We aimed to determine whether the aetiology of ischaemic stroke has changed in recent years and, if so, to ascertain the possible reasons for these changes.
Patients and methodsWe analysed the epidemiological history and vascular risk factors of all patients diagnosed with ischaemic stroke at Complejo Hospitalario Universitario de Albacete (CHUA) from 2009 to 2014. Ischaemic stroke subtypes were established using the TOAST criteria. Our results were compared to data from the classic Stroke Data Bank (SDB); in addition, both series were compared to those of other hospital databases covering the period between the two.
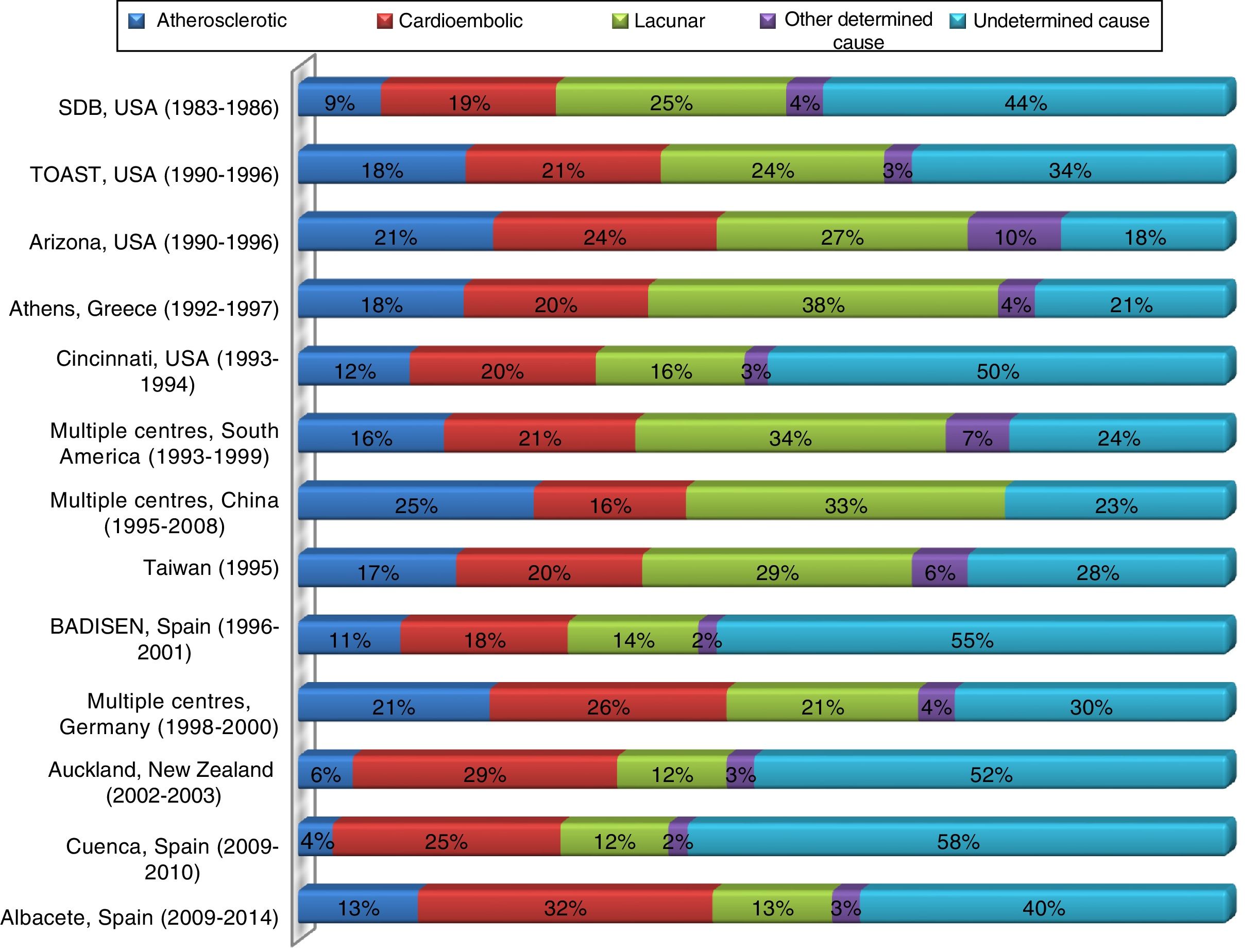
ResultsWe analysed 1664 patients (58% were men) with a mean age of 74 years. Stroke aetiology in both series (CHUA, SDB) was as follows: atherosclerosis (12%, 9%), small-vessel occlusion (13%, 25%), cardioembolism (32%, 19%), stroke of other determined aetiology (3%, 4%), and stroke of undetermined aetiology (40%, 44%). Sixty-three percent of the patients from the CHUA and 42% of the patients from the SDB were older than 70 years. Cardioembolic strokes were more prevalent in patients older than 70 years in both series. Untreated hypertension was more frequent in the SDB (SDB=31% vs CHUA=10%). The analysis of other databases shows that the prevalence of cardioembolic stroke is increasing worldwide.
