Covid-19 has affected all people, especially those with chronic diseases, including Parkinson's Disease (PD). Covid-19 may affect both motor and neuropsychiatric symptoms of PD patients. We intend to evaluate different aspects of Covid-19 impact on PD patients.
Methods647 PD patients were evaluated in terms of PD-related and Covid-19-related clinical presentations in addition to past medical history during the pandemic through an online questioner. They were compared with an age-matched control group consist of 673 individuals and a sample of the normal population consist of 1215 individuals.
ResultsThe prevalence of Covid-19 in PD patients was 11.28%. The mortality was 1.23% among PD patients. The prevalence of Covid-19 in PD patients who undergone Deep Brain Stimulation (DBS) was 18.18%. No significant association was found between the duration of disease and the prevalence of Covid-19. A statistically significant higher prevalence of Covid-19 in PD patients who had direct contact with SARS-CoV-19 infected individuals was found. No statistically significant association has been found between the worsening of motor symptoms and Covid-19. PD patients and the normal population may differ in the prevalence of some psychological disorders, including anxiety and sleeping disorders, and Covid-19 may affect the psychological status.
ConclusionPD patients possibly follow tighter preventive protocols, which lead to lower prevalence and severity of Covid-19 and its consequences in these patients. Although it seems Covid-19 does not affect motor and psychological aspects of PD as much as it was expected, more accurate evaluations are suggested in order to clarify such effects.
La COVID-19 ha afectado a toda la población, especialmente a aquellos con enfermedades crónicas, incluyendo a los pacientes con enfermedad de Parkinson (EP). La COVID-19 puede empeorar tanto los signos motores como los síntomas neuropsiquiátricos de los pacientes con EP. El objetivo de este estudio es evaluar diferentes aspectos del impacto de la COVID-19 en los pacientes con EP.
MétodosA través de un cuestionario virtual se evaluó a 647 pacientes con EP de acuerdo con sus presentaciones clínicas relacionadas con la EP y con la COVID-19, además de la historia médica previa durante la pandemia. Se compararon con un grupo de controles sanos de la misma edad que constaba de 673 individuos y una muestra de la población general de 1.215 individuos.
ResultadosLa prevalencia de la COVID-19 en pacientes con EP fue del 11,28%. La mortalidad fue del 1,23% entre los pacientes con EP. La prevalencia de COVID-19 en pacientes con EP con estimulación cerebral profunda fue del 18,18%. No se encontró una asociación significativa entre la duración de la enfermedad y la prevalencia de COVID-19. Se halló una prevalencia mayor de COVID-19 que fue estadísticamente significativa en pacientes con EP que tuvieron contacto directo con personas infectadas con SARS-CoV-2. No se encontró una asociación estadísticamente significativa entre el empeoramiento de los signos motores y la COVID-19. Los pacientes con EP y la población general podrían diferir en la prevalencia de algunos trastornos psicológicos, incluidos los trastornos de ansiedad y del sueño, y la COVID-19 podría afectar al estado psicológico.
ConclusiónLos pacientes con EP posiblemente sigan protocolos preventivos más estrictos, lo que conduce a una menor prevalencia y gravedad de COVID-19 y de sus consecuencias en estos pacientes. Aunque parece que la COVID-19 no afecta los aspectos motores y psicológicos de la EP tanto como se esperaba, se recomienda la realización de evaluaciones más precisas para aclarar tales efectos.
In December 2019, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), causing a pneumonia-like illness known as Covid-19, emerged in China and spread quickly worldwide and is now an ongoing pandemic.1 The effect of the neurological disorder as a risk factor for Covid-19 infection is yet to be fully understood, and its impact on clinical features of these diseases needs to be well characterized.2
Parkinson's disease (PD) is one of the most common neurodegenerative disorders of the central nervous system, increasing prevalence by aging.3 As the PD occurrence is related to age and PD accompanies other comorbidities, it can be suggested that the risk of Covid-19 infection might be increased in PD patients.4 On the other hand, Covid-19 might also affect motor and neuropsychiatric symptoms of PD patients.5,6
In this study, we evaluated the prevalence of Covid-19 in 647 PD patients along with other parameters, including mortality during the pandemic, Covid-19 symptoms, and alteration in PD motor and psychological symptoms.
