This study aimed to determine the incidence and trends of cerebrovascular disease (CVD) in the healthcare district of Lleida.
Material and methodsWe performed a population-based prospective cohort study including the entire population of the healthcare district of Lleida (440 000 people). Information was gathered from the minimum basic data set from the emergency department and hospital discharges for the period from January 2010 to December 2014. All types of stroke were included. We evaluated crude and age-standardised rates using the world population as a reference. Patients without neuroimaging confirmation of the diagnosis were excluded.
ResultsWe identified 4397 patients: 1617 (36.8%) were aged 80 years or over; 3969 (90.3%) presented ischaemic stroke, and 1741 (39.6%) were women. The crude incidence rate ranged from 192 (95% confidence interval [CI], 179-205) to 211 (95% CI, 197-224) cases per 100 000 population, in 2012 and 2013, respectively. Age-standardised rates ranged from 93 (95% CI, 86-100) to 104 (95% CI, 96-111) cases per 100 000 population, in 2012 and 2013, respectively. For all years, incidence rates increased with age, and were significantly higher among men than among women.
ConclusionThe impact of CVD in Lleida is comparable to that observed in other European regions. However, population ageing induces a high crude incidence rate, which remained stable over the five-year study period.
Determinar la incidencia de la enfermedad cerebrovascular (ECV) y su tendencia en el área sanitaria de Lleida.
Material y métodosEstudio de cohortes de base poblacional que incluyó a toda la población del área sanitaria de Lleida (440.000 personas). Se utilizaron los listados del Conjunto Mínimo Básico de Datos (CMBD) de urgencias y de las altas hospitalarias en el periodo comprendido entre enero de 2010 y diciembre de 2014. Se seleccionaron todos los episodios de ictus. Se evaluaron las tasas brutas y las tasas estandarizadas por edad utilizando la población mundial como referencia. Se excluyeron aquellos casos sin confirmación diagnóstica por neuroimagen.
ResultadosSe incluyeron 4.397 casos, de los cuales 1.617 (36,8%) fueron ≥ 80 años; 3.969 (90,3%) sujetos sufrieron un ictus isquémico, mientras que 1.741 (39,6%) casos correspondieron a mujeres. La tasa de incidencia cruda osciló entre los 192 (intervalo de confianza [IC] del 95%: 179-205) en 2012 y los 211 (IC 95%: 197-224) en 2013 casos cada 100.000 habitantes. Las tasas estandarizadas por edad oscilaron entre los 93 (IC 95%: 86-100) en 2012 y los 104 (IC 95%: 96-111) en 2013 casos por cada 100.000 habitantes. En todos los años, las tasas de incidencia fueron significativamente mayores entre los varones en comparación con las mujeres; y se incrementaron con la edad.
ConclusionesEl impacto de la ECV en Lleida es equiparable a otras regiones europeas, pero el envejecimiento de la población se traduce en una incidencia bruta elevada que se mantiene estable en los 5 años analizados.
Cerebrovascular disease (CVD) has a considerable social impact.1,2 Globally, stroke affects around 15 million people each year; of these, 6.7 million die.1,2 Furthermore, more than half of survivors are left with some kind of disability.1,2 The World Health Organization (WHO) currently estimates the incidence of stroke at 200 cases per 100 000 person-years.3–7 However, a systematic review of different epidemiological studies revealed significant differences in incidence rates according to geographical region and level of income.3–8
In Spain, CVD is the third leading cause of mortality. Few studies have analysed the incidence of stroke in different Spanish regions; furthermore, the available studies have followed different methodologies and present heterogeneous results.9,10 Therefore, estimates of stroke incidence range from 120 to 350 cases per 100 000 person-years.11–18
This study aimed to analyse the incidence of stroke and its subtypes (haemorrhagic and ischaemic stroke) in the healthcare district of Lleida, and to study stroke trends over a 5-year period.
Material and methodsWe conducted a prospective, observational study of all patients presenting stroke in the healthcare district of Lleida between 1 January 2010 and 31 December 2014. The study design considered the criteria for the “ideal” incidence study proposed by Malmgren et al.,19 Sudlow and Warlow20, and the IBERICTUS study.10 A neuroimaging study (CT or MRI) was performed prior to inclusion in the study in all cases.