ConclusionsOur data show that the prevalence of lacunar strokes is decreasing worldwide whereas cardioembolic strokes are increasingly more frequent in both our hospital and other series compared to the SDB. These differences may be explained by population ageing and the improvements in management of hypertension and detection of cardioembolic arrhythmias in stroke units.
Comprobar si han existido variaciones en la etiología del ictus isquémico en los últimos años e investigar las posibles causas que lo justifiquen.
Pacientes y métodosAnálisis de los antecedentes epidemiológicos y factores de riesgo vascular de los pacientes diagnosticados de ictus isquémico en el Complejo Hospitalario Universitario de Albacete (CHUA) entre 2009 y 2014. La clasificación etiológica del ictus isquémico se realizó según los criterios TOAST. Se compararon los resultados con los de la clásica Stroke Data Bank (SDB) y se contrastaron ambas series con otros registros hospitalarios publicados en el periodo que las separa.
ResultadosSe analiza a 1.664 pacientes, 58% varones, mediana de edad 74 años. Según la clasificación etiológica los resultados obtenidos son (CHUA/SDB): aterotrombóticos (12%/9%), lacunares (13%/25%), cardioembólicos (32%/19%), causa infrecuente (3%/4%) e indeterminados (40%/44%). El 63% de los pacientes del CHUA era mayor de 70 años, en la SDB solo el 42% superaba esa edad. En ambos registros el subtipo cardioembólico era más prevalente en mayores de 70 años. La HTA no tratada era más frecuente en la SDB (SDB=31% vs. CHUA=10%). El análisis de otras bases de datos muestra una tendencia progresiva a escala mundial al aumento en la prevalencia del ictus cardioembólico.
ConclusionesNuestro estudio muestra tanto en nuestro centro como a escala mundial una disminución del porcentaje de ictus lacunares y un aumento del de cardioembólicos respecto a la SDB. Estas diferencias pudieran justificarse por el envejecimiento de los pacientes, el mejor control de la HTA actualmente y mayor capacidad para detectar arritmias cardioembólicas en las Unidades de Ictus.
Stroke and associated complications account for approximately 10% of mortality worldwide, making the disease the second leading cause of death and the third leading cause of disability in terms of years of potential life lost.1–3 In Spain, stroke is associated with a mortality rate of 11%, making it the second leading cause of death in the general population and the leading cause of death among women.4 Incidence of stroke in Spain is estimated at approximately 128 cases per 100000 person-years4; this figure rises exponentially in people above the age of 65.
