Spontaneous acute epidural haematoma (SAEH), described by Jackson in 1869, is an infrequent condition with an estimated annual incidence of one case per million population.1 It accounts for less than 1% of all spinal space-occupying lesions, with peak incidence between the sixth and seventh decades of life.1–3 SAEH may cause rapid, irreversible neurological impairment and is associated with a mortality rate of 6% to 8%.3 These lesions are preferentially located in the cervicothoracic region, mainly in the posterior portion of the spinal canal.1 Cases where no underlying cause or predisposing factor for bleeding (blood dyscrasia, anticoagulant or antiplatelet treatment, tumours, pregnancy, or trauma) can be identified are considered spontaneous; this occurs in 40% to 50% of patients.2 Most authors suggest a haemorrhagic venous aetiopathogenic mechanism, due to the rupture of valveless epidural venous plexuses in response to a sudden pressure increase at the thoracic or abdominal level.4 However, other authors suggest bleeding is arterial in origin,5 secondary to the rupture of epidural radicular arteries, based on the rapid clinical deterioration typically associated with SAEH.6
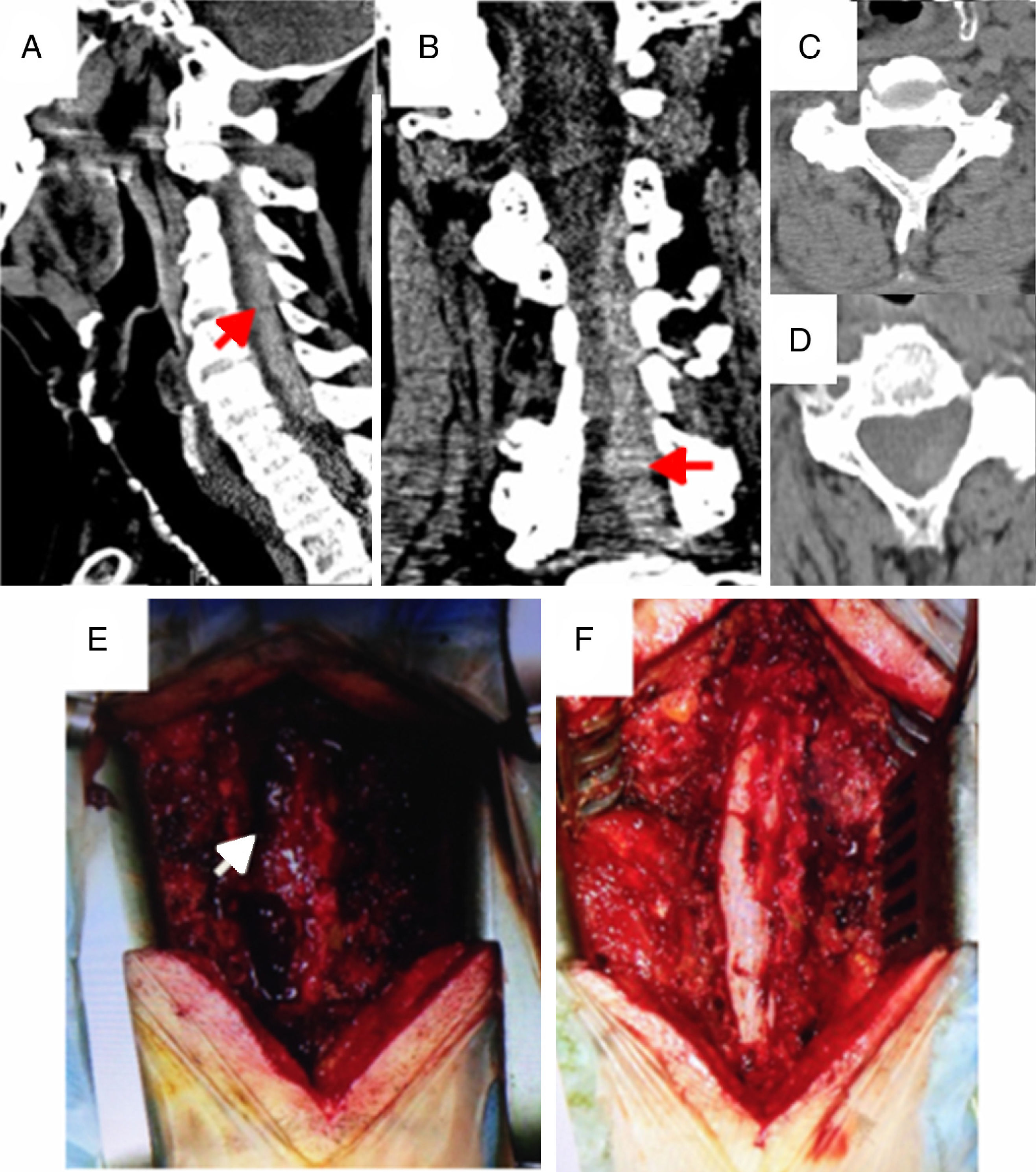
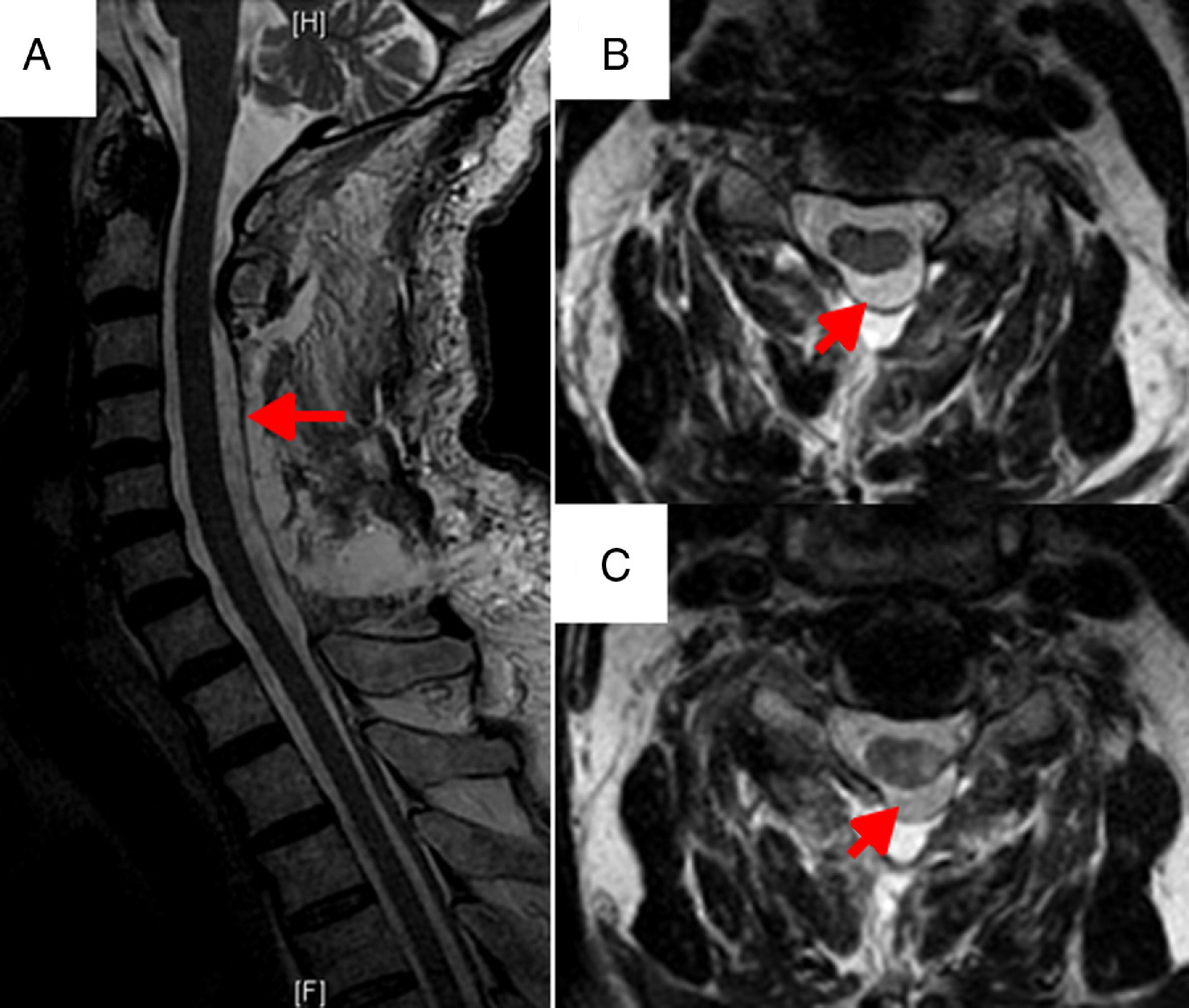
Our patient is a 79-year-old man with no relevant history who presented symptoms of intense headache and neck pain and sudden-onset left hemiparesis of 3 hours’ progression. In view of these symptoms, we activated the code stroke protocol and the patient was transferred to his reference hospital. Motor examination revealed paresis of the left arm (3/5) and left leg paralysis associated with contralateral hypaesthesia without sensory extinction, left extensor plantar reflex, and right flexor plantar reflex. An emergency brain CT scan did not show signs of intra- or extra-axial bleeding or acute brain ischaemia. Suspecting spinal involvement, we performed an emergency cervical CT scan, which showed a hyperdense epidural cervical collection located in