Cerebrovascular diseases are associated with different clinical presentations. On some occasions, these conditions may be difficult to diagnose or even misdiagnosed due to the presence of atypical signs and symptoms that may mislead neurologists and especially the patients themselves.
We present 2 cases of cerebrovascular disease associated with atypical hallucinatory symptoms which developed as the disease progressed, and briefly review the literature on Alice in Wonderland syndrome (AIWS).
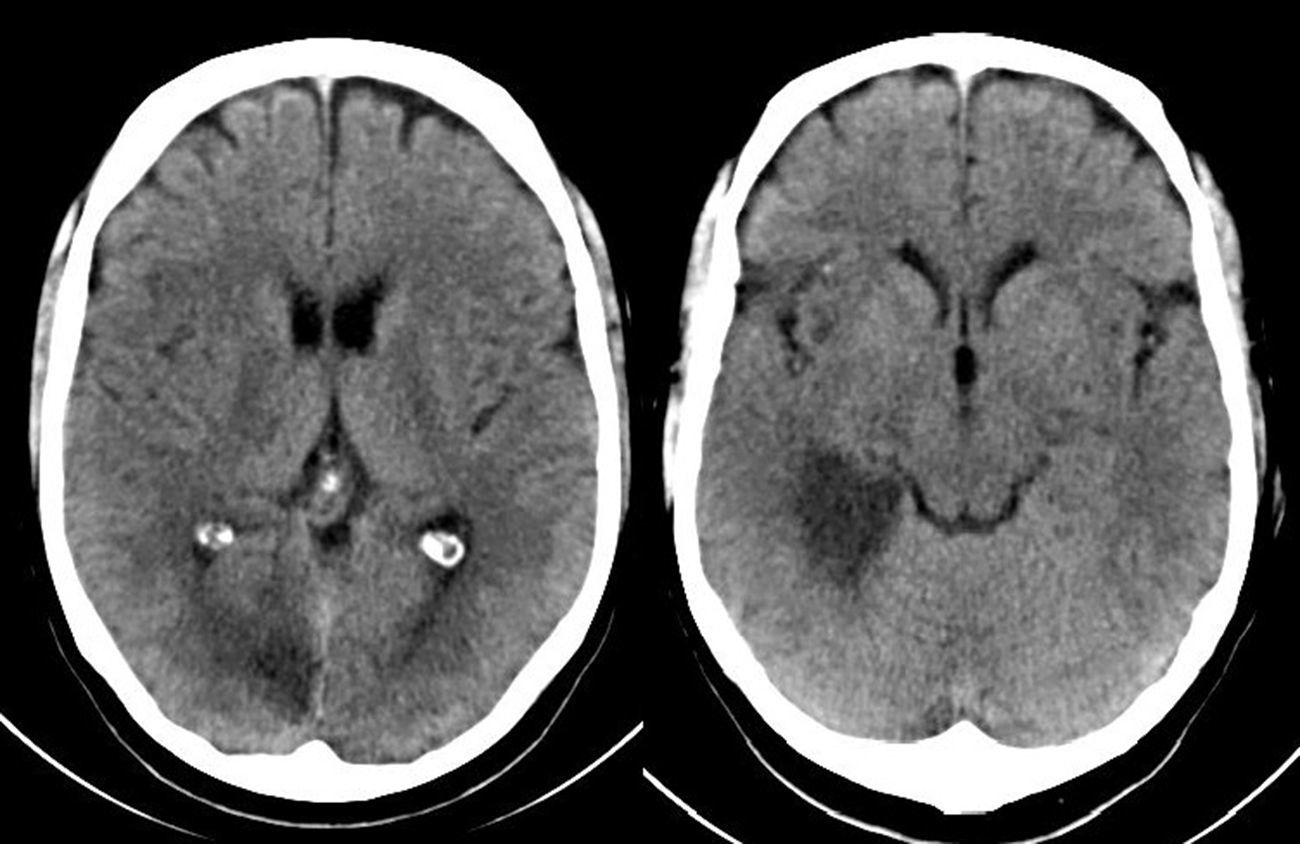
Case 1Our first patient was a 55-year-old man with a history of aortic valve disease, a mechanical prosthetic heart valve, and anticoagulation therapy with acenocoumarol. The patient visited the emergency department due to a one-day history of left leg paraesthesia progressing to the ipsilateral arm. He reported difficulties articulating words. In addition, his family described a mild transient deviation of the labial commissure, strange behaviours such as drinking from a bottle of oil and taking the same medication several times, incoherent speech, and short-term memory impairment. The patient was unaware of having exhibited any unusual behaviour over the previous days and was only worried about paraesthesia. Physical examination revealed disorientation in time, indifference towards his condition, left upper quadrantanopia, mild left upper limb paresis (4+/5) with ataxia, and left-sided brachiocrural hemihypaesthesia; plantar response was indifferent for the left foot and flexor for the right foot. A brain CT scan revealed hypodensities in the territory of the dorsolateral and temporoccipital thalamoperforating branches of the right posterior cerebral artery (Fig. 1). Upon admission, he presented multiple transient episodes of optical hallucinations. Images in the left visual hemifield were distorted (dysmorphopsia). He reported: ‘my wife's body seemed to stretch out and move away’ (macropsia and teleopsia), ‘people on my left side wore white clothes, and I saw white cars crossing my field of view’, ‘my wife seemed to be dressed in white but when she moved to my right side I could see the clothes she was actually wearing’. He saw geometric figures and inverted images in his left visual hemifield: ‘Images moved slowly and they sometimes seemed to freeze’ (palinopsia). An EEG revealed slow activity in the right posterior area, coinciding with the territory of the ischaemic lesion. We should note that the patient was aware that he was seeing optical illusions.