In the light of the above information, it is necessary to create effective, targeted stroke prevention strategies5 and to improve acute-phase care,6 as well as promoting therapies and neurorepair and rehabilitation programmes to minimise sequelae in the post-acute phase.7 Better overall understanding of stroke compels us also to study the epidemiological characteristics of the disease, including a detailed analysis of the various aetiologies and associated risk factors. Stroke databases constitute an invaluable tool in this line of research.8,9 The Stroke Data Bank (SDB), an American project, is without a doubt one of the most historically important examples.10 The database was launched in 1983 by the National Institute of Neurological and Communicative Disorders and Stroke, which gathered prospective data on patients with stroke admitted to 4 US hospitals over a 3-year period. The registry was the first to classify ischaemic stroke according to aetiology (large-artery atherosclerosis; cardioembolism; small-vessel occlusion; stroke of other determined aetiology; and stroke of undetermined aetiology). These categories were restructured and published several years later by the Trial of ORG 10172 in Acute Stroke Treatment (TOAST) study group,11 and continue to be one of the most widely used classifications in the study of stroke epidemiology.12 The TOAST classification has long been used at our centre and by the Spanish Society of Neurology's BADISEN stroke bank project from its conception. After comparing early BADISEN data13 with recent data obtained in our department, and conducting an exploratory analysis of published SDB data, we developed the theory that a change may have taken place in recent years in the aetiological epidemiology of ischaemic stroke. To test this hypothesis and investigate the potential causes of this shift, we analysed aetiological data from patients attending our centre over the last 6 years, comparing these against the data obtained approximately 30 years ago in the SDB project. We also compared the results of both series against other hospital databases published in the intervening period.
Material and methodsWe performed a prospective, observational, single-centre study, analysing data from the Complejo Hospitalario Universitario de Albacete (CHUA) stroke database from August 2009 (the time of its creation) to April 2014. The database was created at the same time as the hospital's stroke unit, and systemically gathers data on all patients referred to the unit from the hospital's emergency department. This study includes patients with ischaemic stroke and transient ischaemic attacks and excludes patients with haemorrhagic stroke. All patients underwent an assessment protocol including a complete blood study, chest radiography, ECG monitoring of at least 24hours’ duration, transcranial and supra-aortic trunk ultrasound, and at least one brain imaging study (CT and/or MRI). According to clinical suspicion, further testing included echocardiography, a thrombophilia study of the peripheral blood, CT or MRI angiography, and arteriography studies of the large vessels and circle of Willis. Ischaemic stroke was classified according