King’s College London, in collaboration with the Stroke Alliance for Europe (SAFE), has published the white paper “The burden of stroke in Europe”1; it was presented at the European Parliament (May 2017) and was drafted “to show each EU country where it stands in terms of the stroke burden and how well it is meeting the need for acute and follow-up care, including examples of good practice. The research findings for this report have led SAFE to generate a number of action points for European Union policy makers, national health service representatives and stroke support organisations.”
The document is the result of a colossal amount of work and a viable (if not necessarily the most appropriate) form of self-evaluation regarding the management of stroke in each country.
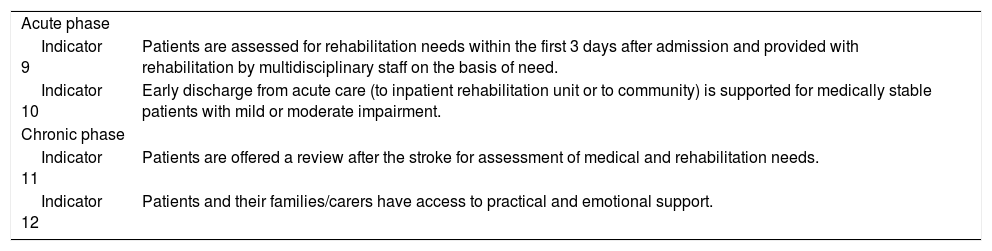
With the aim of framing the study and enabling comparisons between different countries, SAFE included 12 healthcare quality indicators to reference different parts of the stroke care “pathway.” Two indicators reference neurorehablitation in the acute phase and another 2 reference chronic-phase rehabilitation (Table 1).
Healthcare quality indicators studied.
| Acute phase | |
| Indicator 9 | Patients are assessed for rehabilitation needs within the first 3 days after admission and provided with rehabilitation by multidisciplinary staff on the basis of need. |
| Indicator 10 | Early discharge from acute care (to inpatient rehabilitation unit or to community) is supported for medically stable patients with mild or moderate impairment. |
| Chronic phase | |
| Indicator 11 | Patients are offered a review after the stroke for assessment of medical and rehabilitation needs. |
| Indicator 12 | Patients and their families/carers have access to practical and emotional support. |
After the analysis, the research team issued the following recommendations:
- 1
Too many stroke survivors have to wait too long to get an assessment of their rehabilitation needs and to actually receive therapy. Across Europe the aim should be for multi-disciplinary assessments to take place on the stroke unit, and for rehabilitation to start as soon as someone is medically stable.
- 2
Access to rehabilitation therapy must be improved. There is a particular lack of occupational, speech, and psychological therapy across Europe.
- 3
Too many stroke survivors leave hospital without on-going rehabilitation being in place. This is of particular concern for early supported discharge schemes. The evidence is clear that the effectiveness of these schemes relies upon access to rehabilitation at the same intensity as would have been provided on the stroke unit.
- 4
Ongoing, long-term support and follow-up is inadequate in many parts of Europe. We call for national systems to be developed to ensure stroke survivors’ needs are reviewed and followed up.
- 5
Countries should set targets for secondary prevention, screening for depression, and for psychological and social support.
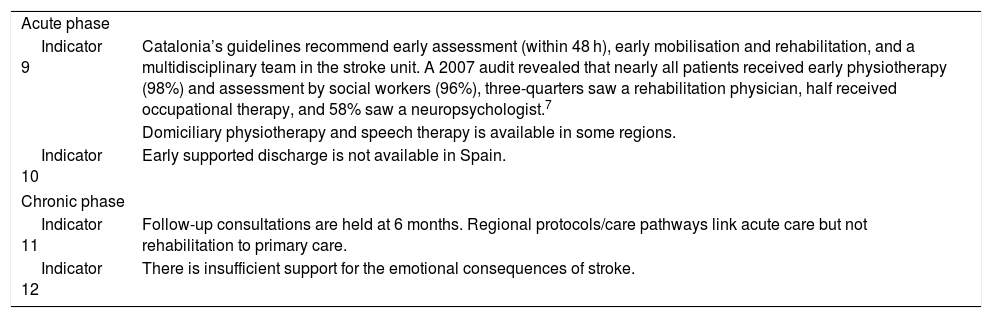
On the http://strokeeurope.eu/data-comparison website, the indicators for each country can be seen and even compared between European Union countries. Spain’s results for indicators 9, 10, 11, and 12 are shown in Table 2.
Spanish results by indicator.
| Acute phase | |
| Indicator 9 | Catalonia’s guidelines recommend early assessment (within 48 h), early mobilisation and rehabilitation, and a multidisciplinary team in the stroke unit. A 2007 audit revealed that nearly all patients received early physiotherapy (98%) and assessment by social workers (96%), three-quarters saw a rehabilitation physician, half received occupational therapy, and 58% saw a neuropsychologist.7 |
| Domiciliary physiotherapy and speech therapy is available in some regions. | |
| Indicator 10 | Early supported discharge is not available in Spain. |
| Chronic phase | |
| Indicator 11 | Follow-up consultations are held at 6 months. Regional protocols/care pathways link acute care but not rehabilitation to primary care. |
| Indicator 12 | There is insufficient support for the emotional consequences of stroke. |
In the above mentioned data, the following points are worth noting:
- 1
In Spain, data are only available for Catalonia, which probably does not reflect the reality of Spain as a whole. A multidisciplinary assessment in the acute phase (within the first 48 hours) is recommended, but this quality standard is not always reached. A national study would be interesting to show the situation of Spanish patients.
- 2
Access to physiotherapy and speech therapy during the neurorehabilitation process is another example of the different actions taken in each region. Home-based therapy has been demonstrated to be effective, and improvements are maintained beyond 6 months; this type of programme should be considered when the accessibility of outpatient services is limited.2
- 3
Approximately one-third of patients are candidates for early discharge with rehabilitation at home.3 These services have been shown to improve patients’ likelihood of recovering independence in the activities of daily living. Furthermore, there is evidence of the cost-effectiveness of this approach in comparison with the healthcare provided in a general medical ward or stroke unit (without early supported discharge).4 This has led to the implementation of these services in such countries as Sweden5 and the United Kingdom.6 In England, Wales, and Northern Ireland, 81% of hospitals have early supported discharge teams, and 35% of patients are treated by one of these teams.8 In Spain, however, no such protocols exist. We consider this to be one of the main lines of work to develop in order to improve the system’s efficiency in the stroke rehabilitation process.
- 4
For the chronic phase, we should note the Poststroke checklist, a questionnaire validated to Spanish that aims to identify rehabilitation needs after stroke.9 It is easy to administer, easy for patients to understand, and may help identify those patients presenting stroke who should be remitted to neurorehabilitation services to receive the necessary healthcare.
We would like to congratulate SAFE for their work and encourage readers to deepen their knowledge on the different aspects of the document, and healthcare managers to analyse this document and assess possible improvement actions.
Please cite this article as: Murie-Fernández M, Laxe S. Neurorrehabilitación del ictus en España, comparativa con Europa. Neurología. 2020;35:354–355.