MethodsStudy design and populationThis cross-sectional, case-control study was approved by the Iran National Committee for Ethics in Biomedical Researches (IR.SBMU.RETECH.REC.1398.439) to investigate Covid-19 prevalence and mortality rate, its clinical features, and further consequences in PD patients compared to the general population. In this study, 647 PD patients were included who were diagnosed by a neurologist based on the UK Brain Bank criteria and were being followed up at the Referral Movement Disorder Center at Shohada Tajrish tertiary hospital, Tehran. The patients with atypical parkinsonism syndrome were excluded from the study. A sub-group of 44 PD patients who had a Deep Brain Stimulation (DBS) surgery was also studied separately. The study was carried out in November 2020, when Iran was in the third peak of the coronavirus pandemic, and Tehran was locked down. Tehran was also locked down during both previous peaks, social distancing protocols were imperative, and all citizen had to wear masks in public places. After obtaining informed consent from all patients, a questionnaire prepared for the patients, consisting of demographic data, medical history, and detailed PD-related and Covid-19-related clinical information of the patients, was completed over the phone call. The same questionnaire was designed for the control groups and the normal population sample, which has been broadcasted over social media. The questionnaire was answered by 1366 individuals, and among those, 673 and 1215 individuals were selected as the age-matched control group and the sample of the normal population, respectively. The individuals for the normal population group were selected randomly from the general population to investigate the differences between them and PD patients in terms of Covid-19 and the current pandemic implications as their age, age-related lifestyle, and underlying diseases are different from PD patients. The normal population group is representing the features of the general population with heterogeneous composition. No identifiable data was not included in the questioner such as name, phone number, and national ID numbers, for the control group.
The diagnosis of Covid-19 was made based on positive Polymerase Chain Reaction (PCR) of SARS-CoV-2 or ground glass appearance on Chest Computed tomography (CT) scan. The patients with clinical suspicion of Covid-19 due to clinical presentation of Covid-19 (i.e. fever, cough, dyspnea, fatigue, muscular pain, dizziness, and weakness), unusual and inexplicable symptoms, dropped O2 saturation, or prior contact with a Covid-19 patient went under either of these tests. A positive polymerase chain reaction (PCR) test, strong evidence of lung involvement on CT scan, or O2 saturation of below 94% were the hospitalization criteria.
OutcomeThe study's primary outcomes are the prevalence of Covid-19 in PD patients, their mortality during the pandemic, and the effect of Covid-19 and the pandemic on motor and psychological status of PD patients. The prevalence of Covid-19 is studied in different sub-groups considering influenza vaccination, family history of neurological disorders, Duration of PD, and direct contact with SARS-CoV-19 infected individuals. The PD and Covid-19 symptoms, in addition to the history of viral infections, are evaluated in this study. The history of visiting physicians during the pandemic is also considered.
Statistical analysisStatistical analysis tests were as follows: Fisher Exact Text (for categorical variable), Mann–Whitney U test (for continuous variables), and Anderson–Darling test (assessment of distribution). Statistical analysis was carried out via Excel Microsoft office, and R language (4.0.2 ed, 2020) implemented in R studio (1.3.1093 ed, 2020). The level of significance for all statistical analyses was fixed at 0.05.
ResultsPD patients’ demographic and general clinical featuresIn this study, we evaluated 647 PD patients (Mean age: 60.57±12.46, Male: 410, Female: 237) for Covid-19 prevalence of their Covid-19- and PD-related presentations. The normal population includes 1215 individuals (Mean age: 39.84±14.90), and the age-matched control group is composed of 673 individuals (Mean age: 56.32±11.62). Tremor, bradykinesia, and rigidity were the most frequent primary symptoms of PD patients, respectively. Duration of PD was about as following: (<1 year: 9.4%, 1–5 years: 37.09%, 5–10 years: 29.05%, >10 years: 24.11%) and we could not find any statistically significant association between duration of disease and prevalence of Covid-19 (p-value>0.05). During the pandemic, 71.87% of PD patients visited their physicians at hospitals or offices.
