We present the case of a 48-year-old man with history of arterial hypertension, type 2 diabetes mellitus, hypercholesterolaemia, frequent cannabis use, and sporadic cocaine use. He attended the emergency department due to sudden-onset headache and blurred vision that had progressed for one week following consumption of cocaine. Before the neurological examination, the patient was assessed by the ophthalmology department, which ruled out ophthalmological disease. During the examination, blood pressure values were normal, and he exclusively presented left homonymous hemianopsia with macular sparing, and no other neurological symptom; he scored 1 on the National Institutes of Health Stroke Scale.
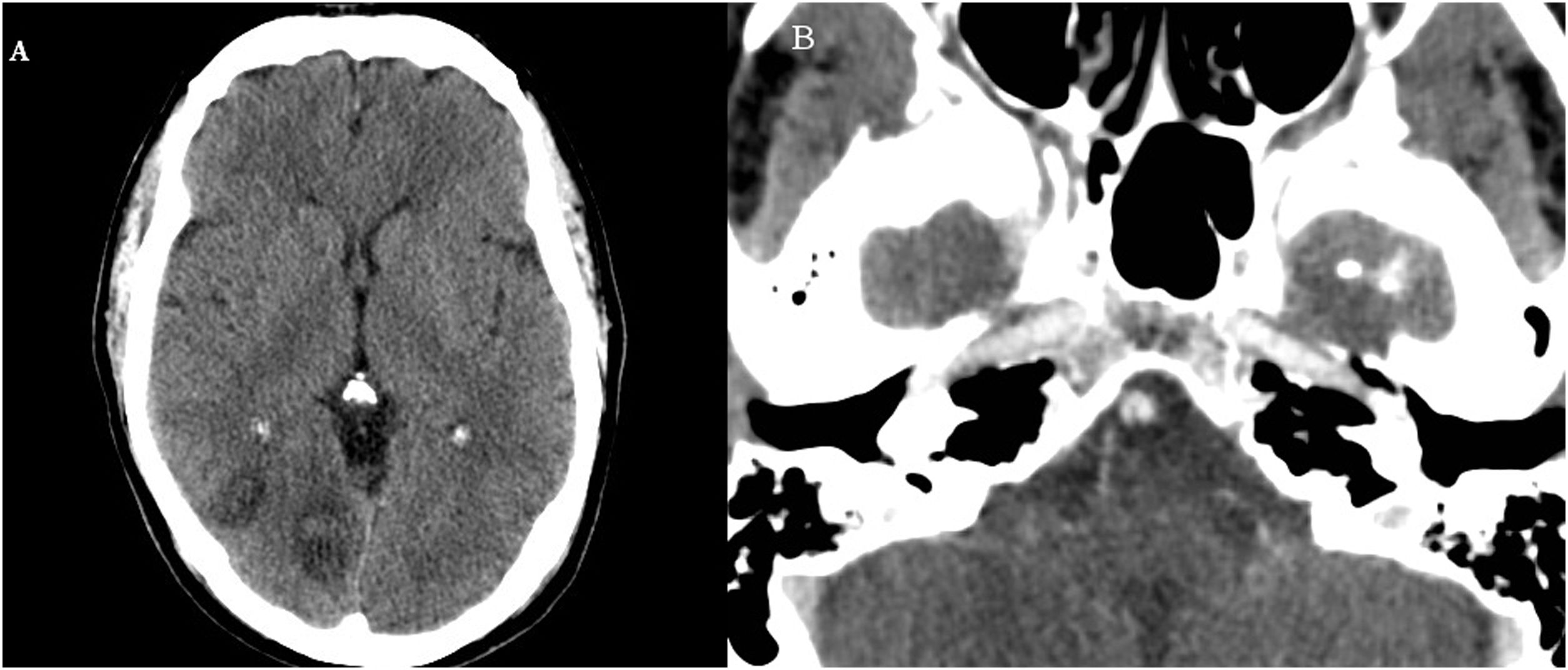
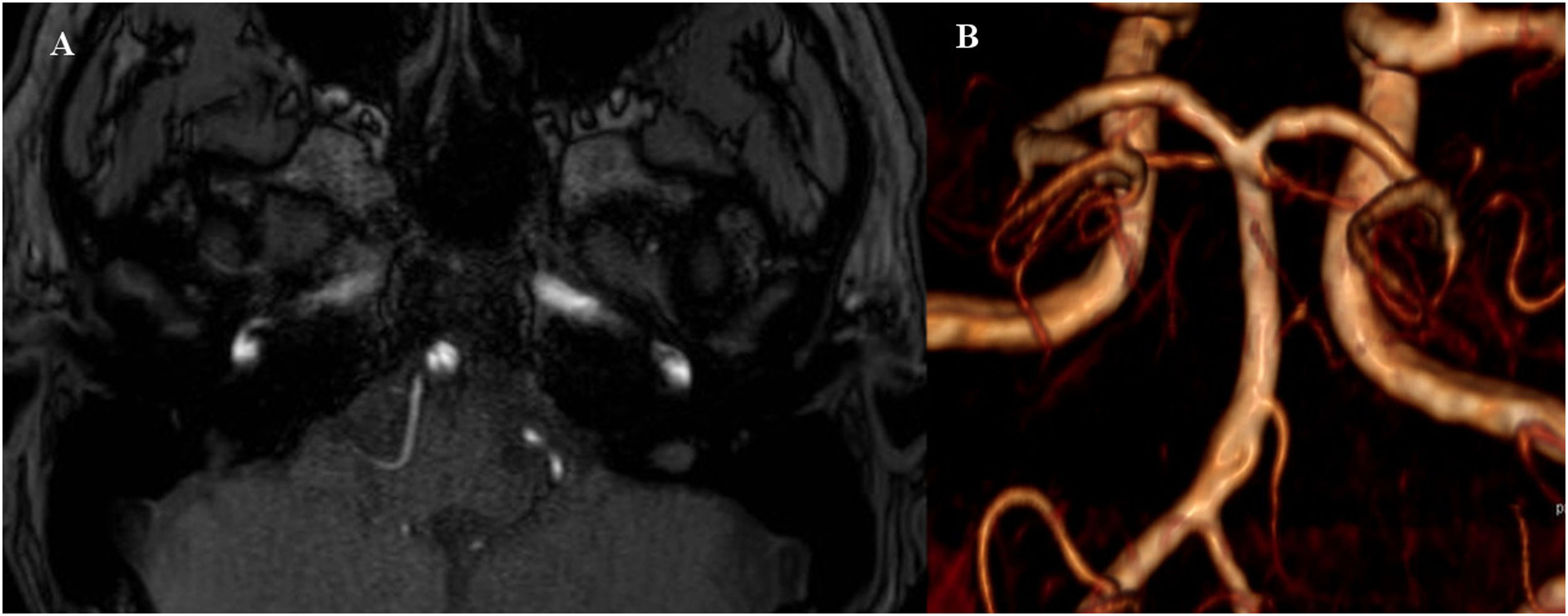
A brain CT scan and CT angiography revealed right occipital lesions (Fig. 1A) and a linear filling defect in the basilar artery (Fig. 1B). A transoesophageal echocardiography study showed small-sized patent foramen ovale. Blood testing revealed no serological or autoimmune alterations. An MRI study identified multiple subacute ischaemic lesions in the right occipital parasagittal and occipitotemporal regions, as well as in the right middle cerebellar peduncle. A 3D time-of-flight (TOF) sequence showed asymmetry of the posterior inferior cerebellar arteries, with the left artery being larger, and asymmetry of the vertebral arteries, with the right artery showing smaller diameter and progressively reduced blood flow in the distal third; a focal filling defect in the inferior third of the basilar artery was observed, which was compatible with basilar web, fenestration, or (less probably) dissection of the artery (Fig. 2A).
Axial CT scan performed at the time of diagnosis. (A) We observed 2 areas of parenchymal hypodensity in the right occipital region, both showing cortico-subcortical involvement and recent haemorrhagic foci in the interior. (B) After contrast administration, we observed a non-specific linear filling defect in the basilar artery; no other relevant alteration was observed in the supra-aortic trunks or intracranial arteries.