The primary data source was the minimum basic dataset of the reference hospital for the study population, Hospital Universitario Arnau de Vilanova, in Lleida; we gathered data on emergency department visits and hospital discharges, coded according to the ninth revision of the International Classification of Diseases (ICD-9). In accordance with the diagnostic criteria of the WHO MONICA project, stroke was defined as rapidly developing signs of focal or global disturbance of cerebral function lasting more than 24 hours (unless interrupted by surgery or death), with no apparent non-vascular cause. The following ICD-9 codes were classified as ischaemic stroke: 433.10, 433.11, 433.21, 433.30, 433.31, 433.80, 433.81, 434.11, 434.90, 434.91, 436, 437.0, 437.1, 437.2, 437.3, 437.7, 437.8, and 437.9. Haemorrhagic stroke corresponded to codes 430, 431, and 432.9. All possible cases were subsequently reviewed by a researcher who verified and validated diagnosis following inspection of the discharge report and the clinical history. We excluded all patients with diagnosis of transient ischaemic attack (transient cerebral ischaemia, ICD-9 codes 435.0, 435.3, 435.8, and 435.9), other intracranial haemorrhages, other ill-defined cerebrovascular disease, and late effects of cerebrovascular disease (ICD-9 codes 432, 433.x0, 434.x0, 437, and 438). The reference population included all residents of the healthcare district of Lleida. Following the definition of the Spanish National Statistics Institute, we defined residents as those individuals listed in the municipal register of any town or city in the province of Lleida and living in said town or city for at least 6 months per year. The study was approved by our hospital’s ethics committee.
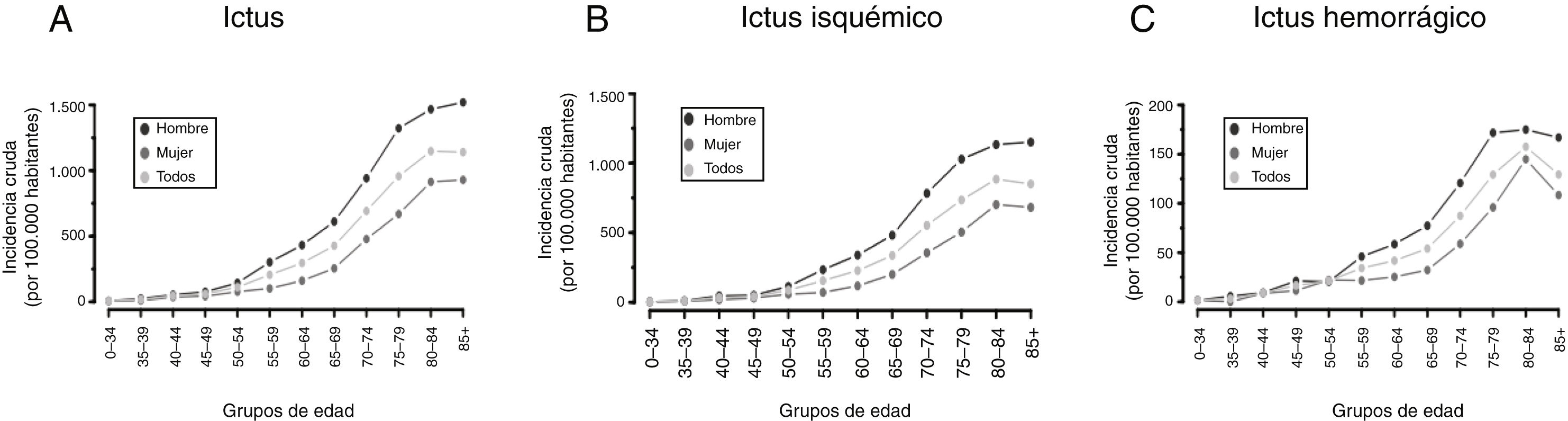
Statistical analysisOur sample was stratified by age group (0-34, 35-39, 40-44, 45-49, 50-54, 55-59, 60-64, 65-69, 70-74, 75-79, 80-84, and ≥ 85 years), sex, and stroke type (ischaemic or haemorrhagic). We calculated crude incidence rates and age-standardised rates per 100 000 population using the WHO standard population published in 2001.21 We also determined the trend in the calculated rates for the period analysed by calculating the annual percentage change (APC), which enables evaluation of trends in stroke incidence. Both global rates and APC were calculated with the Poisson distribution and are presented with 95% confidence intervals (CI). The threshold for statistical significance was set at P < .05.
ResultsA total of 4420 patients were diagnosed with stroke during the study period. We excluded 23 patients who did not live in the healthcare district of Lleida. Our final sample included 4397 patients, 1617 of whom (36.8%) were ≥ 80 years old. A total of 3969 patients (90.3%) presented stroke, with 1741 patients (39.6%) being women.