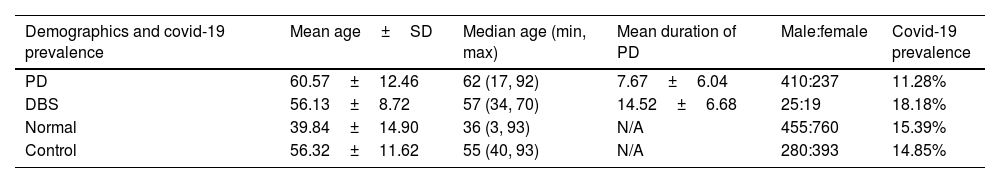
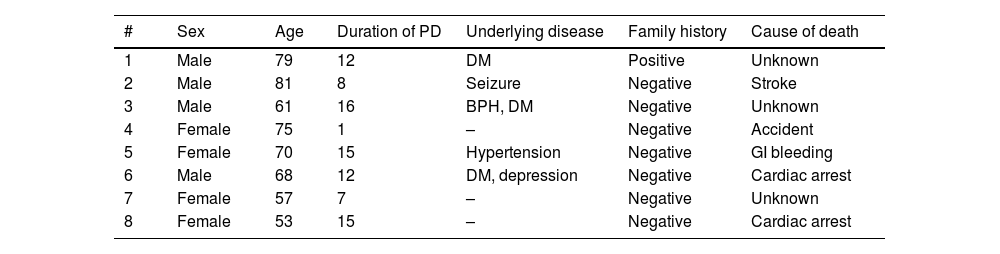
Mortality, Covid-19 prevalence, and hospitalizationThe prevalence of the Covid-19 among 647 PD patients was 11.28%, and it was significantly lower (p-value<0.05) than the normal population (15.39%). However, the difference of Covid-19 prevalence between PD patients and the control group (14.85%) was not statistically significant (p-value≈0.0605) (Table 1). The mortality rate of PD patients was 1.23% (stroke: 1, cardiac arrest without a definite diagnosis: 2, car accident: 1, gastrointestinal bleeding: 1, Unknown: 3) (Table 2). Ten PD patients (1.54%) were hospitalized because of the severity of Covid-19, while this rate was about 5.76% for the normal population and the difference between these hospitalization rates was statistically significant (p-value<0.05). On the other hand, eighteen individuals (2.67%) in the control group were hospitalized because of the severity of Covid-19, and the hospitalization rate of this group was not significantly different from that of PD patients (p-value>0.05).
Demographic information, Covid-19 prevalence and two most frequent underlying diseases of Parkinson's desease and control group.
| Demographics and covid-19 prevalence | Mean age±SD | Median age (min, max) | Mean duration of PD | Male:female | Covid-19 prevalence |
|---|---|---|---|---|---|
| PD | 60.57±12.46 | 62 (17, 92) | 7.67±6.04 | 410:237 | 11.28% |
| DBS | 56.13±8.72 | 57 (34, 70) | 14.52±6.68 | 25:19 | 18.18% |
| Normal | 39.84±14.90 | 36 (3, 93) | N/A | 455:760 | 15.39% |
| Control | 56.32±11.62 | 55 (40, 93) | N/A | 280:393 | 14.85% |
| Underlying diseases (2 most frequent) | |
|---|---|
| PD | Hypertension (25.19%) and diabetes (17.15%) |
| Control | Hypertension (26.44%) and diabetes (14.26%) |
DBS: deep brain stimulation: N/A: not applicable; PD: Parkinson's desease; SD: standard deviation.
Mortality cases among Parkinson's desease group.
| # | Sex | Age | Duration of PD | Underlying disease | Family history | Cause of death |
|---|---|---|---|---|---|---|
| 1 | Male | 79 | 12 | DM | Positive | Unknown |
| 2 | Male | 81 | 8 | Seizure | Negative | Stroke |
| 3 | Male | 61 | 16 | BPH, DM | Negative | Unknown |
| 4 | Female | 75 | 1 | – | Negative | Accident |
| 5 | Female | 70 | 15 | Hypertension | Negative | GI bleeding |
| 6 | Male | 68 | 12 | DM, depression | Negative | Cardiac arrest |
| 7 | Female | 57 | 7 | – | Negative | Unknown |
| 8 | Female | 53 | 15 | – | Negative | Cardiac arrest |
BPH: benign prostatic hyperplasia, DM: diabetes mellitus, GI: gastrointestinal; PD: Parkinson's desease.
In our study, 272 PD patients had a family history of neurological disorders, which the four most frequent of them was a family history of PD in 156 patients, a family history of Alzheimer Disease (AD) in 71 patients, a family history of migraine in 64 patients, and a family history of Multiple Sclerosis (MS) in 34 patients. No significant relation was found between having a family history of PD, MS, and migraine and higher/lower prevalence of Covid-19; However, interestingly, it has been found that such a relation existed between the family history of Alzheimer and a higher prevalence of Covid-19 (p-value<0.05).