In view of the EEG findings and the patient's initial symptoms indicating focal occipital lobe seizures, we started antiepileptic treatment with levetiracetam. As a consequence, symptoms improved considerably and eventually disappeared.
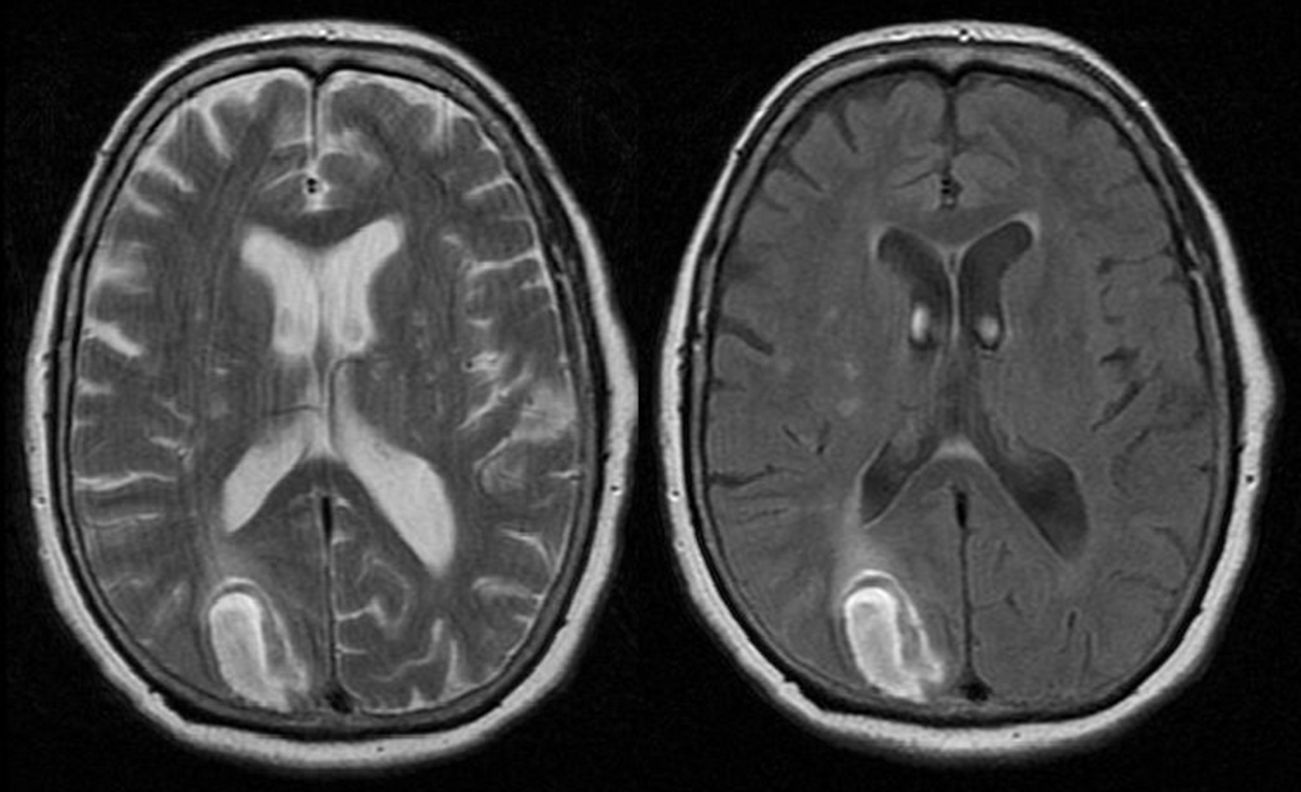
Case 2Our second patient, a 74-year-old man with a history of type 2 diabetes mellitus, came to our hospital due to sudden-onset inability to perceive anything on the left visual hemifield after experiencing a shock. The physical examination revealed left homonymous hemianopsia and mild left spatial neglect. He showed no sensory extinction; plantar reflexes were flexor bilaterally. His gait was cautious but showed no clear motor dysfunction. A brain CT scan revealed an acute haemorrhage in the right occipital area. A transcranial Doppler echo study showed that the contrast bolus reached the middle cerebral artery before the tenth beat, which was suggestive of dural fistula. A brain MRI scan revealed high signal intensity at the periphery of the lesion in T1-weighted sequences and a hyperintense lesion in T2-weighted and FLAIR sequences. Findings were compatible with an intraparenchymal haemorrhage in the right occipital cortical–subcortical area exerting a mass effect (Fig. 2).