the left posterolateral region from C3 to C7 (Fig. 1). After being diagnosed with cervical SAEH, the patient underwent an emergency C3 to C7 posterior cervical laminectomy with microsurgery; the epidural cervical collection was completely evacuated. No underlying vascular anomalies at the C3 to C7 level were identified during the procedure; the anatomical pathology study ruled out the presence of such anomalies in the surgical specimen. A cervical MRI scan performed after the surgery (Fig. 2) revealed the presence of typical postsurgical changes, absence of signs of cervical myelopathy, and small remnants of the epidural collection. The postsurgical study ruled out the presence of any clotting disorders which may have triggered the symptoms. After surgery, the patient displayed good clinical progress, recovering mobility of the left side of the body, with no residual motor or sensory deficits after completing rehabilitation.
Presurgical images from the emergency cervical CT scan. Sagittal (A), coronal (B), and axial (C and D) slices revealing the presence of an extensive hyperdense collection at the left posterolateral epidural level C3-C7 (arrows), compatible with SAEH. This collection causes a pronounced reduction of the spinal canal and displacement of the spinal cord to the right. Images after C3-C7 cervical laminectomy showing the previously described acute cervical epidural collection at the left posterolateral level (E). Image during surgery after complete evacuation of SAEH (F).
SAEH clinically manifests as acute, local, lancinating pain accompanied by motor, sensory, and/or autonomic neurological deficits, normally symmetrical, developing over a period of minutes or days.7 Unilateral symptoms are infrequent and may lead to misdiagnosis, and diagnostic and therapeutic delay. In these cases, a differential diagnosis of cerebrovascular stroke is essential,8 given the catastrophic effect of treatment with fibrinolytic agents. Acute neck pain is probably the only baseline clinical finding that may lead us to suspect spinal involvement. The distinctive feature of the case described is that the patient's condition was initially interpreted as a supratentorial ischaemic stroke.
