Witness accounts of the characteristics of a convulsive seizure serve as the basis for the diagnosis, classification, and treatment of epileptic syndromes; however, no such account is available in many cases.
In clinical practice, one-third of focal seizures with cognitive alterations are not controlled by antiepileptic drugs, with misdiagnosis remaining common. For this reason, video electroencephalography (EEG) monitoring is invaluable in the diagnosis, classification, and treatment of epilepsy.
We present a case which demonstrates the potential difficulty of evaluating an adult patient with absence seizures, in which treatment and “resetting” the clinical history were a help in correctly diagnosing the condition and selecting an appropriate treatment.
The patient was a 45-year-old man who was referred from another hospital, with no relevant family history; 15 years earlier, he had developed recurrent “disconnections” from his surroundings accompanied by occasional oral automatism, lasting approximately 5seconds, during which posture was maintained. These episodes featured no associated sensory aura, dystonic posture, or tonic-clonic seizures and occurred approximately 4 times per day; the patient had no memory of the event. The physical examination revealed no pathological findings. Given the symptoms described, the patient was diagnosed with temporal lobe epilepsy (with complex partial seizures).
A brain magnetic resonance imaging scan yielded normal results, as did a blood test with complete blood count; studies of liver function, iron metabolism, and kidney function; and an autoimmune study. EEGs were performed on 3 occasions, always displaying normal readings.
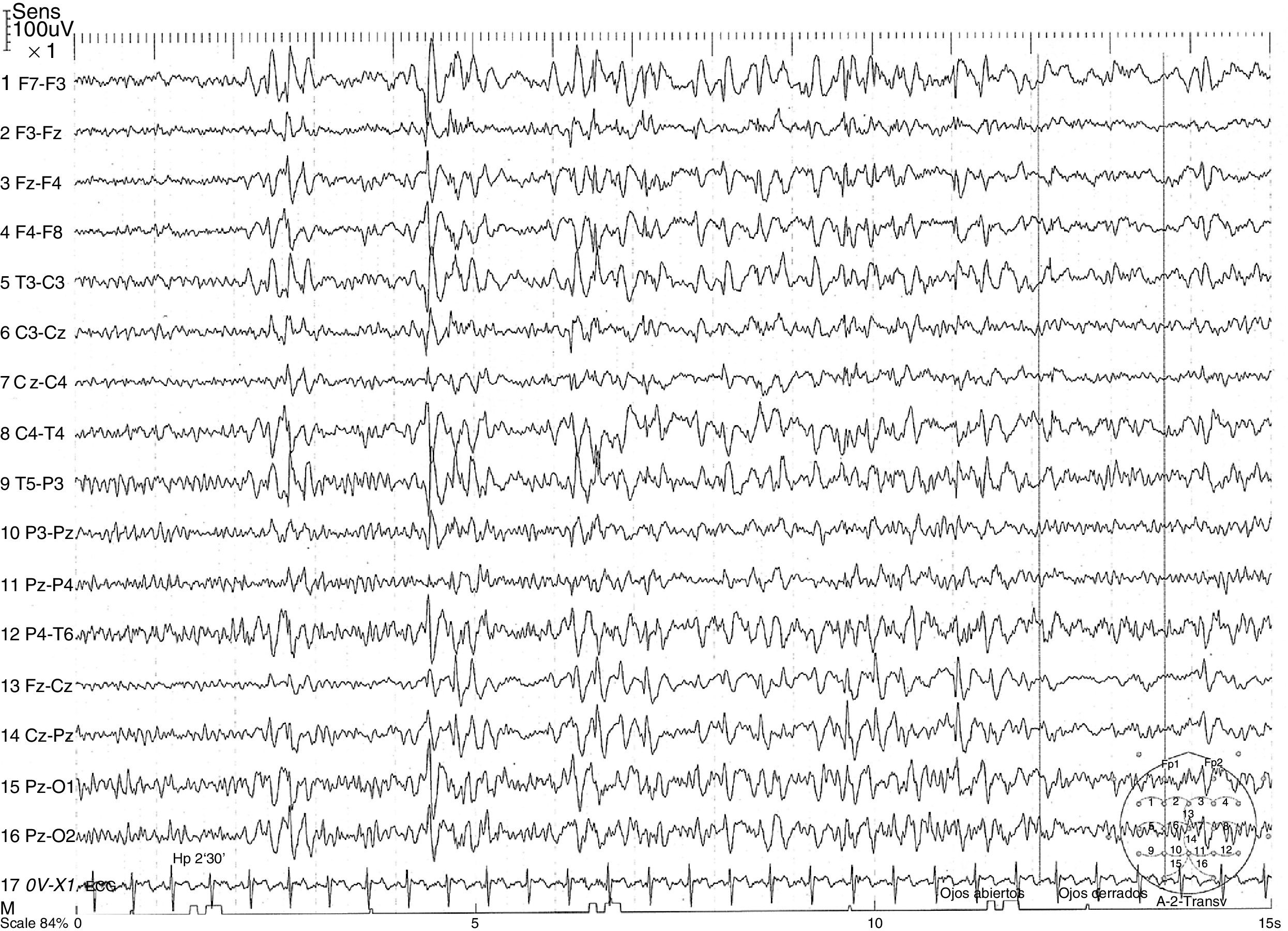
The patient was treated with various antiepileptic drugs, both in monotherapy and in combination therapy. Drugs administered were: clonazepam, lamotrigine, and valproate, which did not achieve seizure control; oxcarbazepine, perampanel, and pregabalin, which were withdrawn due to adverse effects; and carbamazepine and lacosamide, which increased seizure frequency. The patient's diagnosis was reconsidered due to the exacerbation caused by the latter 2 drugs, and a video EEG was performed, successfully recording a seizure. The reading displayed a generalised, synchronous, symmetrical 3.5-Hz spike-and-wave discharge (Fig. 1), which lasted 7seconds and coincided with the patient's disconnection from his surroundings and oral automatism.
