Infection with human immunodeficiency virus (HIV) is associated with a wide range of neuro-ophthalmological manifestations, from ocular motility disorders to impairment of the afferent visual pathway.1 Most of these symptoms present in patients already diagnosed with HIV infection. However, some neuro-ophthalmological disorders, such as acute retinitis or optic neuropathy, may appear as initial manifestations of the disease. Vision loss in HIV-positive patients may indicate presence of a pathological process affecting structures ranging from the cornea to the visual cortex.2 Most cases of optic nerve involvement are due to opportunistic infections (herpes zoster, cytomegalovirus, syphilis, toxoplasmosis, cryptococcosis, histoplasmosis), CNS tumours, or drug toxicity (ethambutol and didanosine).3–6 HIV has also been described as one of the causes of optic neuropathy.1 In these cases, the typical pattern of affectation consists of anterior ischaemic optic neuropathy or neuroretinitis secondary to severe autoimmune microangiopathy. Retrobulbar optic nerve involvement secondary to HIV infection usually manifests with long-term binocular asymmetrical vision loss.7 We present the exceptional case of a patient with unilateral retrobulbar optic neuropathy which we attributed to the action of the HIV virus, and appearing as the initial manifestation of HIV infection.
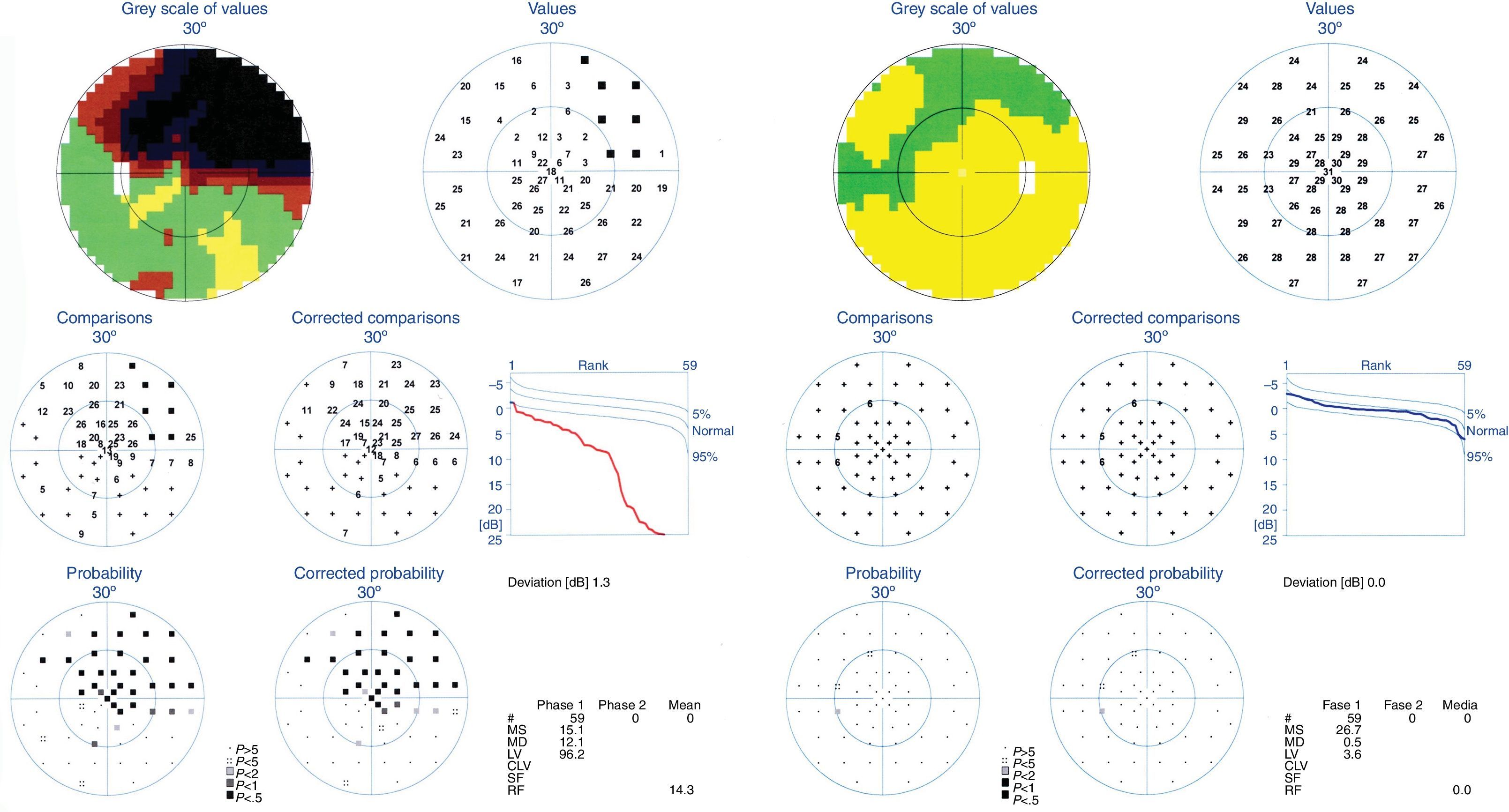
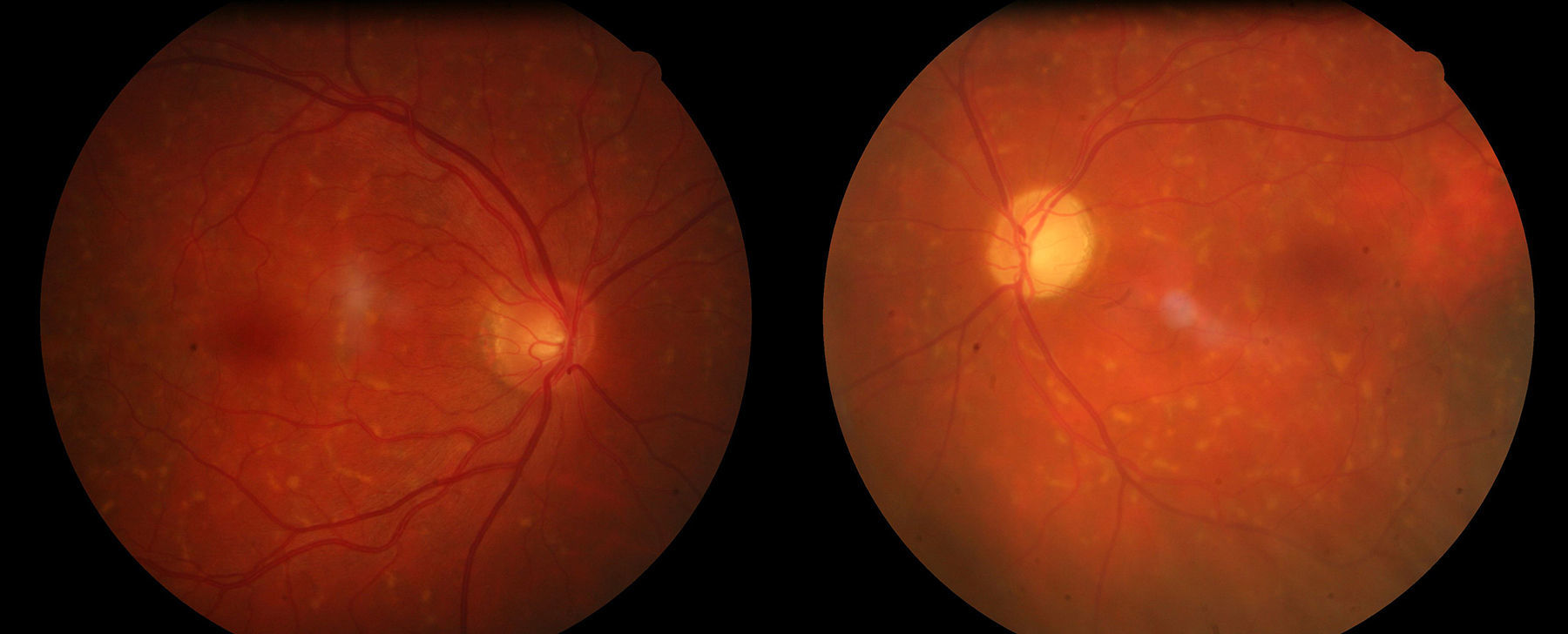
