Behavioural and psychological symptoms of dementia (BPSD), present in the vast majority of patients with Alzheimer's disease (AD), cause extensive impairment in all areas, including functionality. Early diagnosis and management are critical, especially since these symptoms are not included in the Diagnostic and Statistical Manual of Mental Disorders (DSM-V) as a diagnostic criterion of AD, but only as specific features of some patients. The main purpose of this review is to highlight the importance of these behavioural and psychological symptoms of dementia, particularly in AD. In addition, we discuss why these symptoms have not been included in the latest DSM-V.
DevelopmentWe conducted a literature search through various databases to gather data about BPSD in AD, and found a total of 12 articles.
ConclusionsBPSD are present in almost all patients and result in cognitive and functional impairment. The prevalence of these symptoms varies depending on the study and the symptom in question. In our view, BPSD should be included among the DSM diagnostic criteria for AD.
Los síntomas psicológicos y conductuales de la demencia (SPCD) están presentes en la gran mayoría de los pacientes con enfermedad de Alzheimer (EA), provocando en ellos un importante deterioro en todos los ámbitos, incluido el funcional. Por tanto, es importante su diagnóstico y manejo precoces, máxime cuando actualmente no están recogidos en la clasificación Diagnostic and Statistical Manual of Mental Disorders (DSM-V) como un criterio para el diagnóstico de esta enfermedad, sino solo como característica específica de algunos pacientes. Como objetivo principal de esta revisión, se quiere destacar la importancia de estos síntomas en las demencias, en concreto en la enfermedad de Alzheimer. Como objetivo secundario, discutir el hecho de que no hayan sido incluidos como criterio dentro de la nueva clasificación DSM-V.
DesarrolloSe realizó una búsqueda bibliográfica en distintas bases de datos sobre dichos síntomas en la enfermedad de Alzheimer, obteniendo finalmente un total de 12 artículos.
ConclusionesDestacar la importancia de estos síntomas ya que se encuentran en casi todos los pacientes, variando su prevalencia según el estudio y el síntoma estudiado; producen además una afectación de las capacidades del paciente a nivel cognitivo y funcional. También destacar la importancia de que se introduzcan como criterio diagnóstico en la clasificación DSM.
The world population is ageing rapidly, which has led to a significant increase in the incidence of Alzheimer disease (AD) and other types of dementia. This growth of the elderly population and the consequent increased incidence of age-related disorders have a considerable impact on general healthcare, and particularly on the care provided to patients with dementia. Dementia is associated not only with cognitive impairment but also with behavioural and psychological symptoms. These are defined by the 1999 Update Consensus Conference1 as “symptoms of disturbed perception, thought content, mood, or behaviour that frequently occur in patients with dementia”. Behavioural and psychological symptoms of dementia (BPSD) should be correctly assessed with a thorough, systematic neuropsychiatric battery of tests, including such tools as the Behavioural Pathology in Alzheimer's Disease Rating Scale (BEHAVE-AD)2 or the Neuropsychiatric Inventory (NPI).3 Without treatment, BPSDs can have a tremendous impact on patients, their carers, and society. These symptoms may result in earlier institutionalisation,4–8 higher economic costs,9,10 poorer quality of life of both patients and carers,11–13 increased caregiver and nursing staff burden,14,15 and increased disability.16,17 Patients with BPSDs have higher levels of disability; however, when these symptoms improve or resolve, their functional capacity also increases, improving their quality of life.
Psychological symptoms include delusions (prevalence ranges from 10% to 73%; delusion of persecution is the most common),5 hallucinations (12%-49%; visual hallucinations are the most common), misidentifications (affecting 16% of patients with AD),18 depression (diagnosis is very difficult in patients with dementia), apathy (one of the most common symptoms, with over 50% patients affected), and anxiety. Behavioural symptoms include walkabout (one of the most problematic), agitation/aggression, resistance to care, inappropriate sexual behaviour, and catastrophic reactions (anger, verbal and physical aggression). Although each type of dementia has different behavioural and psychological symptoms, patients may also display symptoms that are not typical of the type of dementia that they have.
Dementia in general, and AD in particular, is associated with other relevant behavioural comorbidities, such as obsessive-compulsive disorder and sleep or eating disorders; these disorders should be identified and treated since they contribute to poorer quality of life.