During the last season, 32 of 647 PD patients got an influenza vaccine. No significant difference has been found in the Covid-19 prevalence, neither between PD patients who got an influenza vaccine and PD who did not (p-value>0.7) nor between PD patients and normal population who got an influenza vaccine (p-value>0.4). In addition, there was no significant difference between the prevalence of Covid-19 in PD patients and the control group who both got influenza vaccine. Moreover, the normal population and the control group were vaccinated for influenza more than PD patients (p-value<0.05 and p-value<0.01, respectively).
Covid-19 historyMyalgia (45.30%), fever (41.09%), fatigue and weakness (39.72%), cough (35.61%), headache (23.28%), dyspnea (21.91%), nasal congestion or rhinorrhea (17.80%), sore throat (13.69%) and anosmia (12.32%) were most frequent symptoms of Covid-19 in the PD patients, respectively; while the most frequent symptoms of Covid-19 in the normal population were fever (55.08%), fatigue and weakness (55.08%), myalgia (54.01%), cough (45.98%), headache (43.85%), anosmia (42.78%), loss of appetite (35.82%) and sore throat (35.29%); respectively. PD patients reported a significantly lower occurrence of viral infections before the Covid-19 pandemic in comparison to the normal population (p-value<0.05), but there was no significant difference between the occurrence of viral infections before the Covid-19 pandemic in PD patients and the control group (p-value>0.1). We found a statistically significant higher prevalence of Covid-19 in PD patients who had direct contact with SARS-CoV-19-infected individuals (72.06%) and that of the normal population with a similar condition (p-value<0.05). However, there was not a significant difference between the prevalence of Covid-19 in PD patients who had direct contact with SARS-CoV-19-infected individuals and that of the control group with a similar condition (63%) (p-value>0.1).
PD motor symptomsWorsening of motor symptoms was reported by 32.92% of PD patients, and this rate was 41.09% in PD patients who were infected with Covid-19. No statistically significant difference was found between PD patients who had Covid-19 and PD patients who did not (p-value>0.1) in terms of worsening of motor symptoms. Moreover, no significant association between the prevalence of worsening of motor symptoms and the rate of visiting physicians was observed (p-value>0.9).
Psychological evaluationsDuring the pandemic, 43% and 41.09% of all PD patients and PD patients who had Covid-19, respectively, reported deterioration in their psychological status such as occurrence or worsening of depression. No statistically significant difference has been found in the rate of deterioration in psychological status between PD patients who had and had not Covid-19 (p-value>0.7). Such difference was not also statistically significant between Covid-19-infected PD patients and Covid-19-infected normal population or Covid-19-infected control group (p-value>0.4 and p-value=1 respectively). There was a statistically significant difference between the rate of deterioration in psychological status between all PD patients and the normal population and also all PD patients and the control group (p-value<0.01 and p-value<0.01 respectively), and this rate was higher in the PD patients in both comparisons. Moreover, this rate was significantly higher in PD patients who did not have Covid-19 in comparison to this rate in not infected individuals in the normal population (p-value<0.01).
Experiencing anxiety during the pandemic was declared by 46.21% of all PD patients and 52.05% of PD patients who had Covid-19. The prevalence of anxiety was significantly lower in PD patients than the normal population (p-value<0.05). Moreover, a statistically significant difference was present between the rate of anxiety in all PD patients and in the control group (p-value<0.05). No significant difference was observed in the prevalence of anxiety between PD patients who had Covid-19 and PD patients who did not have Covid-19 (p-value>0.05). Moreover, the prevalence of anxiety in PD patients who had Covid-19 and the normal population who had Covid-19 was not significantly different (p-value>0.5). On the other hand, the difference between the prevalence of anxiety in PD patients who had Covid-19 and the control group who had Covid-19 was not statistically significant (p-value>0.5). In addition, no association was observed between the hospitalization of PD patients subsequent to Covid-19 and the prevalence of anxiety in these patients (p-value>0.5).
Experiencing sleeping problems during the pandemic was reported by 18.54% of all PD patients and 26.02% of PD patients who had Covid-19. Both the normal population and SARS-CoV-2-infected portion of the normal population demonstrated significantly higher rates of sleeping problems than all PD patients and PD patients who had Covid-19, respectively (p-value<0.01). However, there was no statistically significant difference between the rate of sleeping problems in PD patients and the control group (p-value>0.08), and also, there was no such difference between PD patients who had Covid-19 and the control group who had Covid-19 (p-value>0.1). However, the rate of sleeping problems had no significant association with neither rate of hospitalization nor prevalence of Covid-19 (p-value>0.1).