Clinical caseOur patient was a 59-year-old patient who visited our hospital due to a 3-month history of vision loss affecting the upper part of his left eye. He reported no personal or family history of interest, had no known drug allergies, and was not taking any medication. Visual acuity was 0.9 in the right eye and 0.3 in the left. He displayed severe relative afferent pupillary defect in the left eye. Extrinsic ocular motility was normal. Biomicroscopy results and intraocular pressure were also within normal limits. Eye fundus examination revealed drusen located outside the vascular arcades in both eyes, and no papilloedema. Visual field assessment (Octopus TOP G1) revealed a superior altitudinal scotoma in the left eye (Fig. 1). Acute-phase reactants, a biochemical study, a complete blood count, an MRI study, and a biochemical, cytological, and microbiological analysis of CSF all yielded normal results. Our patient tested positive for HIV. CD4 lymphocyte count revealed 721cells/mm3. Viral load was 10020copies/mL. A subsequent CSF analysis ruled out any opportunistic infections. We started antiretroviral treatment (emtricitabine, tenofovir, and efavirenz); visual acuity in the left eye had increased to 0.6 at 2 months, but superior altitudinal scotoma persisted. However, 3 months later visual acuity decreased to finger count in the left eye and examination of the eye fundus revealed optic atrophy (Fig. 2).
Together, optic nerve atrophy and the altitudinal defects revealed by the visual field test suggest an ischaemic mechanism which may be caused by HIV, given the lack of cardiovascular risk factors.8 Results from the screening tests for opportunistic infections and tumours, and the improvement in visual acuity after antiretroviral treatment support this hypothesis.9 HIV infection has also been associated with relapsing-remitting neuritis with inflammation (MS-like neuritis), which responds well to corticosteroid treatment. Some researchers suggest administering penicillin even when serology tests for syphilis are negative due to the high frequency of co-occurrence of these 2 infections.1
