Giant cell arteritis (GCA) is an immuno-mediated systemic type of vasculitis affecting medium- and large-calibre blood vessels. Its histopathology is characterised by an initial inflammatory process which may lead to vascular occlusion. GCA is the most frequent type of vasculitis in adults. Typical clinical manifestations include headache, jaw claudication, and polymyalgia rheumatica. Stroke is a less frequent form of presentation.
Magnetic resonance angiography (MRA) and arteriography may display non-specific alterations in blood vessels. Biopsy of the temporal artery continues to be the gold standard for diagnosis. According to recent studies, positron emission tomography (PET) may be a useful diagnostic tool for inflammatory diseases such as GCA.1,2
We present the cases of 2 patients with symptoms of CNS vasculitis; in these cases, a vascular study with 18F-FDG PET/CT helped diagnose GCA.
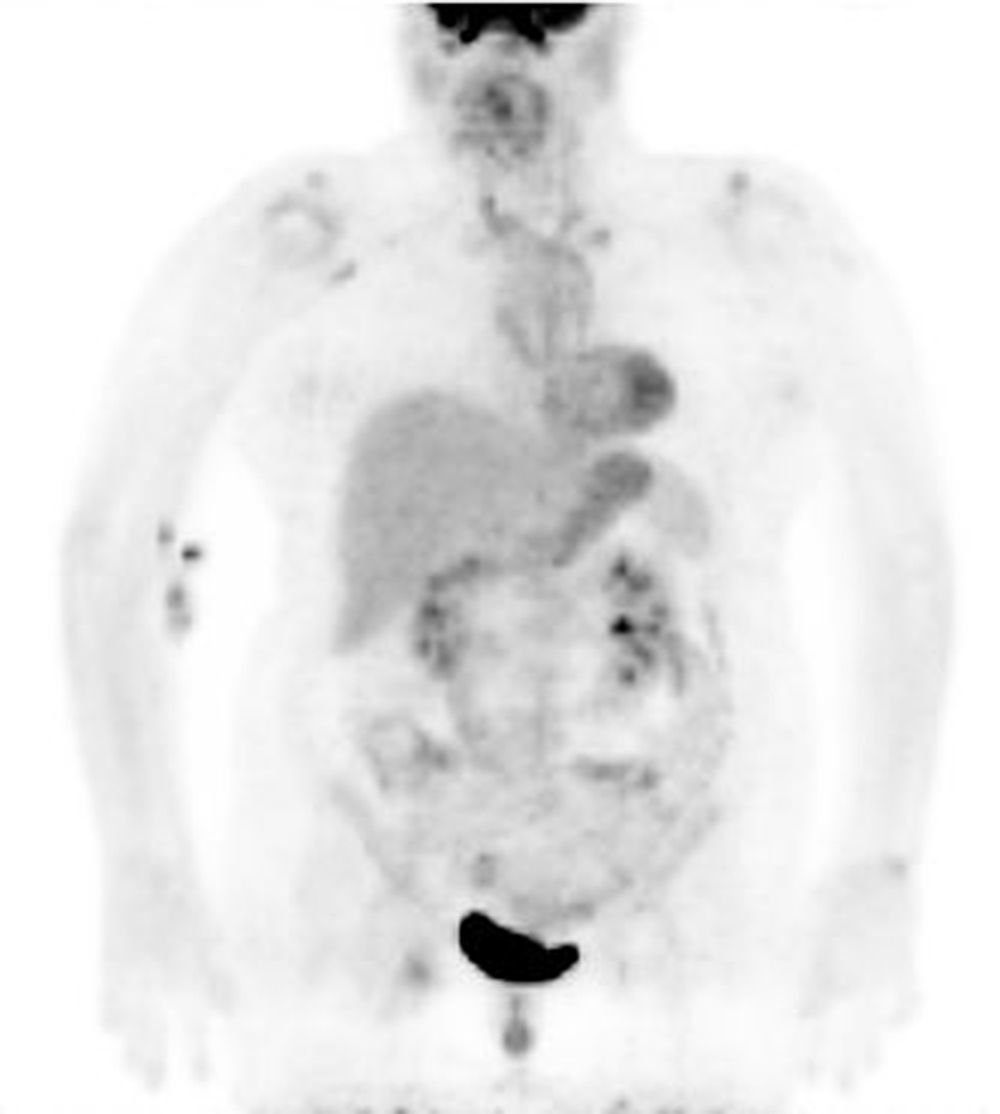
Patient 1Our first patient, a 67-year-old woman, was admitted to the neurology department due to a one-week history of progressive right hemiparesis. She had no history of headache, jaw claudication, fever, or systemic symptoms. Basic laboratory tests, an immunology study, and a CSF test yielded normal results. She displayed an ESR of 43mm/h. The ECG revealed atrial fibrillation, which had previously been documented. An echo-Doppler study of the supra-aortic trunks (SATs) revealed non-significant stenosis. A brain MRI scan disclosed multiple ischaemic lesions at different stages. The arteriography only revealed non-specific alterations, including stenosis and irregularities in the intracavernous segment of both intracranial carotid arteries, and irregularities in both vertebral arteries. A PET/CT scan displayed increased 18F-FDG uptake along the subclavian and axillary arteries, which suggested GCA (Fig. 1). Biopsy of the temporal artery confirmed this diagnosis. The patient received corticosteroid treatment, achieving progressive improvement of symptoms.