A discussion of the patient's clinical history with family members revealed that his school teacher had complained of frequent “distractions” in class when the patient was 14 years old. These went unnoticed as they were never witnessed by the family.
Given the new information provided by the family and the video EEG results, the patient was diagnosed with juvenile absence epilepsy (JAE) and started with zonisamide and levetiracetam, which reduced seizure frequency to one per month.
JAE accounts for approximately 10% of cases of idiopathic generalised epilepsy,1 generally appearing during adolescence and improving from the fourth decade of life.
EEG typically reveals generalised, synchronous, symmetrical, 3.5-Hz spike-and-wave discharge, coinciding with an altered level of consciousness, usually lasting 5-20seconds.
Some studies suggest that calcium channels are a key factor in absence seizure pathogenesis.2 As is the case with most types of idiopathic generalised epilepsy, genetic factors play a more important role than environmental factors. Like childhood absence epilepsy, JAE manifests as an abrupt change in the patient's level of consciousness, with total or partial absence of response to external stimuli. This is frequently associated with palpebral myoclonic movements and oral automatism. In comparison to childhood absence seizures, JAE seizures tend to be longer in duration (mean duration, 16 seconds), are not clearly related with circadian rhythm (seizures occur shortly after awakening), affect level of consciousness less severely, tend to be associated with generalised tonic-clonic seizures (in up to 80% of cases), and occasionally feature mild myoclonic tremor of the type observed in juvenile myoclonic epilepsy (15%-25% of cases).
Interictal EEG readings are usually normal and seizures are often triggered by hyperventilation; video EEG is usually the diagnostic test of choice. Neuroimaging studies do not reveal pathological abnormalities.
Nearly 80% of patients remain seizure-free with classic antiepileptic drugs such as ethosuximide and valproate; levetiracetam is also a good treatment option.3 Inadequate seizure control may lead to the development of atypical absence seizures, particularly in patients treated with such drugs as carbamazepine, oxcarbazepine, vigabatrin, gabapentin, and pregabalin.
This case demonstrates the potential difficulty involved in differentiating complex partial seizures from absence seizures in adult patients. In our patient, the normal results in the routine EEG and the lack of consideration given to the “distractions” in class resulted in a misdiagnosis of temporal lobe epilepsy. This led to the administration of incorrect and occasionally contraindicated treatments (carbamazepine, lacosamide, oxcarbazepine, and pregabalin), exacerbating the absence seizures. It was this exacerbation that led us to reassess the diagnosis and therapeutic approach, confirming the new diagnosis with video EEG.
Animal models have shown that correct, early treatment not only suppresses seizures, but also prevents the development of associated histological alterations.4
Zonisamide is an antiepileptic drug that stabilises the cell membrane and acts on voltage-dependent sodium channels and calcium channels5,6; the latter are one of the main factors involved in the pathophysiology of absence seizures. Responder rates for the drug are 87.5% in cases of typical absence seizures and 46.3% for atypical seizures7; the drug rarely causes severe adverse effects, even at high doses.
The main differential diagnosis to be taken into account is mesial temporal lobe epilepsy, which is clinically characterised by prodromes, complex automatism, and postictal confusion8; the latter symptom is not usually present in adult and/or juvenile absence seizures. Mesial temporal lobe epilepsy also displays markedly different EEG readings and more severe cognitive alterations than JAE. Another diagnosis that should be considered is juvenile myoclonic epilepsy, which may present as disconnection from the patient's surroundings; however, this condition is distinguished by myoclonic jerks, distribution following the circadian rhythm (with greater seizure frequency upon awakening), and EEG findings of generalised 3-6-Hz spike-and-wave discharge of short duration (1-3seconds, vs 8-30seconds in JAE). Furthermore, these readings are not always accompanied by clinical signs, which are almost always present in JAE. JAE is distinguished from Jeavons syndrome by the fact that the latter is a form of reflex epilepsy characterised by palpebral myoclonus, which may or may not be associated with absence seizure. As a general rule, this is induced by eye closure; patients are also highly sensitive to light, which can be a trigger factor. EEG studies show generalised 3-6-Hz spike-and-wave discharges.
FundingThe authors have received no private or public funding.
Please cite this article as: Camacho Velásquez JL, Rivero Sanz E, Sanabria Sanchinel AA, Santos Lasaosa S, Mauri Llerda JA. Sobre la dificultad diagnóstica de las ausencias en el adulto. Neurología. 2018;33:403–405.
This study has not been submitted previously to any journal, nor has it been presented at any meeting or congress.