Crude incidence rates ranged from 192 cases per 100 000 population (95% CI, 179-205) in 2012 to 211 cases (95% CI, 197-224) in 2013 (Table 1). Age-standardised rates, calculated using the reference population, ranged from 93 cases per 100 000 population (95% CI, 86-100) in 2012 to 104 cases (95% CI, 96-111) in 2013. For each year, incidence rates were significantly higher in men than in women. Likewise, incidence rates increased significantly with age, rising above 1000 cases per 100 000 population among individuals aged over 79 years. Crude incidence rates remained stable over the 5-year study period, with an APC of 0.7 (95% CI, –1.4 to 2.8; P = .54). The analysis of stroke incidence trends by age group (Fig. 1) revealed a downward trend in the group of individuals aged 70-74 years (APC: –5.2 [95% CI, –10.8 to 0.7; P = .08]). The analysis by sex revealed a statistically significant increase among women aged 45-49 years (APC: 31.0 [95% CI, 2.2–8.1; P = .03]) and a decrease among women aged 70-74 years (APC: −18.9 [95% CI, −26.8 to 10.2; P < .01]). Among men, significant increases were observed in the population aged 65-69 years (APC: 9.2 [95% CI, 0.5–18.7; P = .04]). Tables 2 and 3 provide data on ischaemic and haemorrhagic stroke, respectively. The incidence of ischaemic stroke remained stable (APC: 0.62 [95% CI, −1.6 to 2.9; P = .58]). The APC for haemorrhagic stroke, in contrast, showed a slight upward trend (0.94 [95% CI, −5.62 to 7.95; P = .02]). In men, upward trends were observed in the incidence of ischaemic stroke in the age groups of 40-44 years (APC: 23.4 [95% CI, −0.1 to 52.2; P = .05]) and 65-69 years (APC: 7.8 [95% CI, −1.1 to 17.5; P = .009]). In women, incidence rates increased in the age groups of 45-49 years (APC: 41.6 [95% CI, 6.1–88.9; P = .02]) and 55-59 years (APC: 18.7 [95% CI, −2.5 to 44.6; P = .09]). Incidence rates for both stroke subtypes increased with age and in men. Thus, 60.1% of ischaemic strokes and 57.7% of haemorrhagic strokes occurred in men.
Stroke incidence by age group. Crude and age-adjusted incidence rates.
| Year | Age group | Crude incidence (95% CI) | Adjusted incidence (95% CI) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0-34 | Crude incidence (95% CI) | Adjusted incidence (95% CI) | 45-49 | 50-54 | 55-59 | 60-64 | 65-69 | 70-74 | 75-79 | 80-84 | ≥ 85 | Total cases | |||
| Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | ||||
| 2010 | |||||||||||||||
| Total | 15 (8.5) | 4 (10.6) | 13 (37.0) | 18 (54.3) | 34 (120.1) | 54 (226.7) | 61 (285.3) | 73 (402.1) | 118 (761.6) | 181 (1009.5) | 188 (1316.3) | 133 (1066.1) | 888 | 202 (189-215) | 100 (93-108) |
| Men | 8 (4.2) | 1 (4.9) | 7 (36.6) | 15 (85.7) | 20 (134.4) | 44 (357.9) | 43 (409.1) | 42 (481.9) | 68 (950.0) | 110 (1385.9) | 101 (1675.8) | 70 (1574.8) | 525 | 234 (214-254) | 131 (119-143) |
| Women | 7 (8.1) | 3 (17.5) | 6 (37.5) | 3 (19.2) | 14 (104.3) | 10 (86.7) | 18 (165.6) | 31 (328.4) | 50 (599.8) | 71 (710.5) | 87 (1053.8) | 63 (784.6) | 363 | 169 (151-186) | 74 (65-–83) |
| 2011 | |||||||||||||||
| Total | 14 (7.8) | 11 (28.9) | 15 (42.1) | 26 (77.2) | 33 (112.2) | 40 (164.2) | 62 (285.5) | 80 (435.0) | 113 (737.1) | 168 (956.5) | 146 (1003.9) | 146 (1112.0) | 854 | 193 (180-206) | 98 (91-105) |
| Men | 8 (8.5) | 10 (48.1) | 10 (51.7) | 21 (117.8) | 21 (136.6) | 32 (253.8) | 42 (391.4) | 55 (619.7) | 59 (836.5) | 98 (1261.9) | 81 (1312.8) | 73 (1553.5) | 510 | 226 (207-246) | 130 (118-142) |