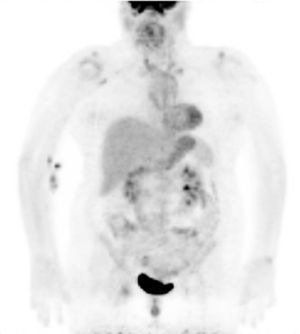
Patient 2Our second patient was a 63-year-old woman with vascular risk factors and a 2-year history of symptoms of intermittent claudication in the lower limbs. She was admitted to the neurology department due to sudden-onset right brachial monoparesis. A brain MRI scan revealed an ischaemic lesion in the left hemisphere. Six months later, she developed symptoms compatible with right-hemisphere stroke. An additional MRI scan showed acute and subacute ischaemic lesions in both hemispheres. An arteriography of the SATs and intracranial blood vessels revealed distal occlusion of the intracranial portion of the right internal carotid artery, preocclusive stenosis of the left internal carotid artery, and stenosis of the right vertebral and left subclavian arteries. The arteriography of the aorta revealed no abnormalities. A biopsy of the temporal artery showed no vasculitic changes. The 18F-FDG PET/CT study displayed diffuse hypermetabolism in the thoracic aorta, supra-aortic vessels, and abdominal aorta, which was compatible with early-stage GCA (Fig. 2). Symptoms improved with corticosteroid treatment.
The 2 cases presented here illustrate the applicability of a non-invasive technique, in this case 18F-FDG PET/CT, for diagnosing GCA, especially in patients with CNS vasculitis and exclusively neurological symptoms.
Among non-invasive techniques, echo-Doppler of the SATs may complement diagnosis of large-vessel vasculitis. Unlike 18F-FDG PET/CT, it cannot be used to assess the extent of the disease, but rather serves to examine the temporal and supra-aortic arteries exclusively.1 In any case, when the disease affects the temporal arteries exclusively, we may find positive results in echo-Doppler of the SAT and false negative results in 18F-FDG PET/CT.3
Brain MRI may show vascular alterations when structural lesions are already present; these findings are frequently non-specific. Arteriography of the SATs and intracranial blood vessels, an invasive technique, may confirm intracranial stenosis and display extracranial involvement for patients in advanced stages. However, findings of intracranial stenosis in arteriography studies may be non-specific, since features are similar in primary and secondary vasculitis of the CNA, and even in atherosclerosis.
18F-FDG PET/CT can detect areas of inflammation in the arterial wall of vessels measuring more than 5mm in diameter in early stages, even before structural changes occur. Furthermore, in the 2 cases presented here, 18F-FDG PET/CT revealed unusual findings, such as diffuse uptake along the arteries typically affected in GCA, which was helpful for differentiating atherosclerosis from arteritis.4 Likewise, this technique helps determine the spread of the disease in the affected vessels,5 an important feature for classifying vasculitis, especially when isolated CNS vasculitis is suspected.
In conclusion, 18F-FDG PET/CT has been proved useful in diagnosing large-vessel vasculitis since it enables a more thorough study of the spread and activity of the disease than do ultrasonography, MRI, or arteriography. We therefore suggest using this non-invasive technique in GCA diagnosis and follow-up, especially in initial stages or in cases with atypical manifestations such as CNS vasculitis.
FundingThis study has received no funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Mañé Martínez MA, Lopez-Cancio Martínez E, Caresia-Aróztegui AP, Vidaller Palacín A, Martínez-Yélamos S, Escudero D. Tomografía por emisión de positrones/tomografía computarizada con 18-fluorodeoxiglucosa en la evaluación de vasculitis del sistema nervioso central secundarias a arteritis de células gigantes. Neurología. 2017;32:120–122.
Partially presented in poster format at the 60th Annual Meeting of the Spanish Society of Neurology. Barcelona, November 2008.