to the TOAST criteria.11 We also analysed data on such other variables as sex, age, and vascular risk factors (VRF). Patients are included in the database when they are admitted to the unit for the first time, not taking into account whether the stroke was the first they had experienced or a recurrence, with the first stroke having been treated elsewhere; this variable was not systematically recorded. No patient appears more than once in the database (we did not include recurrences in patients who had previously been treated for stroke at our centre). We compared our results with those of the SDB study.10 A review was also carried out of other hospital databases, compiled in the period since the SDB was published, using the TOAST classification; we selected 11 such studies which we considered to be representative of the global distribution of stroke. Specifically, we selected 3 studies from the USA,14–16 one multinational review from South America,17 2 studies from Asia,18,19 4 from Europe,20–23 and one from New Zealand.24 No African studies were included as no registry from the region included data on the results of at least one neuroimaging study for all patients.
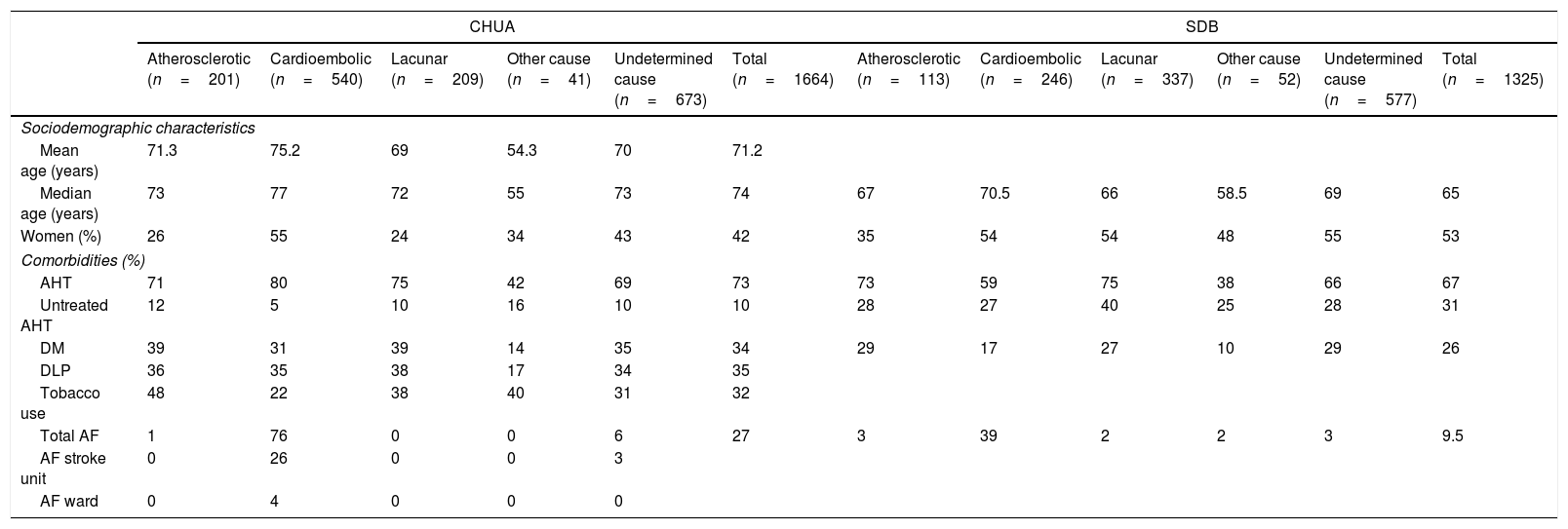
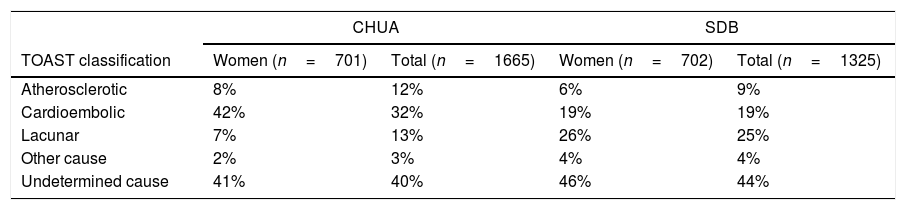
ResultsWe analysed data from a total of 1664 patients attending the CHUA stroke unit with ischaemic stroke or transient ischaemic attack; mean age was 71.2±12 years and median age was 74 (Table 1). Mean ECG monitoring duration was 2.5 days. Aetiology was atherosclerosis in 12% of cases, cardioembolism in 32%, lacunar stroke in 13%, other determined aetiology in 3%, and undetermined in 40% of cases (Table 2).
Social and demographic characteristics and comorbidities by stroke subtype in the CHUA and SDB databases.
| CHUA | SDB | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Atherosclerotic (n=201) | Cardioembolic (n=540) | Lacunar (n=209) | Other cause (n=41) | Undetermined cause (n=673) | Total (n=1664) | Atherosclerotic (n=113) | Cardioembolic (n=246) | Lacunar (n=337) | Other cause (n=52) | Undetermined cause (n=577) | Total (n=1325) | |
| Sociodemographic characteristics | ||||||||||||
| Mean age (years) | 71.3 | 75.2 | 69 | 54.3 | 70 | 71.2 | ||||||
| Median age (years) | 73 | 77 | 72 | 55 | 73 | 74 | 67 | 70.5 | 66 | 58.5 | 69 | 65 |
| Women (%) | 26 | 55 | 24 | 34 | 43 | 42 | 35 | 54 | 54 | 48 | 55 | 53 |
| Comorbidities (%) | ||||||||||||
| AHT | 71 | 80 | 75 | 42 | 69 | 73 | 73 | 59 | 75 | 38 | 66 | 67 |
| Untreated AHT | 12 | 5 | 10 | 16 | 10 | 10 | 28 | 27 | 40 | 25 | 28 | 31 |
| DM | 39 | 31 | 39 | 14 | 35 | 34 | 29 | 17 | 27 | 10 | 29 | 26 |
| DLP | 36 | 35 | 38 | 17 | 34 | 35 | ||||||
| Tobacco use | 48 | 22 | 38 | 40 | 31 | 32 | ||||||
| Total AF | 1 | 76 | 0 | 0 | 6 | 27 | 3 | 39 | 2 | 2 | 3 | 9.5 |
| AF stroke unit | 0 | 26 | 0 | 0 | 3 | |||||||
| AF ward | 0 | 4 | 0 | 0 | 0 | |||||||
AF: atrial fibrillation; AF stroke unit: atrial fibrillation diagnosed at the stroke unit; AF ward: atrial fibrillation diagnosed in inpatients wards; AHT: arterial hypertension; CHUA: Complejo Hospitalario Universitario de Albacete; DLP: dyslipidaemia; DM: diabetes mellitus; SDB: Stroke Data Bank.