| Women | 6 (7.0) | 1 (5.8) | 5 (30.8) | 5 (31.5) | 12 (85.5) | 8 (68.1) | 20 (182.1) | 25 (262.8) | 54 (652.3) | 70 (714.4) | 65 (776.2) | 73 (865.9) | 344 | 159 (142-175) | 68 (60-77) |
| 2012 | |||||||||||||||
| Total | 9 (5.1) | 8 (20.5) | 12 (33.5) | 19 (56.2) | 29 (94.8) | 55 (218.4) | 63 (286.0) | 69 (362.2) | 94 (645.0) | 164 (932.9) | 174 (1197.4) | 156 (1136.3) | 852 | 192 (179-205) | 93 (86-100) |
| Men | 4 (4.4) | 5 (23.6) | 9 (46.4) | 11 (61.1) | 23 (144.2) | 42 (321.0) | 50 (456.7) | 48 (519.2) | 55 (819.8) | 99 (1281.2) | 100 (1617.3) | 73 (1479.5) | 519 | 230 (211-250) | 127 (116-139) |
| Women | 5 (5.9) | 3 (16.8) | 3 (18.3) | 8 (50.5) | 6 (41.0) | 13 (107.5) | 13 (117.3) | 21 (214.2) | 39 (495.9) | 65 (659.7) | 74 (886.4) | 83 (943.7) | 333 | 153 (137-170) | 62 (54-70) |
| 2013 | |||||||||||||||
| Total | 14 (8.1) | 6 (15.3) | 24 (67.1) | 14 (41.1) | 35 (112.4) | 52 (202.1) | 73 (325.1) | 98 (500.2) | 107 (736.3) | 153 (905.9) | 172 (1168.2) | 181 (1274.9) | 929 | 211 (197-224) | 104 (96-111) |
| Men | 5 (5.6) | 5 (23.5) | 12 (62.2) | 7 (38.5) | 25 (153.2) | 39 (292.3) | 56 (497.6) | 71 (749.7) | 75 (1116.2) | 98 (1320.4) | 92 (1482.4) | 76 (1482.1) | 561 | 251 (230-271) | 141 (129-154) |
| Women | 9 (10.8) | 1 (5.6) | 12 (72.8) | 7 (44.0) | 10 (67.5) | 13 (104.9) | 17 (151.8) | 27 (266.8) | 32 (409.6) | 55 (580.9) | 80 (939.2) | 105 (1157.8) | 368 | 169.5 (152-187) | 70 (61-79) |
| 2014 | |||||||||||||||
| Total | 13 (7.8) | 5 (12.9) | 17 (47.4) | 25 (73.1) | 38 (120.2) | 57 (216.1) | 67 (297.1) | 88 (436.3) | 89 (579.4) | 154 (980.0) | 156 (1054.3) | 165 (1114.0) | 874 | 200 (186-213) | 98 (90-105) |
| Men | 9 (10.4) | 5 (23.8) | 14 (72.7) | 14 (76.6) | 25 (151.5) | 39 (284.3) | 46 (403.4) | 67 (686.1) | 70 (983.3) | 94 (1363.7) | 78 (1247.4) | 80 (1512.6) | 541 | 244 (223-264) | 137 (125-149) |
| Women | 4 (4.9) | 0 (0) | 3 (18.1) | 11 (69.2) | 13 (85.9) | 18 (142.2) | 21 (188.4) | 21 (201.8) | 19 (230.5) | 60 (680.2) | 78 (912.9) | 85 (892.6) | 333 | 154 (138-171) | 62 (54-70) |
| APC (95% CI); P | |||||||||||||||
| Total | 5.5 (−11.7 to 26.1); | −5.2 (−25.3 to 20.4); | 10.7 (−5.3 to 29.3); | 0.3 (−12.6 to 15.0); | 0.2 (−10 to 11.5); | 0.91 (−7.4 to 10.0); | 2.2 (−5.4 to 10.3); | 3.2 (−3.7 to 11.5); | −5.2 (−10.8 to 0.7); | −1.2 (−5.9 to 3.7); | −3.1 (−7.6 to 1.7); | 2.2 (−2.8 to 7.4); | 0.7 (−1.4 to 2.8); | ||
| .55 | .66 | .2 | .97 | .97 | .84 | .59 | .37 | .08 | .62 | .2 | .4 | .54 | |||
| Men | 15.4 (−10.7 to 49.0); | 5.2 (−20.0 to 38.2); | 16.7 (−4.0 to 41.9); | −12.1 (−25.9 to 4.1); | 3.6 (−9.0 to 18.0); | −3.5 (−12.6 to 6.6); | 2.1 (−6.7 to 11.8); | 9.2 (0.5 to 18.7); | 3.65 (−3.9 to 11.8); | 0.0 (−6.1 to 6.47); | −4.6 (−10.6 to 1.9); | −1.2 (−8.1 to 6.2); | 1.9 (−0.83 to 4.7); | ||
| .27 | .72 | .12 | .14 | .6 | .49 | .65 | .04 | .36 | > .99 | .16 | .74 | .18 | |||
| Women | −3.2 (−24.6 to 24.3); | −33.8 (−61.5 to 13.8); | 0.92 (−22.0 to 30.6); | 31.0 (2.16–8.1); | –6.38 (–22.4 to 13.0); | 15.9 (–3.13 to 38.7); | 1 (–12.8 to 17.0); | −9.3 (–19.9 to 2.7); | −18.9 (–26.8 to 10.2); | −3.0 (–10.3 to 4.9); | −1.24 (–7.9 to 8.6); | 5.3 (–1.7 to 12.9); | −1.1 (–4.3 to 2.2); | ||
| 0.8 | .14 | .94 | .03 | .49 | .11 | .89 | .12 | < .01 | .45 | .73 | .14 | .51 | |||
APC: annual percentage change; CI: confidence interval; CIR: crude incidence rate.
