Cutaneous leishmaniasis caused by Leishmania infantum is a parasitic disease which is widely disseminated in some areas of Spain. Its most frequent manifestation is a papule or isolated, self-limiting nodule, also known as oriental sore. However, in immunocompromised patients, the condition's effects are more extensive and progressive, and progression is slower, potentially leading to systemic involvement.1 We present a case of aggressive cutaneous leishmaniasis in a patient with relapsing-remitting multiple sclerosis (RRMS) treated with fingolimod. Our hypothesis is that the aggressiveness of the disease was due to fingolimod-induced lymphopaenia.
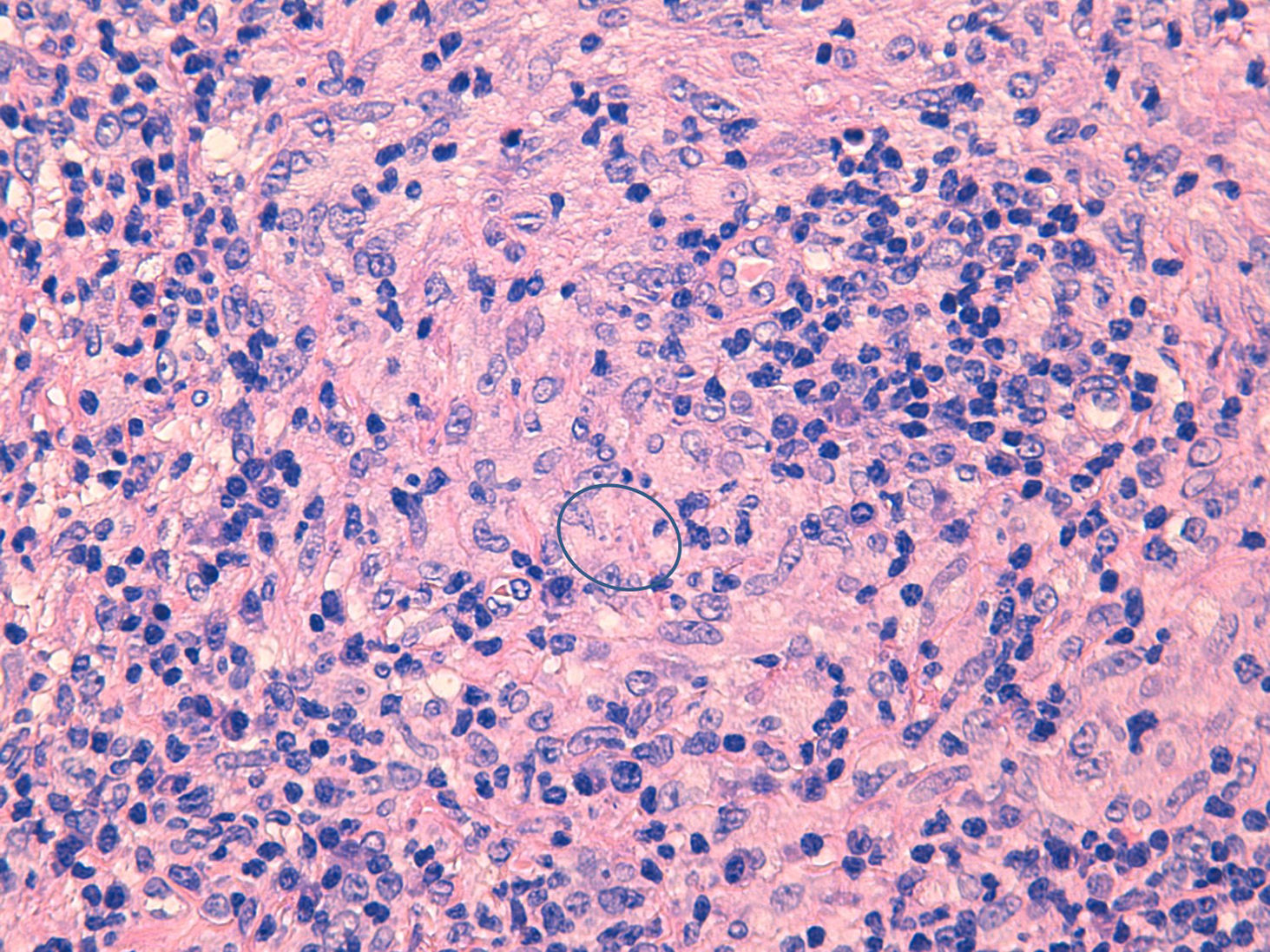
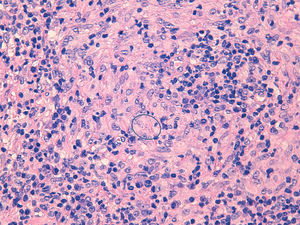
Our patient is a 32-year-old white woman diagnosed with RRMS in 2009, who had been receiving fingolimod at a daily dose of 0.5mg for 25 months. She was neurologically stable from treatment onset, displaying grade III maintained lymphopaenia (absolute lymphocyte count <500cells/mm3). The patient complained of a painful papule on the rim of the right auricle, which had expanded over the following months to cover the whole ear, becoming granulomatous and infiltrative. She also presented associated painful cervical adenopathies. The patient had no systemic symptoms; the physical examination yielded normal results. A biopsy of the lesion revealed a lymphoplasmacytic inflammatory infiltrate with non-caseating granulomatomas and amastigotes (Fig. 1); PCR was positive for Leishmania infantum. Treatment was started with intralesional amphotericin B, which was subsequently administered intravenously due to lack of response.
The development of new immunosuppressants for the treatment of MS has led to more effective disease control, but involves a higher risk of infectious complications associated with immunosuppression.2 Fingolimod, the first oral therapy for RRMS, acts by preventing the migration of lymphocytes from the lymph nodes, selectively affecting T cells expressing the homing receptor CCR7, such as CD4+ and naïve CD8+, and central memory T cells.3 This action mechanism causes lymphopaenia due to selective lymphocyte redistribution with preserved immunological memory; therefore, it does not initially translate into an increased risk of opportunistic infections associated with cellular immunosuppression.4 Although clinical trials performed before its approval for treating MS did not show a stronger association with infections in general, or opportunistic infections in particular, than treatment with placebo or interferon, the literature does include some isolated cases.5–7 In our patient, the progression of infection, its aggressiveness, and the involvement at a local level, with associated adenopathies and the need for intravenous treatment, suggest that persistent lymphopaenia associated with fingolimod may increase the risk and aggressiveness of opportunistic infections in immunocompromised patients.
Please cite this article as: Hernández Clares R, Sánchez Pedreño P, García Vazquez E, Carreón Guarnizo E, Meca Lallana JE. Leishmaniasis cutánea agresiva en paciente con esclerosis múltiple tratada con fingolimod. Neurología. 2018;33:348–349.