Patients with DBS deviceIn the current study, 44 of 647 PD patients underwent DBS surgery, and 8 of them (18.18%) got infected with SARS-CoV-19; there was no significant difference between the prevalence of Covid-19 in these patients with either the rest of PD patients or the normal population. Worsening of motor symptoms occurred in 38.65% of PD patients who had undergone a DBS surgery. No statistically significant difference was found in worsening of motor symptoms between PD patients who had undergone a DBS surgery and PD patients who had not (p-value>0.4).
DiscussionCovid-19 and its complications in patients with underlying diseases were among the very first concerns at the beginning of the current pandemic. The likelihood of a poor outcome in patients with PD after Covid-19 is hypothesized to be greater than the general population.6
In our study, the prevalence of Covid-19 among PD patients was 11.28%, lower than that of the normal population and age-matched control group (statistically significant and insignificant, respectively). Moreover, the mortality rate of PD patients during our study was 1.23%. Different studies have been published concerning the prevalence of Covid-19 and its mortality in PD patients; however, there is no consensus on the results. Some studies have stated the higher prevalence of Covid-19 in PD patients7; whereas, other studies have reported a similar8 or lower9 prevalence of Covid-19 in PD patients in comparison with the control group. The Covid-19 mortality rate of PD patients is also varied from 0.13% to 75% among different studies,7,9–11 similar to or significantly greater or lower than that of the general population.7–10 The difference between studies’ methodologies,8 condition of the health system in different countries,1 ethnicity of patients,1 and the timing of seeking medical attention12 are possible factors affecting the difference between the results. In our study, the lower prevalence of Covid-19 in PD patients in comparison with the normal population might be due to the tighter preventive protocols that PD patients follow because of their underlying diseases or advanced ages. This suggestion can be strengthened by our result that the prevalence of other viral infections in PD patients before the pandemic was lower than the normal population. In a study in line with our observation, it has been reported that the PD patients infected with Covid-19 were younger, and it may be due to the lower preventive measures of young people.13 Moreover, it has been suggested that the similarity between PD patients and the general population's Covid-19 prevalence may be due to higher levels of attention, percussion, and self-isolation among these patients.7 The current condition of the health system in Iran, and the difference between the ethnicity of Iranian patients and the patients with other nationalities, might be other factors that participated in such an outcome and its difference from other reports.
On the other hand, the tight preventive measures in PD patients might mask the true vulnerability of PD patients to Covid-19 when the prevalence of Covid-19 is considered as an indicator. In this sense, PD patients might be more susceptible to become infected with SARS-CoV-2 or having more serious Covid-19 complications due to the primary dysfunction of the systems (e.g., respiratory, nervous, and gastrointestinal systems) targeted later by SARS-CoV-2. PD leads to respiratory dysfunction,10 gastrointestinal problems,11 sedentary lifestyle,4,14 immune system malfunction,14 nervous system dysfunction,4,14 institutionalization,15 and a need for using medications with possible side effects and drug interactions,16 which may place PD patients at higher risks of mortality and morbidity subsequent to Covid-19 infection. However, the effect of anti-PD drugs was found to be insignificant on the prevalence of Covid-19.16 In contrast, sudden discontinuation of anti-parkinsonian drugs is recognized as a potential cause of death in PD patients infected with Covid-19.14,17 Advanced age of PD patients and long disease duration would be other risk factors for vulnerability to Covid-19.8
Concurrent underlying diseases might also play an important role. Cardiovascular diseases are suggested as possible risk factors in worse outcomes in PD patients affected with Covid-19.18 Dementia, hypertension, and PD duration may be other contributing factors for such outcomes.10 Our results can be interpreted as the consequences of the pathophysiology of PD or its medications, as we have observed that PD patients who had first-degree relatives infected with Covid-19 possessed a higher prevalence of Covid-19 in comparison with the same group in the normal population. This result indicates that possibly PD patients are at a higher risk of being infected with Covid-19. Moreover, we have observed that DBS surgery might not put PD patients at higher risk of Covid-19. Although it has been reported previously that patients with DBS device are more vulnerable to Covid-19 poor outcomes,17 similar to our results, Sainz-Amo et al. have reported DBS surgery would not affect the susceptibility of PD patients to Covid-19.15