Incidence of ischaemic stroke by age group. Crude and age-adjusted incidence rates.
| Year | Age group | Crude incidence (95% CI) | Adjusted incidence (95% CI) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0-34 | 35-39 | 40-44 | 45-49 | 50-54 | 55-59 | 60-64 | 65-69 | 70-74 | 75-79 | 80-84 | ≥ 85 | Total cases | |||
| Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | ||||
| 2010 | |||||||||||||||
| Total | 9 (5.0) | 4 (10.6) | 12 (34.2) | 15 (45.3) | 29 (102.4) | 49 (205.7) | 55 (257.3) | 66 (363.5) | 107 (690.6) | 167 (931.4) | 179 (1253.2) | 121 (970.0) | 813 | 185 (172-198) | 90 (83-98) |
| Men | 4 (4.2) | 1 (4.9) | 6 (31.4) | 14 (80.0) | 19 (127.7) | 40 (325.4) | 38 (361.5) | 38 (436.0) | 63 (880.1) | 103 (1297.7) | 97 (1609.4) | 64 (1439.8) | 487 | 217 (198-237) | 120 (108-132) |
| Women | 5 (5.8) | 3 (17.5) | 6 (37.5) | 1 (6.4) | 10 (74.5) | 9 (78.1) | 17 (156.4) | 28 (296.6) | 44 (527.8) | 64 (640.5) | 82 (993.2) | 57 (709.8) | 326 | 151 (135-169) | 64 (56-74) |
| 2011 | |||||||||||||||
| Total | 12 (6.7) | 10 (26.2) | 11 (30.9) | 18 (53.4) | 27 (91.8) | 31 (127.3) | 57 (262.5) | 76 (413.3) | 105 (684.9) | 147 (836.9) | 132 (907.6) | 132 (1005.3) | 758 | 171 (159-184) | 86 (79-93) |
| Men | 7 (7.4) | 9 (43.3) | 8 (41.3) | 14 (78.5) | 16 (104.0) | 26 (206.2) | 37 (344.8) | 52 (585.9) | 56 (794.0) | 88 (1133.1) | 74 (1199.4) | 64 (1362.0) | 451 | 200 (182-220) | 114 (103-127) |
| Women | 5 (5.8) | 1 (5.8) | 3 (18.5) | 4 (25.2) | 11 (78.4) | 5 (42.6) | 20 (182.1) | 24 (252.3) | 49 (591.9) | 59 (602.2) | 58 (692.6) | 68 (806.6) | 307 | 142 (126-158) | 60 (52.4-69.0) |
| 2012 | |||||||||||||||
| Total | 8 (4.5) | 6 (15.4) | 9 (25.1) | 14 (41.4) | 26 (85.0) | 48 (190.6) | 54 (245.1) | 67 (351.7) | 90 (617.6) | 149 (847.6) | 154 (1059.8) | 140 (1019.7) | 765 | 173 (161-185) | 83 (76-90) |
| Men | 4 (4.4) | 3 (14.2) | 7 (36.1) | 7 (38.9) | 22 (137.9) | 37 (282.8) | 44 (401.1) | 47 (508.4) | 52 (775.1) | 89 (1151.8) | 91 (1471.8) | 66 (1337.7) | 469 | 208 (190-228) | 114 (104-127) |
| Women | 4 (4.7) | 3 (16.8) | 2 (12.2) | 7 (44.2) | 4 (27.4) | 11 (91.0) | 10 (90.3) | 20 (204.0) | 38 (483.2) | 60 (609.0) | 63 (754.7) | 74 (841.4) | 296 | 136 (121-152) | 55 (47-63) |
| 2013 | |||||||||||||||
| Total | 8 (4.6) | 6 (15.3) | 22 (61.5) | 12 (35.2) | 31 (99.6) | 47 (182.6) | 66 (293.9) | 88 (449.1) | 99 (681.3) | 141 (834.8) | 154 (1045.9) | 168 (1183.4) | 842 | 191 (178-204) | 92 (85-100) |
| Men | 2 (2.2) | 5 (23.5) | 11 (57.1) | 6 (33.0) | 24 (147.1) | 36 (269.8) | 51 (453.1) | 64 (675.8) | 69 (1026.9) | 89 (1199.1) | 84 (1353.5) | 71 (1384.6) | 512 | 229 (209-250) | 278 (116-140) |
| Women | 6 (7.2) | 1 (5.6) | 11 (66.7) | 6 (37.7) | 7 (47.2) | 11 (88.8) | 15 (133.9) | 24 (237.1) | 30 (384.0) | 52 (549.2) | 70 (821.8) | 97 (1069.6) | 330 | 152 (136–-69) | 60 (53-70) |
| 2014 | |||||||||||||||
| Total | 11 (6.6) | 4 (10.3) | 16 (44.6) | 20 (58.5) | 33 (104.4) | 53 (201.0) | 57 (252.8) | 78 (386.7) | 81 (527.3) | 137 (871.8) | 147 (993.4) | 154 (1039.7) | 791 | 181 (168-194) | 86 (80-94) |