BPSDs should be recognised as a part of dementia; for many years, however, they have been disregarded by the traditional mental disorder classification systems (more specifically, classification systems for dementia syndromes). This is striking, considering the high prevalence of BPSDs in these patients and the resulting high levels of disability and dependence. The first editions of the Diagnostic and Statistical Manual of Mental Disorders (DSM) describe the cognitive symptoms of dementia but do not mention behavioural problems. The NINCDS-ADRDA criteria for the clinical diagnosis of AD, published in 1984,19 list several associated behavioural symptoms (depression, insomnia, delusions, etc.). The DSM-IV,20 and subsequently the DSM-IV-TR,21 do include these criteria. The DSM-IV-TR focuses on describing the clinical characteristics of dementia (alterations in perception, mood, etc.). When the DSM-IV-TR was under revision, some experts recommended that dementia should include multiple descriptive categories for BPSDs. However, the DSM-V22 only included the phrase “with behavioural disturbance” to identify patients requiring special management. The DSM-V also uses a different terminology, replacing ‘dementia’ with ‘major neurocognitive disorder’ and ‘mild cognitive impairment’ with ‘mild neurocognitive disorder’. In summary, although BPSDs have been described for over a century, there is still no consensus on how they should be quantified or classified.
The main purpose of this review is to highlight the importance of these symptoms in patients with dementia, and specifically with AD. As a secondary objective, we reflect on the fact that BPSDs were not included as a diagnostic criterion in the DSM-V.
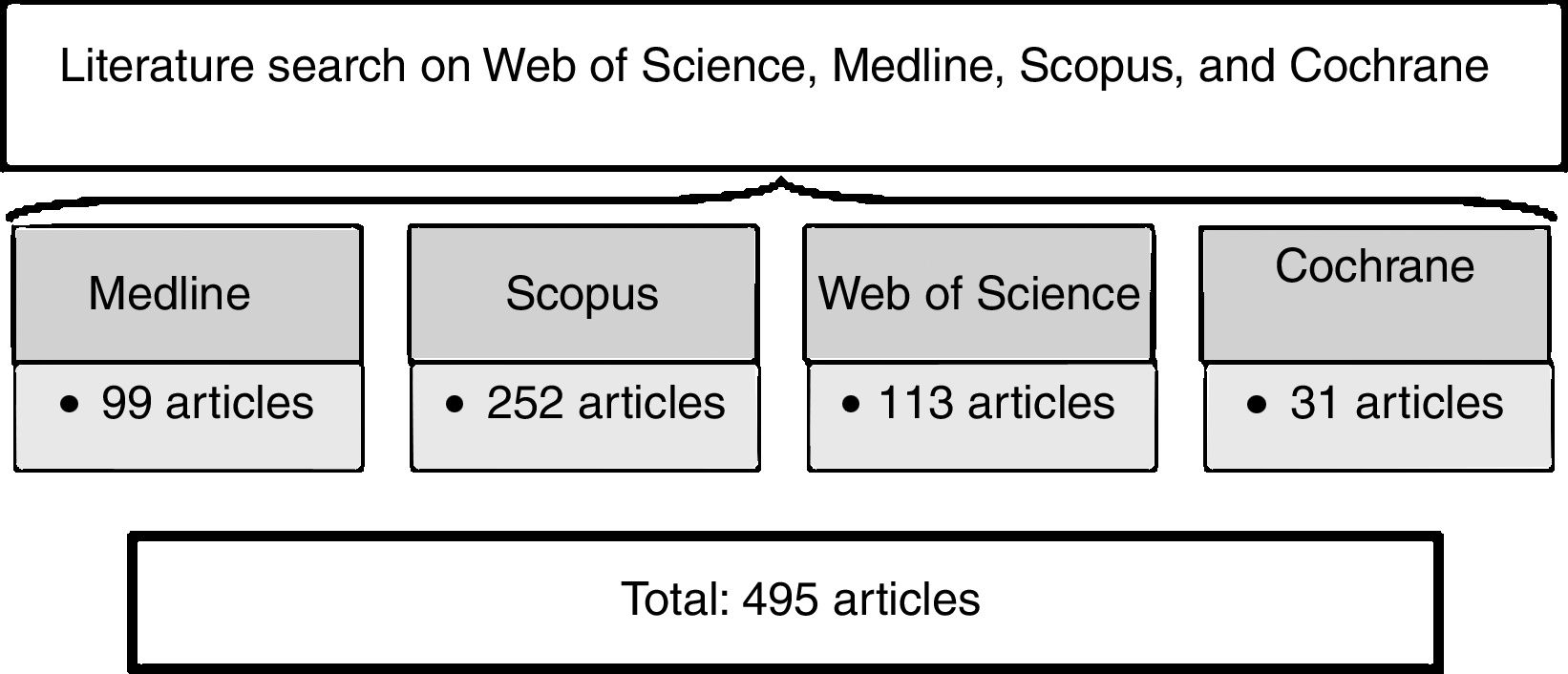