TOAST ischaemic stroke subtypes in the CHUA and SDB databases, by sex.
| CHUA | SDB | |||
|---|---|---|---|---|
| TOAST classification | Women (n=701) | Total (n=1665) | Women (n=702) | Total (n=1325) |
| Atherosclerotic | 8% | 12% | 6% | 9% |
| Cardioembolic | 42% | 32% | 19% | 19% |
| Lacunar | 7% | 13% | 26% | 25% |
| Other cause | 2% | 3% | 4% | 4% |
| Undetermined cause | 41% | 40% | 46% | 44% |
CHUA: Complejo Hospitalario Universitario de Albacete; SBD: Stroke Data Bank.
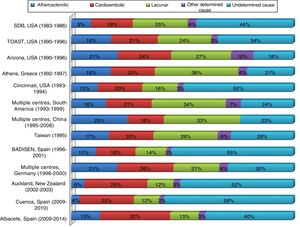
Fig. 1 lists the stroke databases selected. All databases are based on hospital registries using the TOAST classification, and were compiled in different countries and years. We studied a total of 13 registries, including the SDB and CHUA databases in addition to the 11 databases mentioned previously. Generally, the more recent studies show a larger percentage of cardioembolic stroke and a smaller percentage of lacunar stroke than older studies.
Hospital stroke registries. Distribution of TOAST subtypes of ischaemic stroke in Albacete and in other hospital registries.
Sources: Foulkes et al.,10 Adams et al.,14 Frey et al.,15 Vemmos et al.,20 Schneider et al.,16 Saposnik et al.,17 Tsai et al.,18 Yip et al.,19 Morín-Martín et al.,21 Grau et al.,22 Feigin et al.,24 and Carod-Artal et al.23
Stroke was more frequent in male patients at our hospital, whereas in the SBD, women accounted for 53% of patients (Table 1). However, cardioembolic stroke was more frequent in women in both databases (55% in the CHUA registry and 54% in the SDB); in the CHUA database, all other subtypes, and particularly atherosclerosis and lacunar stroke, were more frequent in men.
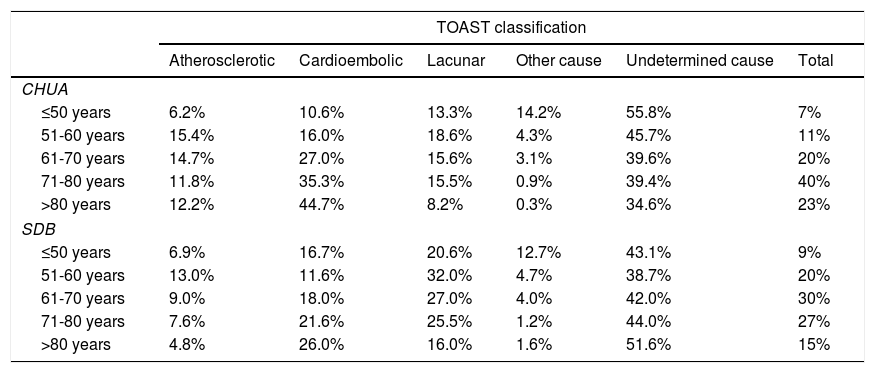
Table 3 shows the distribution of stroke by age group. Sixty-three percent of patients in our sample were older than 70; the age group most frequently affected by stroke was 71-80 years (40% of cases). In the SDB, on the other hand, patients aged above 70 accounted for just 42% of cases. In both databases, lacunar stroke and other determined aetiology were more common in younger age groups. However, the prevalence of cardioembolic stroke increases in line with age group in both populations. This is the most frequent aetiology in patients aged over 80 in our sample (44.7% of cases), and is responsible for more cases than undetermined aetiology.