| Men | 7 (8.1) | 4 (19.1) | 14 (72.7) | 11 (60.2) | 23 (139.4) | 37 (269.7) | 39 (342.0) | 59 (604.1) | 65 (913.1) | 83 (1204.1) | 74 (1183.4) | 74 (1399.1) | 490 | 221 (202-241) | 122 (111-135) |
| Women | 4 (4.9) | 0 (0) | 2 (12.1) | 9 (56.6) | 10 (66.1) | 16 (126.4) | 18 (161.5) | 19 (182.6) | 16 (194.1) | 54 (612.18) | 73 (854.4) | 80 (840.1) | 301 | 139 (124-156) | 54 (47-63) |
| APC (95% CI); P | |||||||||||||||
| Total | 2.1 (–16.4 to 24.7); | –7.3 (−28.2 to 19.5); | 14.2 (–3.5 to 35.1); | 1.8 (–12.9 to 19.0); | 1.4 (–9.7 to 13.7); | 2.7 (–6.3 to 12.6); | 0.9 (–7.1 to 9.4) | 2.1 (–5.0 to 9.7); | −5.1 (–10.9 to 1.1); | −1.49 (−6.42 to 3.7); | −3.5 (–8.3 to 1.5); | 3.0 (–2.2 to 8.5); | 0.6 (–1.6 to 2.9); | ||
| .84 | .56 | .12 | .82 | .82 | .57 | .84 | .57 | .1 | .57 | .16 | .27 | .58 | |||
| Men | 4.72 (–21.1 to 39.0); | 3.9 (–22.8 to 39.7); | 23.4 (–0.1 to 52.2) | −13.6 (–28.9 to 4.9) | 5.2 (–8.2 to 20.6); | −1.6 (–11.4 to 9.2); | 1.7 (–7.6 to 11.9); | 7.8 (–1.1 to 17.5); | 3.4 (–4.4 to 11.8); | –1.1 (–7.4 to 5.6); | –5.0 (–11.2 to 1.7); | –0.34 (–7.6 to 7.5); | 1.7 (–1.1 to 4.6); | ||
| .75 | .8 | .05 | .14 | .46 | .76 | .72 | .09 | .41 | .74 | .14 | .93 | .24 | |||
| Women | –0.5 (25.0–32.1); | –33.8 (61.5–13.8); | –0.8 (–25.2 to 31.6); | 41.6 (6.1–88.9); | –7.4 (–25.3 to 14.7); | 18.7 (–2.5 to 44.6); | –2.5 (–16.6 to 13.8); | –9.9 (–20.8 to 2.6); | –18.5 (26.7–9.3); | –1.9 (–9.6 to 6.5); | –1.71 (–8.8 to 5.9); | 6.1 (–1.3 to 14.0); | –0.9 (–4.4 to 2.6); | ||
| .97 | .14 | .96 | .02 | .48 | .09 | .74 | .12 | < .01 | .65 | .65 | .11 | .6 | |||
APC: annual percentage change; CI: confidence interval; CIR: crude incidence rat.
Incidence of haemorrhagic stroke by age group. Crude and age-adjusted incidence rates.
| Year | Age group | Crude incidence (95% CI) | Adjusted incidence (95% CI) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0-34 | 35-39 | 40-44 | 45-49 | 50-54 | 55-59 | 60-64 | 65-69 | 70-74 | 75-79 | 80-84 | ≥ 85 | Total cases | |||
| Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | Cases (CIR) | ||||
| 2010 | |||||||||||||||
| Total | 2 (1.1) | 0 (0) | 1 (2.85) | 3 (9.05) | 5 (17.66) | 5 (20.99) | 6 (28.06) | 7 (38.55) | 11 (71) | 14 (78.08) | 9 (63.01) | 12 (96.19) | 75 | 17 (13-21) | 9 (7-12) |
| Men | 0 (0) | 0 (0) | 1 (5.3) | 1 (5.7) | 1 (6.7) | 4 (32.5) | 5 (47.6) | 4 (45.9) | 5 (69.9) | 7 (88.2) | 4 (66.4) | 6 (135.0) | 38 | 17 (12-23) | 10 (7-15) |
| Women | 2 (2.3) | 0 (0) | 0 (0) | 2 (12.8) | 4 (29.8) | 1 (8.7) | 1 (9.2) | 3 (31.8) | 6 (72.0) | 7 (70.1) | 5 (60.6) | 6 (74.7) | 37 | 17 (12-24) | 8.8 (6-4) |
| 2011 | |||||||||||||||
| Total | 2 (1.1) | 1 (2.6) | 4 (11.3) | 8 (23.7) | 6 (20.4) | 9 (37.0) | 5 (23.0) | 4 (21.8) | 8 (52.2) | 21 (119.6) | 14 (96.3) | 14 (106.6) | 96 | 22 (18-27) | 12 (9-15) |
| Men | 1 (1.1) | 1 (4.8) | 2 (10.3) | 7 (39.3) | 5 (32.5) | 6 (47.6) | 5 (46.6) | 3 (33.8) | 3 (42.5) | 10 (128.8) | 7 (113.5) | 9 (191.5) | 59 | 26 (20-34) | 16 (12-22) |