Material and methodsWe conducted a literature search on the Web of Science, Medline/PubMed, Scopus, and Cochrane databases using the keywords ‘Alzheimer disease’ and ‘behavioural and psychological symptoms’ to gather articles published in the past 5 years (2010-2015). We used the following search strategy on Web of Science: (“Alzheimer disease” AND “behavioural and psychological symptoms”, publication years: 2010-2015); the search returned 113 articles. On Medline, we used ([“alzheimer disease” AND “behavioural and psychological symptoms”]) AND (“2010” [Date - Publication]: “2015”[Date - Publication]); our search yielded 99 articles. We gathered 252 articles from Scopus using the following search strategy: (“Alzheimer disease” AND “behavioural and psychological symptoms”) AND Pubyear > 2009 AND Pubyear < 2016. It is not possible to limit the timeframe for publication of Cochrane reviews. We gathered 31 of these articles with the following search strategy: (“alzheimer disease” AND “behavioural and psychological symptoms”). We gathered a total of 495 scientific articles on AD and BPSDs (Fig. 1).
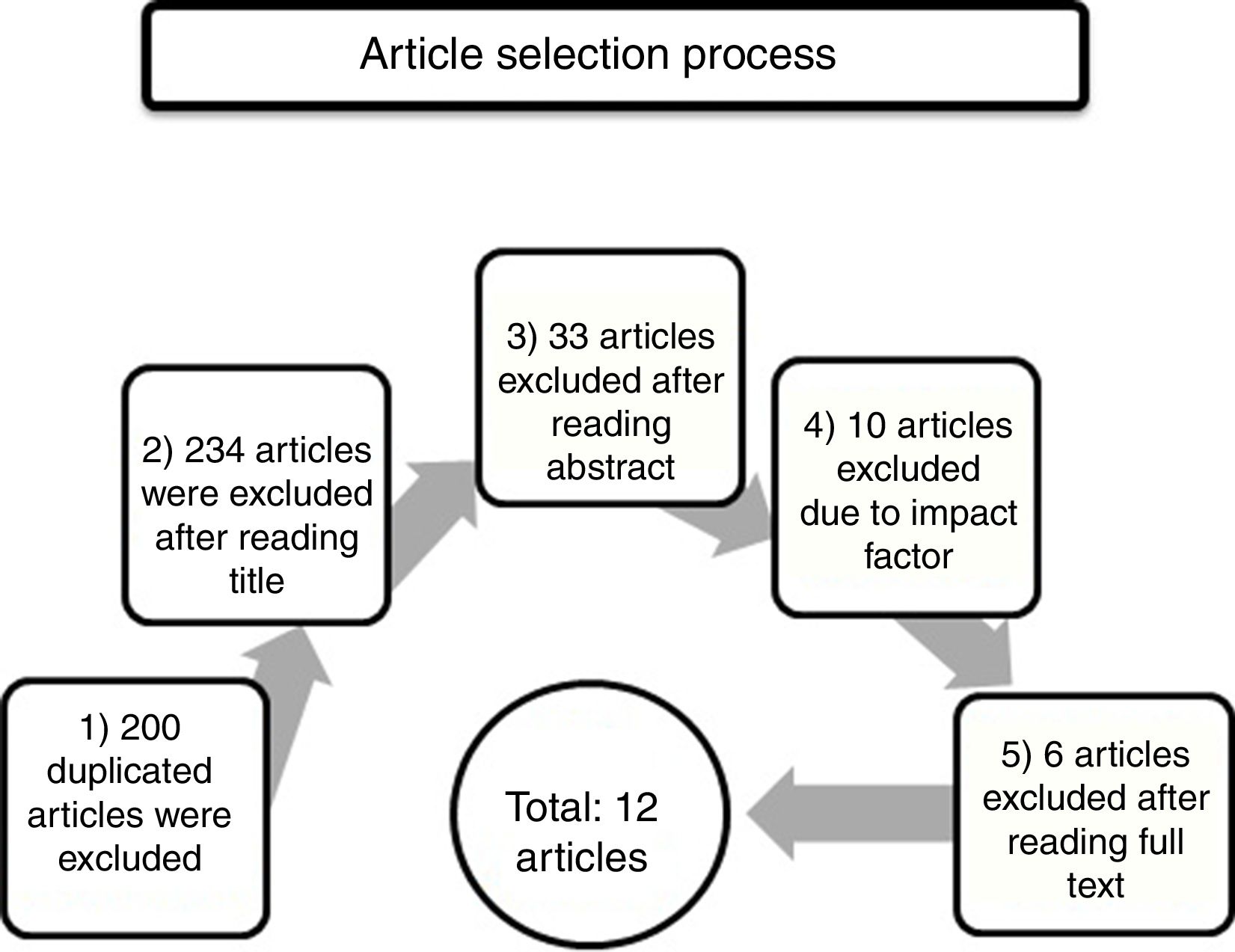
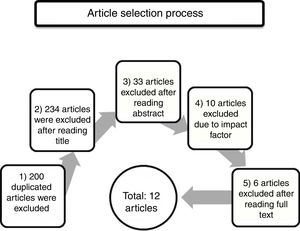
We selected articles addressing BPSDs in patients with AD and excluded those addressing other types of dementia, treatment, or disorders affecting carers (Fig. 2). The article selection process was as follows: 1) A total of 200 duplicate articles were excluded. 2) We then read all article titles and excluded those articles whose topic was unrelated to the subject of our review, those addressing BPSD treatment or pathophysiology, those addressing other types of dementia or dementia in general, and those addressing carers and their diseases; a total of 234 articles were excluded in this stage. 3) We subsequently read the abstracts and excluded an additional 33 articles on the treatment, pathophysiology, and genetics of BPSDs. We also excluded one article on depression. 4) The Journal Citation Report electronic resource was used to exclude articles published in journals with no impact factor. We also excluded those articles published in journals from such countries or regions as China (2), India (1), Thailand (1), Africa (1), and Korea (1). In this step we excluded 10 articles in total. 5) Finally, we read the full texts of the remaining articles and excluded those addressing the costs or treatment of BPSDs, and those comparing BPSDs between different types of dementia (vascular dementia, frontotemporal dementia, etc.). Our literature review finally included a total of 12 articles.