Upon admission, the patient began to experience hallucinations: he saw objects and relatives lying on the floor and he also reported that ‘the heads of the healthcare professionals at the hospital were swollen like balloons’ (macropsia). Although no anomalies were found on the EEG, the patient started a course of levetiracetam for hallucination control, without success. Eslicarbazepine was added as an adjuvant treatment and hallucinations disappeared.
AIWS, first described by Lippman1 in 1952, was named after Lewis Carroll's well-known novel due to the similarity between the symptoms associated with this syndrome and those experienced by the main character in one of the chapters. The author had frequent migraine episodes, which may explain his accurate descriptions of visual phenomena in the novel.
This syndrome is characterised by the development of alterations in visual perception. The main type of hallucination, consisting of changes in shape (metamorphopsia), is usually accompanied by colour, size, and spatial alterations. Visual alterations include visual field inversion, palinopsia (recurrence of a visual image after the stimulus has been removed), prosopagnosia (inability to recognise familiar faces), teleopsia (objects appearing more distant than they actually are), micropsia (objects seeming smaller than their actual size; also known as lilliputianism or Lilliputian hallucination), peliopsia (objects appearing to be closer than they actually are), visual allesthesia (loss of stereoscopic vision), polyopia (perception of multiple images), zoopsia (visual hallucination of animals), achromatopsia (lack of colour vision), visual agnosia (inability to recognise familiar objects), and akinetopsia (inability to perceive motion).2–5 It may occasionally be accompanied by depersonalisation, derealisation, and alterations in time perception. As a result, AIWS may be mistaken for a psychiatric disorder.1 The most remarkable feature of this syndrome is that patients are aware that they are experiencing hallucinations.4
Some of the most frequent causes of this syndrome are CNS infections (especially those caused by Epstein–Barr virus6), migraine, epilepsy, hallucinogenic substances (LSD, marijuana, etc.), and space-occupying lesions. In some isolated cases, the syndrome has been reported secondary to treatment with topiramate and dextromethorphan. Before establishing a diagnosis of the syndrome, ophthalmological conditions such as retinal alterations should be ruled out as these may also present with metamorphopsia. AIWS is more frequent in people under 14 years.7 There may be diagnostic difficulties with this age group since symptoms may be associated with anxiety or other psychiatric alterations involving psychotic delusions.8 Brain electrical stimulation, EEG, and functional MRI studies typically show alterations in the primary visual cortex of the non-dominant hemisphere (Brodmann areas 18 and 19), which corresponds to the calcarine sulcus and the lingual gyrus; these areas tend to be hypoactive.3 Other alterations include hyperactivity in the superior parietal region of the right hemisphere, and hypoperfusion of the right frontal and parietal lobes (the latter is a visual association area) in SPECT images.6 Other studies have described frontal lobe seizures as the cause of this syndrome.8 In cases of AIWS secondary to migraine, visual evoked potentials tend to show greater amplitude, probably due to transient ischaemia of the visual tract.
In our 2 patients, the cause of AIWS was epileptic activity secondary to ischaemic and to haemorrhagic lesions, respectively; in both cases, lesions affected the occipital lobe.
Please cite this article as: Camacho Velasquez JL, Rivero Sanz E, Tejero Juste C, Suller Marti A. Síndrome de Alicia en el país de las maravillas en patología cerebrovascular. Neurología. 2016;31:418–420.