| Women | 1 (1.2) | 0 (0) | 2 (12.3) | 1 (6.3) | 1 (7.1) | 3 (25.5) | 0 (0) | 1 (10.5) | 5 (60.4) | 11 (112.3) | 7 (83.6) | 5 (59.3) | 37 | 17 (12-24) | 8 (5-12) |
| 2012 | |||||||||||||||
| Total | 1 (0.6) | 2 (5.1) | 3 (8.4) | 5 (14.8) | 3 (9.8) | 7 (27.8) | 9 (40.9) | 2 (10.5) | 4 (27.5) | 15 (85.3) | 20 (137.6) | 16 (116.5) | 87 | 20 (16-24) | 10 (8-13) |
| Men | 0 (0) | 2 (9.5) | 2 (10.3) | 4 (22.3) | 1 (6.3) | 5 (38.2) | 6 (54.8) | 1 (10.8) | 3 (44.7) | 10 (129.4) | 9 (145.6) | 7 (141.9) | 50 | 22 (17-30) | 12 (9-17) |
| Women | 1 (1.2) | 0 (0) | 1 (6.1) | 1 (6.3) | 2 (13.7) | 2 (16.5) | 3 (27.1) | 1 (10.2) | 1 (12.7) | 5 (50.8) | 11 (131.8) | 9 (102.3) | 37 | 17 (12-23) | 7 (5–12) |
| 2013 | |||||||||||||||
| Total | 6 (3.5) | 0 (0) | 2 (5.6) | 2 (5.9) | 4 (12.9) | 5 (19.4) | 7 (31.2) | 10 (51.0) | 8 (55.1) | 12 (71.1) | 18 (122.3) | 13 (91.6) | 87 | 20 (16-24) | 11 (8-14) |
| Men | 3 (3.4) | 0 (0) | 1 (5.2) | 1 (5.5) | 1 (6.1) | 3 (22.5) | 5 (44.4) | 7 (73.9) | 6 (89.3) | 9 (121.3) | 8 (128.9) | 5 (97.5) | 49 | 22 (16–29) | 13 (10-19) |
| Women | 3 (3.6) | 0 (0) | 1 (6.1) | 1 (6.3) | 3 (20.2) | 2 (16.1) | 2 (17.9) | 3 (29.6) | 2 (25.6) | 3 (31.7) | 10 (117.4) | 8 (88.2) | 38 | 18 (12-24) | 8 (6-13) |
| 2014 | |||||||||||||||
| Total | 12 (1.2) | 1 (2.6) | 1 (2.8) | 5 (14.6) | 5 (15.8) | 4 (15.2) | 10 (44.4) | 10 (49.6) | 8 (52.1) | 17 (108.2) | 9 (60.8) | 11 (74.3) | 83 | 19 (15-24) | 10 (8-13) |
| Men | 2 (2.3) | 1 (4.8) | 0 (0) | 3 (16.4) | 2 (12.1) | 2 (14.6) | 7 (61.4) | 8 (81.9) | 5 (70.2) | 11 (159.6) | 4 (64.0) | 6 (113.4) | 51 | 23 (17-30) | 14 (10-19) |
| Women | 0 (0) | 0 (0) | 1 (6.0) | 2 (12.6) | 3 (19.8) | 2 (15.8) | 3 (26.9) | 2 (19.2) | 3 (36.4) | 6 (68.0) | 5 (58.5) | 5 (52.5) | 32 | 15 (10-21) | 7 (5-11) |
| APC (95% CI); P | |||||||||||||||
| Total | 19.4 (−19.3 to 76.5); | 12.5 (−44.2 to 127.1); | –9.2 (−40.3 to 38.3); | –5.0 (−28.8 to 26.9); | –6.9 (−30.3 to 24.4); | –11.9 (−31.6 to 13.7); | 13.03 (−10.3 to 42.4); | 17.0 (−8.6 to 49.6); | –6.7 (−25.2 to 16.4); | 1.1 (−13.6 to 18.3); | 2.1 (−13.5 to 20.5); | –6.3 (−21.0 to 11.2); | 0.9 (−5.6 to 8.0); | ||
| .38 | .74 | 0.65 | .73 | .63 | .33 | .3 | .21 | .54 | .89 | .81 | .46 | .02 | |||
| Men | 81.1 (−8.6 to 258.8); | 12.6 (−44.2 to 127.4); | –22.9 (−57.2 to 39.3); | –7.1 (−34.3 to 31.5); | –12.0 (−43.4 to 37.0); | –18.6 (−40.6 to 11.8); | 5.2 (−19.1 to 36.8); | 27.1 (−6.1 to 71.95); | 7.6 (−19.8 to 44.2); | 11.5 (−9.2 to 36.7); | 0.8 (−21.2 to 28.8); | –9.93 (−29.3 to 14.8); | 3.61 (−5.2 to 13.2); | ||
| .09 | .74 | .39 | .68 | .57 | .2 | .71 | .12 | .63 | .3 | .95 | .4 | .43 | |||
| Women | –12.1 (−48.3 to 49.7); | – | 9.7 (−41.2 to 104.8); | –0.4 (−41.0 to 68.3); | –2.9 (−34.0 to 42.8); | 2.7 (−33.8 to 59.2); | 41.2 (−14.3 to 132.7); | –2.5 (−37.0 to 50.9); | –23.0 (−45.7 to 9.2); | –12.4 (−31.7 to 12.6); | 3.1 (−17.6 to 29.2); | –2.6 (−23.5 to 24.0); | –2.54 (−12.1 to 8.1); | ||
| .63 | .77 | .99 | .88 | .91 | .18 | .91 | .14 | .3 | .79 | .83 | .63 | ||||
APC: annual percentage change; CI: confidence interval; CIR: crude incidence rate.