As the patient’s clinical symptoms improved, he was discharged home and recommended monotherapy with acetylsalicylic acid, statins, and control of vascular risk factors. A follow-up angiography study consisting of a non-contrast 3 T MRI study with 3D TOF sequences was performed at 3 months, revealing the same alteration and no signs of intramural haematoma, aneurysm, or vessel stenosis suggesting basilar dissection,1 but rather an anatomical variant (incomplete fenestration) or septum (basilar web) (Fig. 2B).
Carotid web is a cause of stroke in young adults, and is considered an atypical form of focal fibromuscular dysplasia that causes local thrombosis and subsequent arterio-arterial embolism.2 Furthermore, arterial webs in the posterior circulation are extremely rare, but may be considered a potential cause of ischaemia. Basilar fenestration is an anatomical variant presenting an approximate incidence rate of 2.3%, and is not associated with risk of stroke.3
To date, multiple cases of dysplasia in the posterior circulation have been described, although to our knowledge, only one case presented a septum in the basilar artery or basilar web.4 In our case, we report the association between 2 congenital anomalies, or rather the possibility that an incomplete fenestration may behave as a septum from a radiological perspective.
Although in our case the aetiology of the cerebral infarctions may also be related to the consumption of vasoactive substances or presence of patent foramen ovale, the fact that the infarctions affected the area distal to the septum leads us to suspect that said anomaly may have played a pathogenic role. Furthermore, the patent foramen ovale may be considered a low-risk finding, as only a few bubbles passed during Valsalva manoeuvres after injection of agitated saline; additionally, it scores 5 on the Risk of Paradoxical Embolism (RoPE) scale. However, the presence of multiple potential aetiologies in our patient prevents us from assigning an unquestionable causal role to the septum.
The presence of these anatomical anomalies may favour the indication of secondary preventive treatment with antiplatelets in accordance with international guidelines; however, for carotid web, anticoagulant or revascularisation therapy is suggested.
FundingThis study received no funding of any kind.
Conflicts of interestThe authors have no conflicts of interest to declare.