Age distribution of patients by stroke subtype.
| TOAST classification | ||||||
|---|---|---|---|---|---|---|
| Atherosclerotic | Cardioembolic | Lacunar | Other cause | Undetermined cause | Total | |
| CHUA | ||||||
| ≤50 years | 6.2% | 10.6% | 13.3% | 14.2% | 55.8% | 7% |
| 51-60 years | 15.4% | 16.0% | 18.6% | 4.3% | 45.7% | 11% |
| 61-70 years | 14.7% | 27.0% | 15.6% | 3.1% | 39.6% | 20% |
| 71-80 years | 11.8% | 35.3% | 15.5% | 0.9% | 39.4% | 40% |
| >80 years | 12.2% | 44.7% | 8.2% | 0.3% | 34.6% | 23% |
| SDB | ||||||
| ≤50 years | 6.9% | 16.7% | 20.6% | 12.7% | 43.1% | 9% |
| 51-60 years | 13.0% | 11.6% | 32.0% | 4.7% | 38.7% | 20% |
| 61-70 years | 9.0% | 18.0% | 27.0% | 4.0% | 42.0% | 30% |
| 71-80 years | 7.6% | 21.6% | 25.5% | 1.2% | 44.0% | 27% |
| >80 years | 4.8% | 26.0% | 16.0% | 1.6% | 51.6% | 15% |
CHUA: Complejo Hospitalario Universitario de Albacete; SDB: Stroke Data Bank.
The most frequent VRF in both studies was arterial hypertension (AHT); AHT was present in 73% of patients in the CHUA sample (Table 1). No major differences were observed between the 2 samples in terms of the distribution of the classic VRFs in the different aetiological subgroups, with the exception of cardioembolic stroke: 59% of SDB patients had AHT vs 80% of CHUA patients. In the CHUA registry, patients with cardioembolic stroke showed the highest rate of AHT. We observed a considerable difference between the 2 databases in the percentage of patients with AHT not receiving antihypertensives (31% in the SDB and <10% in the CHUA registry; Table 1). The aetiology showing the greatest difference for this variable was lacunar stroke: 40% of patients with AHT and lacunar stroke in the SDB were not being treated.
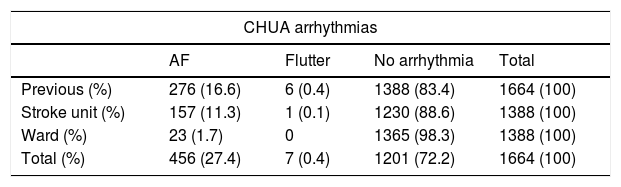
The most frequent cause of cardioembolic stroke in our sample was atrial fibrillation (AF); AF was responsible for 76% of these cases in our sample vs 39% in the SDB (Table 1). As shown in Table 4, of all cases of AF observed at our centre (n=456), over half were known prior to stroke occurrence or diagnosed upon the patient's arrival at the hospital's emergency department (n=276). One-third of arrhythmias (n=157) were detected during continuous ECG monitoring at the stroke unit; the remaining cases (n=23) were diagnosed in the inpatients ward.
Distribution of potentially emboligenic arrhythmias in patients admitted to the CHUA.
| CHUA arrhythmias | ||||
|---|---|---|---|---|
| AF | Flutter | No arrhythmia | Total | |
| Previous (%) | 276 (16.6) | 6 (0.4) | 1388 (83.4) | 1664 (100) |
| Stroke unit (%) | 157 (11.3) | 1 (0.1) | 1230 (88.6) | 1388 (100) |
| Ward (%) | 23 (1.7) | 0 | 1365 (98.3) | 1388 (100) |
| Total (%) | 456 (27.4) | 7 (0.4) | 1201 (72.2) | 1664 (100) |
AF: atrial fibrillation; CHUA: Complejo Hospitalario Universitario de Albacete. Previous: arrhythmias diagnosed prior to stroke or upon the patient's arrival at the emergency department; ward: arrhythmias diagnosed during patient's stay in a conventional inpatient ward; stroke unit: arrhythmias diagnosed during continuous ECG monitoring in the stroke unit.