ResultsOf the 12 articles included in the review,18,23–33 9 were studies on AD18,23–30 (some also included patients with other types of dementia) and the remaining 3 were literature reviews.31–33
Spalletta et al.23 included 1015 patients newly diagnosed with AD (according to the NINCDS-ADRDA criteria) and receiving no treatment. Their purpose was to determine which BPSDs appear in these patients (using the NPI), and to describe their frequency and severity and the association between presence of these symptoms and dementia severity according to the Mini–Mental State Examination (MMSE).34 One or more symptoms were recorded in 77.8% of patients, with apathy being the most frequent symptom. All BPSDs increased with severity of cognitive impairment, with the exception of affective symptoms. The researchers conclude that psychiatric assessment of patients with AD is necessary in order to detect any BPSDs and to design an appropriate care plan.
Fernández et al.24 studied BPSDs and their association with cognitive impairment in 1014 patients diagnosed with AD (DSM-IV criteria). The severity of dementia was measured with the MMSE; BPSDs were assessed using the Spanish-language version of the non-cognitive section of the Alzheimer's Disease Assessment Scale (ADAS-Non-Cog).35,36 Psychotic symptoms were more prevalent among patients with high ADAS-Non-Cog scores (26-50), whereas emotional symptoms were more frequent in those with lower scores (≤25). The prevalence of apathy is similar to those reported in previous studies. The results of this study confirm the high prevalence of non-cognitive symptoms in patients with AD, and suggest that cognitive impairment is associated with presence of BPSDs in patients with high ADAS-Non-Cog scores: the number of BPSDs increases with severity of cognitive impairment.