We studied the incidence of stroke in the province of Lleida according to the “ideal” methodology for this type of study.10 We observed a high crude incidence rate, ranging from 192 to 211 cases per 100 000 person-years. Our crude rate is higher than those reported for such other European countries and regions as Ireland,22 France,23 England,24,25 and southern Italy,26,27 similar to those reported for some regions in Germany,28 and lower than those of northern Italy,29 Eastern Europe,30 and Scotland.31 Compared to other Spanish studies, our study also found a higher incidence than did such reference studies as IBERICTUS12 and ISISCOG.11 This high incidence rate may be explained by the population pyramid in our region, which reveals an ageing population. In fact, one in every 3 patients with stroke was older than 80 years. Population studies conducted in nearby regions, such as the healthcare district of Tarragona, and including individuals older than 60 years report considerable crude incidence rates.17 However, the adjusted incidence rates are similar to those reported for most European countries, and clearly lower than those of developing countries.4
Over the 5-year study period, our population displayed a correlation between stroke incidence and age, as we may expect. This phenomenon is well documented in the literature.4,16,32 Incidence increases significantly after the age of 65 years, and exponentially after the age of 85, both for ischaemic and for haemorrhagic stroke. In the group of patients aged 80 to 84 years, crude incidence rates reached 1316 cases per 100 000 population. A clear association with sex was also observed, with incidence rates ranging from 226 to 251 cases per 100 000 person-years in men and from 153 to 169 cases in women. The association between male sex and higher incidence among individuals older than 45 years was clear for ischaemic stroke, but this was not the case for haemorrhagic stroke. The association between male sex and incidence of CVD is well documented3,33,34 and has also been demonstrated in other Spanish studies, such as IBERICTUS,12 ISISCOG,11 and the study conducted in Tarragona.13 The risk factors for CVD differ between sexes. In women, the most prevalent type of ischaemic stroke is cardioembolic; furthermore, women are usually older at the time of stroke.33,35 Studies into the progression of stroke incidence by sex reveal a downward trend among women.3 In our study, no significant differences were observed in global or sex-specific incidence rates over the 5-year period. However, we did observe a slight increase in the incidence of haemorrhagic stroke.
One of the main limitations of our study is that it included data on emergency department visits and hospital discharges gathered from the minimum basic dataset; as a result, patients who did not visit the emergency department were not included in our sample. Furthermore, we did not differentiate between patients with first-ever stroke and those with recurrent stroke, which may have led us to misinterpret prevalent cases as incident cases. Likewise, we did not analyse the vascular risk factors of each patient. This information may have been useful for explaining age- and sex-related differences in incidence rates.
Stroke continues to be one of the main causes of death and one of the leading causes of global burden of disease worldwide. A study into the incidence of stroke in our setting provides valuable information on its impact on public health. Our results show that the impact of CVD in Lleida is comparable to that observed in other European regions, but population ageing results in a high crude incidence rate that remained stable over the 5-year period analysed. These results should be considered in the design of public health policies in our region.
FundingAgency for Management of University and Research Grants, Catalan regional government(reference 2017 SGR 1628).
Conflicts of interestThe authors have no conflicts of interest to declare.
We wish to thank A. J. Valls and R. Boix for their assistance with statistical analysis.
Please cite this article as: Vena AB, Cabré X, Piñol R, Molina J, Purroy F. Evaluación de la incidencia y tendencia de la enfermedad cerebrovascular en la región sanitaria de Lleida (España) en el periodo 2010-2014. Neurología. 2022;37:631–638.