In MRI studies, SAEH in the acute or hyperacute stage appears isointense on T1-weighted sequences and hyperintense on T2-weighted sequences.9 Although MRI is the diagnostic method of choice, spine CT is a widely available test which is fast to perform and suitable for unstable patients under invasive monitoring, and can show the location and extension of the haemorrhage. Further studies such as MR-angiography may provide relevant information on underlying lesions.10 Spinal MR-angiography is not routinely indicated; it would only be justified in those cases in which spinal MRI and/or CT findings give rise to strong suspicion of an underlying vascular lesion responsible for SAEH.11
SAEH is considered a surgical emergency and most published series recommend early surgical treatment, since surgical decompression in the first 12 to 24 hours after symptom onset is associated with better functional outcomes.2 Decompressive laminectomy and complete evacuation of the epidural collection is currently considered the surgical treatment of choice, achieving the best results.12 Conservative symptomatic treatment may be indicated in cases of incidental diagnosis, patients with minimal or no clinical signs of spinal cord compression, in patients with severe comorbidities and poor prognosis of short-term survival, or in patients with severe clotting disorders resulting in high surgical risk.2 The baseline degree of spinal involvement, as well as the time between symptom onset and surgical decompression, may be the most important prognostic factors for functional recovery.13
FundingThe authors have received no funding for this study.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Arévalo A, Navas M, Pulido P, García de Sola R. Hematoma epidural agudo cervical espontáneo de inicio atípico simulando cuadro ictal. Neurología. 2018;33:407–410.