Garre-Olmo et al.25 studied 491 patients with a diagnosis of AD according to the NINCDS-ADRDA criteria. Based on their BPSD, patients were classified into 3 categories: psychotic syndrome, affective syndrome, and behavioural syndrome. The frequency of psychotic and behavioural syndromes was found to increase over time (from 18.3% to 25.7%, and from 63.3% to 71.8%, respectively), whereas no changes were seen in the incidence of affective syndrome. Behavioural syndrome was the most frequent. Psychotic syndrome was most frequent in patients with moderate AD. The incidence of affective syndrome was low in patients with mild and advanced AD, increasing in patients with moderate AD.
Palmer et al.26 studied 177 patients with AD (DSM-IV and NINCDS-ADRDA criteria) to determine whether neuropsychiatric alterations predict functional impairment (assessed with the Katz Index of Independence in Activities of Daily Living [Katz ADL],37 which defines functional impairment as inability to perform one or more activities of daily living) and cognitive decline (assessed with the MMSE, with a decrease of at least 5 points indicating cognitive impairment). The researchers described 5 syndromes: psychotic, psychomotor, affective, manic, and apathy; apathy was the most frequent. They concluded that certain neuropsychiatric syndromes play an important role in AD progression, predicting functional and cognitive impairment, and may be useful for long-term planning of care and treatment of patients with AD.
Bettney et al.27 studied 84 patients with dementia (51 with AD according to the NINCDS-ADRDA criteria and 33 with vascular dementia) to determine which neuropsychiatric syndromes (psychosis, hyperactivity, apathy, affective disorder) were stable throughout the progression of the disease. In their sample, these symptoms remained relatively stable throughout the 2-year study period.
Pocnet et al.28 studied the association between BPSDs and personality traits of AD in 54 patients with early-stage AD (ICD-10 and NINCDS-ADRDA criteria) and 64 controls. BPSDs were more prevalent in patients with AD than in controls, with apathy being the most frequent symptom. The researchers found no association between premorbid personality traits and BPSDs in early stages of AD, although they could not rule out a more complex relationship. In any case, as personality and behavioural changes occur in early stages of AD, they may help in early detection of the disease.
Poletti et al.29 evaluated 166 patients with dementia, 157 of whom had BPSDs and were therefore included in the final sample. Of these, 140 had AD (NINCDS-ADRDA criteria) and the remaining 17 had frontotemporal or vascular dementia. Depression was the most frequent symptom in their sample, with irritability also being very prevalent among the subset of patients with AD. The researchers aimed to determine whether BPSDs may serve as predictors of cognitive impairment and found a statistically significant association (P=.001) between cognitive impairment and 2 other symptoms (apathy and motor disturbance), both in the whole sample of patients with BPSD and in the subset of patients with AD. However, they could not definitively state that BPSDs were the only factors leading to cognitive impairment; rather, multiple factors have been suggested to promote cognitive impairment and BPSDs (the environment, a history of psychiatric disorders, genetic factors, etc.).
Tran et al.18 studied the impact of psychotic symptoms on functional independence in 234 patients diagnosed with AD according to the NINCDS-ADRDA criteria. In their sample, 35% of patients had psychotic symptoms, with the delusions “someone is in my house” and “someone is stealing from me” being the most frequent. The researchers concluded that patients with many psychotic symptoms may be less autonomous in activities of daily living (assessed with the Katz ADL index) and that these symptoms have no impact on instrumental activities (assessed with the scale designed by Lawton and Brody38).
Bidzan et al.30 studied BPSDs in early-stage AD and vascular dementia. They gathered 291 residents of nursing homes in Gdynia (Poland) who did not meet the DSM-IV criteria for dementia at the beginning of the study. The final analysis included 150 patients, of whom 111 were not diagnosed with dementia (controls), 14 were diagnosed with vascular dementia, and 25 with AD (NINCDS-ADRDA criteria). BPSDs were evaluated with the nursing home version of the NPI (NPI-NH).39 The researchers found a high rate of BPSDs in preclinical stages of AD and vascular dementia. Aggressive behaviour was more frequent in patients with AD. The authors concluded that BPSDs were more likely to be observed closer to the time of diagnosis of dementia, especially AD.
Of the 3 review articles included in our study, 2 address BPSDs generally31,32 and one focuses on apathy specifically.33 According to the García-Alberca et al.31 review, prevalence of BPSDs varies between studies, with apathy being the most common symptom. The researchers also address the association between BPSDs and the stage of AD, and suggest using BPSDs as a marker of advanced AD, based on the results of the study by Fernández et al.24 Milano et al.32 classify BPSDs into 5 categories: apathy, depression, psychosis, agitation, and aggression. They state that depression is a risk factor for AD and suggest that presence of BPSDs may be a cause of diagnostic error, as early-stage AD may be misdiagnosed as other psychiatric disorders. According to the review by Cipriani et al.,33 most patients with AD experience BPSDs, with apathy being a common symptom in these patients (19%-92%). The researchers call attention to the fact that apathy is underrecognised despite its high incidence in patients with AD and its considerable impact on patients’ functional ability and caregiver burden and stress.
