Optic nerve drusen (OND) are hyaline bodies made up of amino acids, ribonucleic acid, and small quantities of iron and calcium. Their pathogenesis is still largely unknown.1,2 Incidence estimates range between 3 and 4 cases per 1000 inhabitants and they are slightly more likely to affect women than men. OND are normally bilateral, asymmetric, and asymptomatic.3 When symptoms do appear, the condition typically presents with a decrease in visual acuity (VA) or visual field (VF) loss. OND are not usually visible in the eye fundus during childhood since they remain covered by the optic disc until around the third decade of life. They are frequently associated with such ocular vascular anomalies as presence of cilioretinal arteries, vessel tortuosity, peripapillary neovascularisation, and occlusive vascular diseases. B-mode ultrasonography remains the gold standard diagnostic test; it detects hyperreflective lesions in the optic disc with posterior acoustic shadowing.1 VF testing and optical coherence tomography (OCT) are also useful for monitoring disease progression. The latter procedure appears to be more sensitive than perimetry for detecting nerve fibre loss in early stages of the disease. Less sensitive and specific diagnostic tools include computed tomography (CT) and fluorescein angiography (FA).4
We present the exceptional case of a patient with OND and severe VF alterations in both eyes (OU) resembling optic neuropathy.
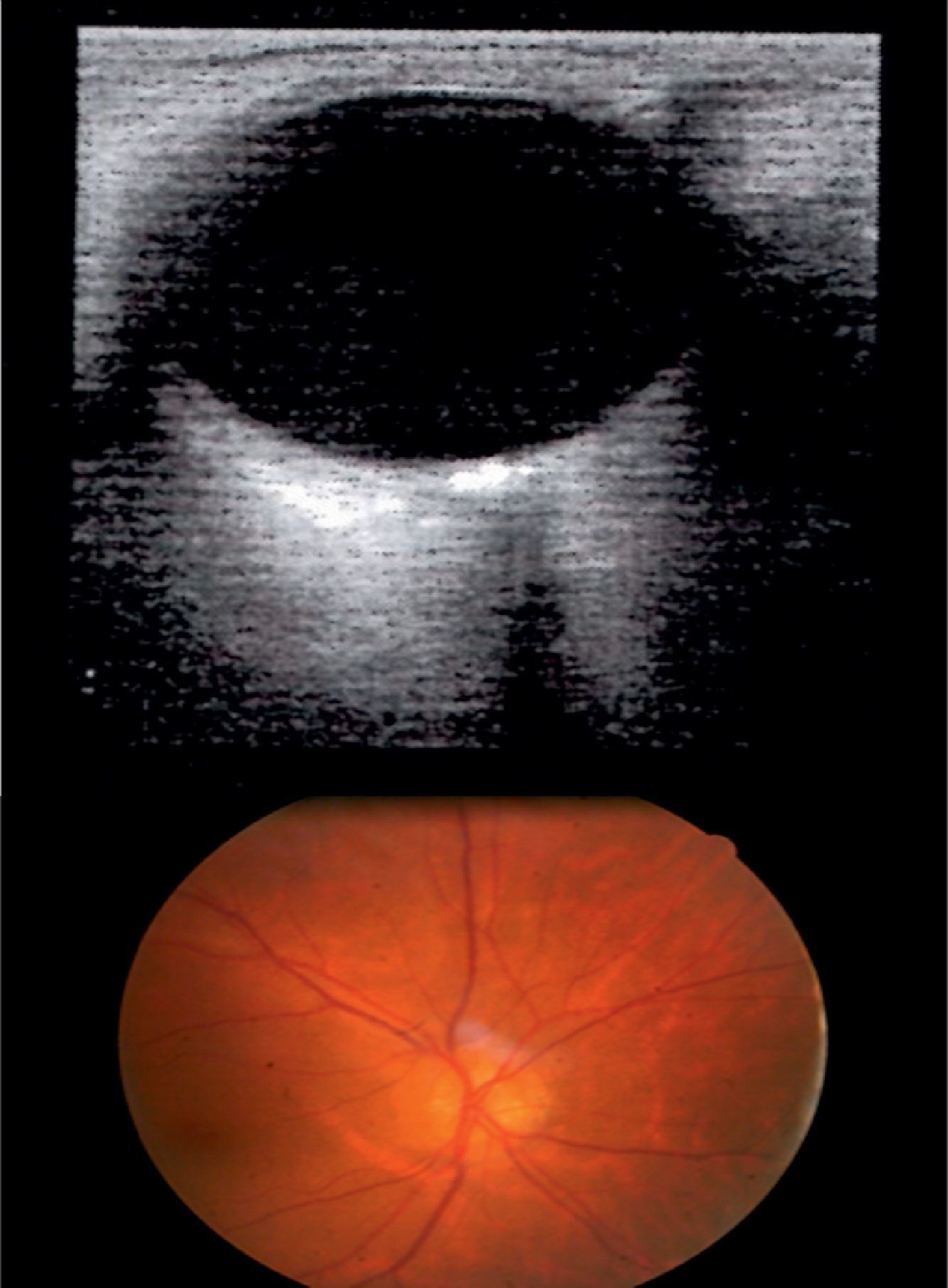