Closely monitoring HIV-positive patients with posterior ischaemic optic neuropathy is essential due to the likelihood of subsequent acute retinal necrosis secondary to herpes zoster or CNS lymphoma. The likelihood of experiencing this complication increases in patients diagnosed with acquired immune deficiency syndrome. Optic neuropathy secondary to HIV infection does not seem to be correlated with either the CD4 lymphocyte level or the presence of opportunistic infections.1
ConclusionUnilateral retrobulbar optic neuropathy is an infrequent manifestation of HIV infection. However, it should be included in the differential diagnosis of seropositive patients with atypical symptoms, since it may also constitute the initial manifestation of HIV infection. Diagnosis is made by exclusion, after ruling out presence of opportunistic infections, CNS neoplasm, or drug allergies.
FundingThis study has received no public or private funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Pérez-Bartolomé F, Santos-Bueso E, Ávalos-Franco N, Porta-Etessam J. Neuropatía óptica retrobulbar unilateral como primera manifestación de la infección por el virus de la inmunodeficiencia humana. Neurología. 2017;32:199–201.
This study was presented at the ninth Research Awards for Ophthalmology Residents (Ramón Castroviejo Institute of Ophthalmology Research, Faculty of Medicine, Universidad Complutense de Madrid, Spain) on 19 February 2015.