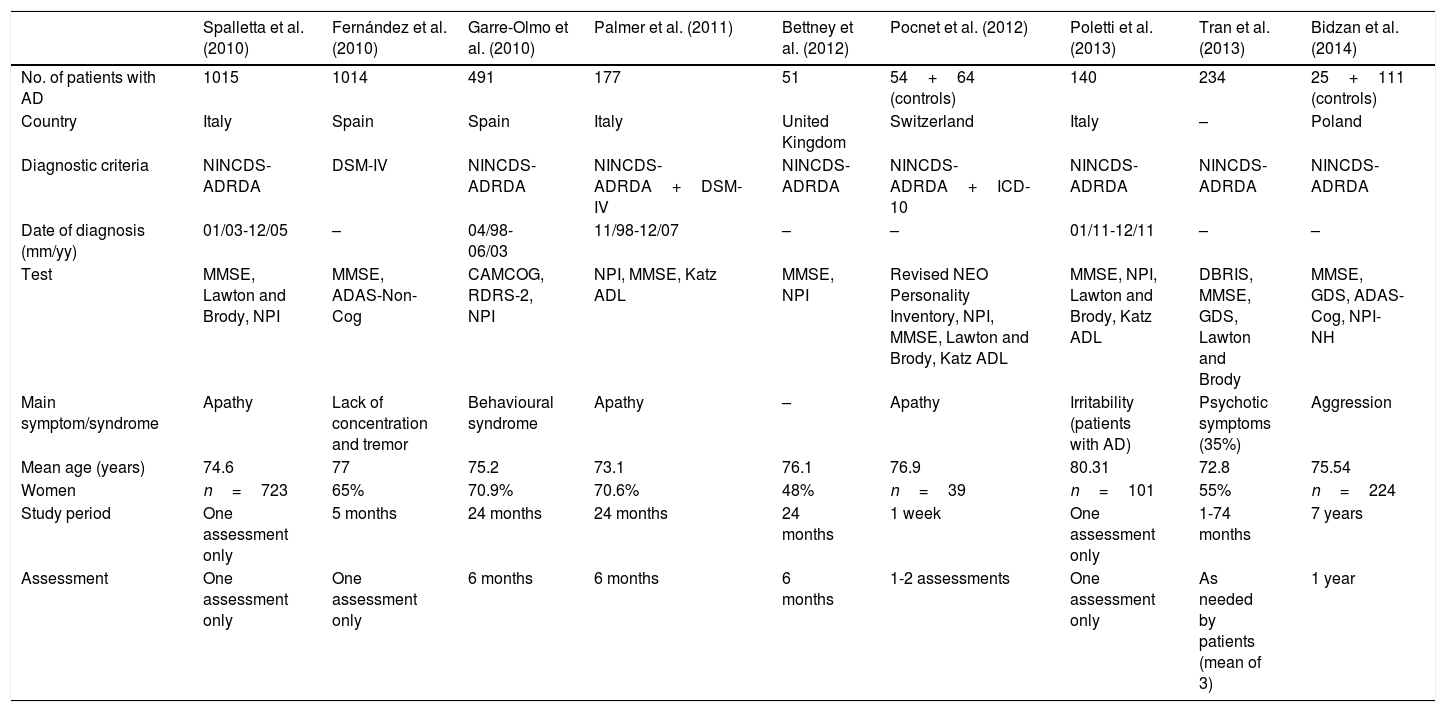
The main symptom or syndrome studied in each article varies (Table 1). Apathy is reported in 3 of the 9 articles23,26,28 and in 2 of the 3 reviews.32,33 The study by Tran et al.18 addresses psychotic symptoms only. The NINCDS-ADRDA diagnostic criteria, more specific for diagnosing AD, were used in all studies except for the study by Fernández et al.,24 who used the DSM-IV criteria. Palmer et al.26 used both diagnostic classifications. Regarding the assessment of BPSDs, most studies used the NPI (Bidzan et al.30 used the nursing home version of this index).