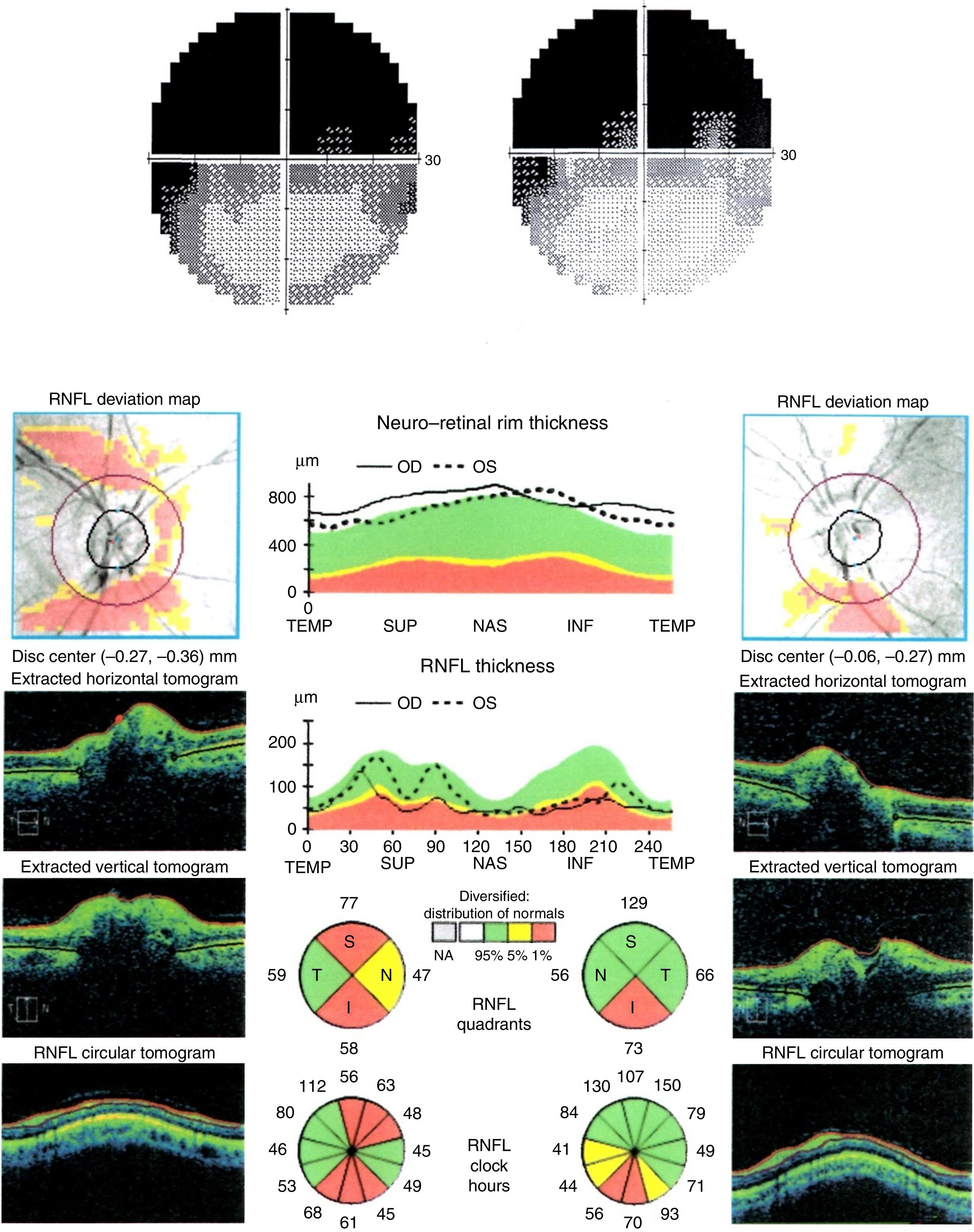
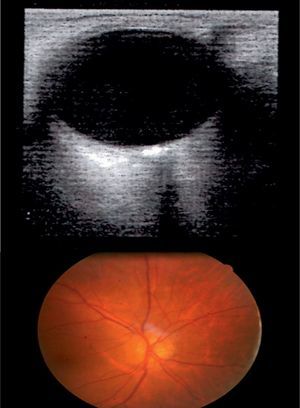
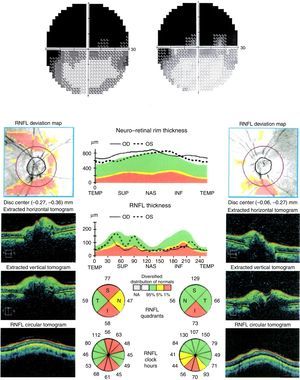
The patient was a 30-year-old woman who reported a one-year history of progressive decreases in VA and VF loss in OU, which did not improve with optical correction. She displayed no other visual symptoms. The patient's personal and family history revealed no relevant findings or known drug allergies. She was not taking any medication. In the VA test, the patient was able to count fingers at 1m with the right eye and 0.3m with the left eye; VA did not improve with pinhole glasses. The confrontation VF test revealed deficiencies in the upper area of the VF in OU. Biomicroscopy results, intraocular pressure, and intrinsic and extrinsic ocular motility were all within normal limits. OND were observed in the eye fundi in OU. The B-mode ultrasound scan revealed hyperechoic artefacts with posterior acoustic shadowing in the optic nerve head in OU, confirming the diagnosis of OND (Fig. 1). Repeated Humphrey VF tests (SITA-Standard 24-2 programme) showed progressive superior altitudinal defects in OU. OCT revealed thinning of the retinal nerve fibre layer (RNFL) in both optic nerves in several quadrants, especially the lower ones (Fig. 2). Results from laboratory analyses, electrophysiological tests, and a gadolinium contrast MRI were within normal limits.