We compared CHUA data for each year studied to identify any variations over the 6 years of the study period, finding no statistically significant differences (statistical results not shown) for the main demographic, clinical, and aetiological variables included in the registry.
DiscussionThe most significant difference between the 2 databases is in the percentage of cardioembolic and lacunar strokes. Expanding the analysis to cover other hospital registries using the TOAST classification, we observe that the results of studies performed prior to the first decade of the 21st century14–22 are similar to those of the SDB, whereas the results of more recent studies23,24 are far more similar to our own (Fig. 1). We may therefore postulate a progressive, worldwide trend towards greater prevalence of cardioembolic ischaemic stroke, and a downward trend in the prevalence of lacunar stroke. In the CHUA database, this tendency is more pronounced if we exclusively analyse female patients (cardioembolic stroke affected 42% of women in the CHUA study vs 19% in the SDB; lacunar stroke affected 7% vs 26%). However, men were 3 times more likely to have atherosclerotic or lacunar stroke in our population. This disparity in stroke aetiology between sexes was significant in our sample, whereas it was not observed in the SDB population.
These findings may be explained in several ways. As described previously, age seems to have a strong influence over aetiology. Therefore, one possible explanation for the difference between the 2 databases in the distribution of aetiologies may be the increase in life expectancy in recent decades: the median age in the CHUA study was 74 years, vs 65 in the SDB (Table 1). Furthermore, the most frequently affected age groups in our database were patients aged over 70, in whom atherosclerotic and lacunar stroke are less prevalent and cardioembolic stroke is more frequent (Table 3). These results are consistent with those of other series which have shown that cardioembolic stroke is more frequent in older populations25,26; this may to a large extent be due to the influence of AF, whose prevalence increases exponentially with age.27,28
A role may also be played by the recent introduction of stroke units, which enable long-term ECG monitoring, and consequently the ability to detect potentially emboligenic arrhythmias.29 In our series, AF was responsible for 76% of cardioembolic strokes (Table 1). Many cases of AF were diagnosed based on observations from continuous ECG monitoring in the stroke unit; in our centre, cardiac activity is typically monitored for 48-72hours (2.5 days on average). Specifically, of all patients with AF (n=456), 157 (34%) were diagnosed at the stroke unit. The rate of AF detection in patients with no known arrhythmia at the time of admission was 13% in our series (Table 4); this is somewhat higher than the rates reported in the meta-analysis by Kishore et al.30 (overall detection rate of 11.5%, although the studies reviewed are very heterogeneous) and the study by Jiménez-Caballero et al.25 (11.8%). These results therefore corroborate the importance of stroke units, not only in acute stroke management and treatment,6,31 but also as a tool for aetiological diagnosis, which is extremely important for optimising secondary prevention treatment strategies.
In addition to the potential effects of age and admission to a stroke unit, improved control of VRFs may also play a role in the changes observed in the distribution of stroke aetiologies (Table 1). The prevalence of classic VRFs in our series is similar to that reported in other Spanish registries32 and in the SDB study. However, there does appear to have been a substantial change in the percentage of patients receiving treatment: a marked difference was observed between our series and the SDB in the prevalence of untreated AHT (10% vs 31%). Given the proven association between AHT and lacunar stroke,32,33 it is logical to consider that better control of this factor, influenced in recent years by the development of population-level primary prevention strategies,34 may have had a role in modifying the epidemiological characteristics of cerebrovascular disease, reducing the prevalence of lacunar stroke.
