We present the case of a patient with meningitis due to pneumococcus admitted to our department with subsequent hyponatraemia and polyuria.
The patient was a 64-year-old woman operated on for closed mastoidectomy with tympanoplasty due to chronic otitis media, with hearing loss in the left ear 3 months after admission.
The patient presented with pain and suppuration in the left ear lasting for one month. A few days before admission, the pain had become more intense and was accompanied by headache, vomiting, fever and, later on, a reduction in her level of consciousness, for which reason she was referred to the emergency department, where she was seen to have stiffness in the neck and was given a cranial tomography, which was normal, and a lumbar puncture, which produced a purulent liquid.
She was admitted to the intensive care unit with a diagnosis of acute bacterial meningitis with a likely focus in the ear. Empirical treatment was begun with cephotaxime, vancomycin, and corticosteroids. A few hours after admission, she required mechanical ventilation due to a diminished level of consciousness and increased respiratory labour. Streptococcus pneumoniae was isolated in the culture of the cerebrospinal fluid and, after identifying the antibiogram (intermediate sensitivity to cephotaxime), the dosage of cephotaxime was increased and rifampicin was added. She was extubated satisfactorily after 2 days, although she still presented a confused state. Three days later, she started with polyuria (>5L/day) and progressive hyponatraemia down to 130mEq/L, elevated natriuresis (148mEq/L) with also elevated urinary osmolality (277mOsm/kg), while maintaining good renal function. Suspicion then fell on a cerebral salt-wasting (CSW) syndrome, with additional evidence of hypouricaemia (1.2mg/dL), elevated levels of cerebral natriuretic peptide (2012pg/mL) and anti-diuretic hormone in a normal range (4.2μg/L). Adequate restoration of volume with saline solution in the light of urinary sodium and water losses allowed her condition to be brought under control, and natraemia, diuresis, and neurological status returned to normal.
Hyonatraemia is one of the most common electrolytic disorders, both in habitual clinical practice and associated with diseases of the central nervous system (CNS).1,2
The causes of hyponatraemia are numerous, but most of them are synonymous with a reduction in plasma osmolality (SIADH), with water restriction forming the basis for treatment. Nonetheless, especially in cases of intracranial pathology, hyponatraemia may also be due to a different mechanism, with a loss of sodium through the kidneys of cerebral origin (CSW), in which case restricting water intake is contraindicated.2
Suspicion of this syndrome required the presence of inappropriate natriuresis for the levels of circulating sodium and volume depletion.3 Typically, the onset of hyponatraemia due to CSW occurs in the first 10 days following the neurological or neurosurgical event. Thus, in the context of an illness in the CNS, CSW is diagnosed in a patient with clinical evidence of hypovolaemia and with the following findings4:
- –
Hyponatraemia (<135mEq/L) with low plasma osmolality.
- –
Inappropriately elevated urinary osmolality (>100mOsm/kg and usually >300mOsm/kg).
- –
Diminished uric acid in plasma due to loss of urate in urine.
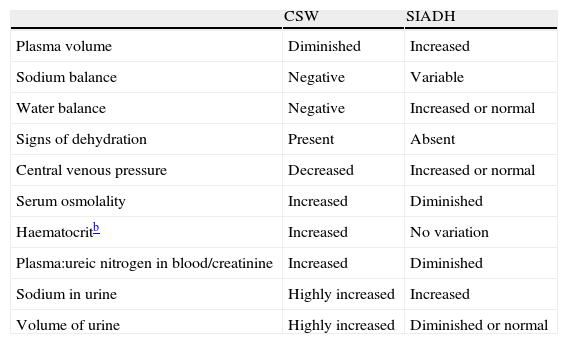
Clinical evidence of hypovolaemia is fundamental as these same findings can be found in SIADH4 (Table 1).
Differences between CSW and SIADH.a
| CSW | SIADH | |
| Plasma volume | Diminished | Increased |
| Sodium balance | Negative | Variable |
| Water balance | Negative | Increased or normal |
| Signs of dehydration | Present | Absent |
| Central venous pressure | Decreased | Increased or normal |
| Serum osmolality | Increased | Diminished |
| Haematocritb | Increased | No variation |
| Plasma:ureic nitrogen in blood/creatinine | Increased | Diminished |
| Sodium in urine | Highly increased | Increased |
| Volume of urine | Highly increased | Diminished or normal |
Please cite this article as: Pérez Cateriano V, et al. Síndrome pierde sal cerebral asociado a meningitis bacteriana. Neurología. 2011;26:441–2.