Comparative study of the 9 studies including patients with AD.
| Spalletta et al. (2010) | Fernández et al. (2010) | Garre-Olmo et al. (2010) | Palmer et al. (2011) | Bettney et al. (2012) | Pocnet et al. (2012) | Poletti et al. (2013) | Tran et al. (2013) | Bidzan et al. (2014) | |
|---|---|---|---|---|---|---|---|---|---|
| No. of patients with AD | 1015 | 1014 | 491 | 177 | 51 | 54+64 (controls) | 140 | 234 | 25+111 (controls) |
| Country | Italy | Spain | Spain | Italy | United Kingdom | Switzerland | Italy | – | Poland |
| Diagnostic criteria | NINCDS-ADRDA | DSM-IV | NINCDS-ADRDA | NINCDS-ADRDA+DSM-IV | NINCDS-ADRDA | NINCDS-ADRDA+ICD-10 | NINCDS-ADRDA | NINCDS-ADRDA | NINCDS-ADRDA |
| Date of diagnosis (mm/yy) | 01/03-12/05 | – | 04/98-06/03 | 11/98-12/07 | – | – | 01/11-12/11 | – | – |
| Test | MMSE, Lawton and Brody, NPI | MMSE, ADAS-Non-Cog | CAMCOG, RDRS-2, NPI | NPI, MMSE, Katz ADL | MMSE, NPI | Revised NEO Personality Inventory, NPI, MMSE, Lawton and Brody, Katz ADL | MMSE, NPI, Lawton and Brody, Katz ADL | DBRIS, MMSE, GDS, Lawton and Brody | MMSE, GDS, ADAS-Cog, NPI-NH |
| Main symptom/syndrome | Apathy | Lack of concentration and tremor | Behavioural syndrome | Apathy | – | Apathy | Irritability (patients with AD) | Psychotic symptoms (35%) | Aggression |
| Mean age (years) | 74.6 | 77 | 75.2 | 73.1 | 76.1 | 76.9 | 80.31 | 72.8 | 75.54 |
| Women | n=723 | 65% | 70.9% | 70.6% | 48% | n=39 | n=101 | 55% | n=224 |
| Study period | One assessment only | 5 months | 24 months | 24 months | 24 months | 1 week | One assessment only | 1-74 months | 7 years |
| Assessment | One assessment only | One assessment only | 6 months | 6 months | 6 months | 1-2 assessments | One assessment only | As needed by patients (mean of 3) | 1 year |
AD: Alzheimer disease; BPSD: behavioural and psychological symptoms of dementia.
Source: A. Pérez Romero.
All the articles included in our review report high incidence of BPSDs, confirming the significant importance of these symptoms in patients with AD. Our results also show that the NPI is the main diagnostic tool used for BPSDs. Apathy appears to be one of the most prevalent symptoms.
According to some studies, BPSD incidence increases due to more severe cognitive impairment.23,24 Other studies suggest the opposite: higher incidence of BPSDs leads to more severe cognitive impairment. We should point out, however, that cognitive impairment severity is influenced by a wide range of factors, and not only by these symptoms.29
Several articles agree that BPSDs may be used as predictors of dementia,26,28,30,31 or AD in this case, since they play an important role in disease progression; it has been suggested that these symptoms are markers of cognitive31 or functional26 impairment, appear in the form of personality changes,28 and may point to early-stage dementia.30 Diagnostic errors may occur when BPSDs appear at very early stages of dementia, as these symptoms may be misdiagnosed for other psychiatric disorders.32
DiscussionThis review underscores the importance of BPSDs in dementia, and more specifically in AD. A large majority of patients will experience these symptoms at some point during disease progression. BPSDs have a negative impact on patients’ quality of life and well-being. Early diagnosis of these symptoms is essential to preventing adverse effects, providing early treatment (pharmacological or otherwise), and designing the most suitable care plan for these patients.
It is difficult to compare the results of the studies included in our review since they use different tools and classification systems for cognitive impairment and BPSDs.
Presence of BPSDs should be regarded as a diagnostic criterion of AD. Although the DSM classification does mention these symptoms, it includes them as specifiers rather than listing them among the diagnostic criteria.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Pérez Romero A, González Garrido S. La importancia de los síntomas psicológicos y conductuales (SPCD) en la enfermedad de Alzheimer. Neurología. 2018;33:378–384.