. Lastly, posterior deltoid fibres were only activated during the last step of the task, which was releasing the cup and returning the hand to its initial position. The biceps brachii showed similar activation sequences in both groups. However, there were differences in the activation sequences of the triceps brachii. In CVA patients, this muscle activated during 2 events: beginning the capture process by moving the hand from its initial position to the cup, and transporting the cup to the lips. In the control group, the triceps was not activated during transport of the cup, but rather during the last step, that is, releasing the cup and returning the hand to its initial position. In the patient group, we observed activation of the extensor and flexor muscles of the wrist during the steps of grasping and releasing the cup. In the control subjects, wrist extensors were activated in the steps of grasping and releasing the cup, and wrist flexors were mainly activated during transport of the cup to the lips.
DiscussionThe purpose of this study was to analyse 3D kinematics and the muscle activation sequence of the upper extremity during the task of drinking from a cup in both CVA patients and healthy subjects.
The main finding is decreased joint range of motion along the sagittal plain of the upper extremity in CVA patients compared to controls, which was anticipated. Decreased range of motion affects the two analysed articulations (shoulder and elbow), and this complicates the task of drinking by making movement less fluid and increasing the risk of dropping the cup. This deficit is compensated for through an increase in trunk motion, with larger ranges of motion for flexion-extension and inclination. Along the frontal plane of the shoulder, abduction–adduction range of motion increases, which aids in performing the activity and completing the task of drinking the water in the cup.
Results from the study by Murphy et al.11 coincide with our own in that stroke patients demonstrated increased shoulder abduction and decreased elbow extension, in addition to increased anterior displacement of the trunk. Other studies18,19 have also observed increased mobilisation of the trunk in stroke patients performing reaching activities. Increased mobilisation of the trunk in stroke patients has been reported as an indicator of greater severity.20 Functional evaluations of stroke patients should therefore include an analysis of trunk displacement.
The muscle activation sequence reported by EMG describes activity chronologies that differ between control subjects and CVA patients. The latter show a compensation pattern that is mainly driven by the superior trapezius. In patients with CVA, the deltoid fibres show poorly disassociated activity. Deltoid fibres are mainly responsible for completing the first steps in the task. These initial steps, which include beginning the activity, extending the arm and raising the arm to bring the hand to the mouth, take place less fluidly, one by one. There is a decrease in synergic activity by the superior trapezius and the different deltoid fibres. Posterior fibres of the deltoids and triceps brachii in stroke patients do not participate in the last steps in the activity (lowering the arm and returning it to its original position) as they do in control subjects. These motions are performed by the superior trapezius. Therefore, the motion of descending and retracting the upper extremity to return it to its initial position, driven in control subjects by posterior fibres in the deltoids and triceps, is driven by the muscle action of the superior trapezius in stroke patients.
At present, some authors state that techniques based on recovering movement are less effective than those based on compensation mechanisms.21 Studies using surface EMG and 3D kinematic analysis to evaluate DLAs provide sufficient information about impaired muscles and limited joint range of motion during performance of an activity. At the same time, they deliver information about the muscles involved in compensation strategies, and their joint kinematics. By knowing which muscles are active, which are deficient, and what kinematic compensation strategies are used, we can design specific treatment with no need to recur to compensatory therapy methods.
The limits of the study are the number of movements and list of DLAs that were analysed. This is a pilot study within a line of research whose objectives include expanding the sample size, analysing other joints such as the wrist, evaluating other planes of motion and measuring other highly relevant variables such as joint kinetics and muscle strength. In addition, studies including data from both impaired and healthy upper extremities provide information about the biomechanical or neuroplastic origin of movement disorders in the side of the body ipsilateral to the lesioned brain hemisphere.16
The knowledge we gather from optoelectronic movement analysis systems together with surface EMG is fundamental in order to make clinical decisions and monitor the patient properly. A 3D analysis of the movements required to drink from a cup permits precise measurement of the ranges of motion of the articulations involved in performing this daily life activity.
Conflicts of interestThis study was carried out as part of the research project Hybrid NeuroProsthetic and NeuroRobotic Devices for Functional Compensation and Rehabilitation of Motor Disorders (HYPER) within the programme CONSOLIDER-Ingenio 2010 and the 6th Spanish National Plan for scientific research, development and technological innovation 2008–2011.
Please cite this article as: Molina Rueda F, et al. Análisis del movimiento de la extremidad superior hemiparética en pacientes con accidente cerebrovascular: estudio piloto. Neurología. 2012;27:343–7.