We found that although PD patients were hospitalized because of the severity of Covid-19 more than our normal population, the rate of hospitalization among these patients was not significantly different from our control group. This may indicate that other causes are involved in increasing the rate of hospitalization rather than PD. Our observation is in line with a paper from Vignatelli et al., which states that “PD per se probably is not a risk factor for Covid-19 hospitalization”.19
In our study, 32.92%, 38.65%, and 41.09% of PD patients, PD patients who had undergone a DBS surgery, and PD patients who had Covid-19 reported worsening of motor symptoms. However, we could not find any significant association between Covid-19 and worsening of motor symptoms or between DBS surgery and worsening of motor symptoms. Similarly, it has been reported that motor symptoms did not worsen in PD patients during the lockdown period.7 On the other hand, in another study, it is reported that more than half of the patients experienced worsening of the symptoms, which were as the following: bradykinesia 47.7%, rigidity 40.7%, gait disturbances 34.5%, tremor 20.8%.9
Moreover, we could not find any association between the deterioration in psychological status and Covid-19 in PD patients. However, these problems have been reported before.9 Such association could not also be found between anxiety and Covid-19 and sleeping disorders and Covid-19. But interestingly, the normal population demonstrated higher levels of deterioration in psychological status, anxiety, and sleeping disorders than PD patients. Since our normal population was significantly younger than the population of PD patients, it is possible to interpret these results as a reflection of higher levels of psychological tensions that younger people encounter. This interpretation can be strengthened with the observation that PD patients had significantly higher levels of deterioration in psychological status and anxiety than the control group with similar mean age, indicating the age and its related psychological issues an essential factor. Therefore, it can be said the PD patients may have higher levels of deterioration in psychological status and anxiety than the control group, but these two are not as high as they are in the normal population because of possibly more psychological tensions.
The observations regarding the motor or psychological status of PD patients can be interpreted in the context of the current condition as it imposes limitations on the normal lifestyle, which may lead to deterioration in the clinical course of PD. Reduction in physical activity during quarantine may worsen both motor and non-motor symptoms as exercise may attenuate clinical symptom progression in PD.18 Availability of PD medications, health services, and physicians’ advice or guidance during the lockdowns is recognized as an important factor in the deterioration of the clinical course of PD patients. In this sense, disability in PD patients may increase due to a lack of access to suitable and sufficient medications. This condition may lead to an increase in motor, non-motor, and neuropsychiatric symptoms and possibly higher mortality.16,17
Since some PD patients could not be reached because they may have passed away or hospitalized in other facilities, the prevalence of Covid-19 and the rate of mortality might be slightly different compared to the condition that these points are taken into account. Another limitation of our study would be the inaccuracy of our control group in terms of gender and age distribution despite of similar mean age.
ConclusionPD patients possibly follow tighter preventive protocols since the prevalence of Covid-19 in PD patients, and the prevalence of other viral infections before the pandemic in these patients, and the hospitalization rate were lower than the normal population and age-matched control group. The DBS surgery did not have an association with a higher prevalence of Covid-19. Worsening of motor symptoms and deterioration of psychological status occur in PD patients; however, they do not have an association with Covid-19.
Authors’ contributionsConceptualization and study design: MS, ST.
Data collecting: MS, ME, PF.
Statistical Analysis: ST.
Literature Review: ST, ZA.
Writing Manuscript: ST, ZA, ING.
Editing: MS, ST.
Supervision: MS, AZ, ST.
Data availabilityAll data will be available by the corresponding author on a request.
Ethical statement- -
This cross-sectional, case–control study was approved by the Iran National Committee for Ethics in Biomedical Researches (IR.SBMU.RETECH.REC.1398.439).
- -
An informed consent is obtained from all patient for using their medical information.
- -
We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.
None of the authors have received any funding of any kind for either this project or other projects.
Conflicts of interestAuthors declare no conflicts of interest.
This article is taken from disease registry, titled “Parkinson's Disease Registry in Patients Referred to Neurology Clinics of Shahid Beheshti University of Medical Sciences in Tehran (SBMU-PDR)” and code number “IR.SBMU.RETECH.REC.1398.439” from ethic committee that was supported by deputy of research and technology in Shahid Beheshti University of Medical Sciences (http://dregistry.sbmu.ac.ir).