Progression of superior altitudinal VF defects and structural damage in the inferior quadrants as shown by the OCT suggest anterior ischaemic optic neuropathy (AION). However, the chronic presentation of the condition, preservation of the temporal quadrants in OU, the absence of optic disc oedema, and relative afferent pupillary defect make it difficult to confirm this diagnosis. The presence of OND most likely provides the sole explanation for decreased VA and VF defects.
The pathogenesis of this process is not yet understood. OND are considered benign, but on occasions they may exert a direct mechanical effect which compromises the axoplasmic flow in the optic nerve head (compartment syndrome). This will alter local homeostasis and result in localised oedema leading to overall atrophy and consequent ganglion cell death. The severity of OND has been correlated with thinning of the RNFL. Damage, which is initially limited to the anterior part of the nerve, may spread and result in retrograde involvement over time.
No effective treatment has been described for these patients. Some authors recommend neuroprotective drugs, but few studies have demonstrated the efficacy of this approach.5
ConclusionAlthough rare, OND are a potential cause of progressive vision loss which may mimic VF alterations associated with optic neuropathy, as in the case presented. Optic neuropathy should be considered a possible complication of OND.
Please cite this article as: Pérez-Bartolomé F, Cifuentes-Canorea P, Santos-Bueso E, García-Feijoó J. Simulación de neuropatía óptica por drusas. Neurología. 2016;31:651–653.