We should highlight the comparison between results of the CHUA database and those of the BADISEN,21 a multi-centre database created by the Spanish Society of Neurology. Being a Spanish registry, we would expect the BADISEN results to bear the greatest similarity with our own. However, while BADISEN's results are similar to those of the CHUA registry in the proportion of atherosclerotic, lacunar, and other determined causes of stroke, we did observe an increase in the percentage of cardioembolic stroke in our database. This percentage (15%) is comparable also to the difference between observed levels of stroke of undetermined cause in the 2 studies. These differences may to a great extent be due to the hypotheses discussed above. Firstly, the mean age in the BADISEN database is 68.6 years, vs 71.2 in the CHUA study. This small difference in age may have a large effect on the results given the higher prevalence of cardioembolic stroke at older ages. Secondly, during the data collection period for the article by Morín-Martín et al.21 (1996-2001), the majority of participating hospitals lacked stroke units, or at least continuous ECG telemetry. The implication of this is that many of cases of potentially emboligenic arrhythmias detected in our stroke unit probably would not have been diagnosed at the time of the BADISEN study; these cases would therefore have been classified as stroke of undetermined aetiology.
Another interesting detail arising from the comparison with the different registries listed in Fig. 1 is the high proportion of ischaemic strokes of undetermined aetiology, which has remained reasonably stable in recent decades. It is striking that despite the new techniques available for diagnosis of stroke (widespread availability of ECG, multi-modal brain MRI, cardiac monitoring in stroke units, improvements in thrombophilia detection, etc.), a reduction has not been observed in the proportion of strokes of undetermined cause, which appears, in fact, to have grown slightly over time. The definitions of the TOAST categories may influence this, over-representing stroke of undetermined cause due to the strict inclusion criteria in the other subgroups. This subgroup also includes patients with 2 potential causes of stroke, which would mean that with the increasingly comprehensive aetiological studies available, the group of strokes due to undetermined cause may grow due to the detection of various potential causes. It was not possible to study the latter hypothesis in our study, as no distinction was made between cryptogenic cases and cases where cause was undetermined due to the presence of various possibilities; this constitutes a limitation of the study. However, we consider it more likely that the same hypotheses discussed with reference to the increased prevalence of cardioembolic stroke may also explain the increase in stroke of undetermined cause. Many of these cases may in fact be attributable to undetected AF or to the so-called atrial cardiopathy, if we recognise this concept encompassing embolic strokes associated with pathologies affecting the atrial tissue.35 This disease would explain embolism linked not only to AF, but also to ageing, enlargement, or inflammation of the left atrium. Atrial cardiopathy has been shown to be more frequent in patients who also display other VRFs, particularly AHT. This association was also observed in our series, with the subgroup of patients with cardioembolic stroke displaying the highest rate of AHT. Other hypotheses that may help to explain the increased number of cryptogenic strokes include aortic arch atheroma or complex, non-obstructive atherosclerosis involving intra- or extra-cranial arteries.
Finally, the study has some other limitations which should be noted. Firstly, this is a comparison of registries of patients admitted to hospital. This limits the ability to extrapolate results to the general population, and may also entail a selection bias, as the study does not include patients with less severe strokes who were not admitted, which may understate the importance of time progression in lacunar strokes. Another potential limitation may be the distribution of races in each database (98% of patients in our study were Caucasian) and the possible influence of this factor on the difference observed between SDB and CHUA results. However, such an influence would appear to be fairly limited, as a comparative analysis of various databases from around the world has demonstrated that the differences observed appear to be influenced more by the time the study was performed than by the location or the races included. Lastly, it should be noted that we did not systematically analyse certain potentially relevant clinical variables (obesity, alcoholism, ischaemic heart disease, heart failure, valvulopathy, peripheral artery disease) which may have provided valuable additional information.
In summary, our study shows a progressive change in the aetiology of ischaemic stroke, with an increase in cardioembolic and a decrease in atherosclerotic and lacunar stroke prevalence. This shift may be influenced by population ageing, better control of classic VRFs, and the recent increase in the ability to detect emboligenic arrhythmias. If this tendency should persist, it will become even more important to continue improving secondary prevention of stroke due to cardioembolism and undetermined causes.36,37
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Sánchez-Larsen Á, García-García J, Ayo-Martín O, Hernández-Fernández F, Díaz-Maroto I, Fernández-Díaz E, et al. ¿Se ha producido un cambio en la etiología del ictus isquémico en las últimas décadas? Análisis y comparación de una base de datos de ictus actual frente a las históricas. Neurología. 2018;33:369–377.
This study was presented as an oral communication at the 66th Annual Meeting of the Spanish Society of Neurology, Valencia, November 2014.