Socioeconomic status is a factor that influences health-related behaviour in individuals as well as health conditions in entire populations. The objective of the present study was to analyse the sociodemographic factors that may influence knowledge of stroke.
MethodCross-sectional study. A representative sample was selected by double randomisation. Face-to-face interviews were carried out by previously trained medical students using a structured questionnaire with open- and closed-ended questions. Adequate knowledge was previously defined. The Mantel–Haenszel test and adjusted logistic regression analysis were used to assess the association between knowledge of stroke and the study variables.
Results2411 subjects were interviewed (59.9% women; mean age 49.0 [SD 17.3] years) Seventy-three per cent were residents of urban areas, 24.7% had a university education, and 15.2% had a low level of schooling. Only 2.1% reported earning more than 40000euros/year, with 29.9% earning less than 10000. Nearly 74% reported having an excellent or good state of health. The unemployment rate was 17.0%. Prevalence of ‘adequate knowledge’ was 39.7% (95% CI: 37.7%-41.6%). Trend analysis showed an association between knowledge of stroke and income (Z=10.14, P<.0001); educational level (Z=15.95, P<.0001); state of health (Z=7.92, P<.0001); and employment status (Z=8.98, P<.0001).
ConclusionsEducational level, income, employment status, and state of health are independent factors for adequate knowledge of stroke. Public awareness campaigns should present material using simple language and efforts should be directed towards the most disadvantaged social strata in particular.
El nivel socioeconómico es un factor que condiciona el comportamiento individual ante la salud y las condiciones de salud de la población. Se evalúa la asociación entre factores socio-demográficos y el conocimiento del ictus en la población general.
MétodoEstudio transversal. Los sujetos fueron seleccionados por un sistema de asignación al azar doble. Se administró un cuestionario estructurado con preguntas abiertas y cerradas mediante entrevistas cara a cara. El «conocimiento adecuado» fue definido previamente. Se utilizaron el test de Mantel-Haenszel y la regresión logística con modelos ajustados para evaluar la asociación entre el conocimiento del ictus y las variables estudiadas.
ResultadosEntrevistas, 2.411; 59,9% mujeres; edad media±desviación estándar, 49,0±17,3años. El 74% reside en área urbana. Un 24,7% tenía estudios universitarios, el 15,2% un nivel de escolarización bajo. Solo el 2,1% declaraba ganar mas de 40.000euros/año y un 29,9% menos de 10.000. Casi el 74% declaró tener un excelente o buen nivel de salud. El desempleo fue del 17,0%. La prevalencia de «conocimiento adecuado» fue del 39.7% (IC del 95%, 37,7%-41,6%). El análisis de tendencias mostró una asociación entre conocimiento y nivel económico (z=10,14; p<0,0001); nivel de estudios (z=15,95; p<0,0001), estado de salud (z=7,92; p<0,0001) y situación laboral (z=8,98; p<0,0001).
ConclusionesEl nivel de estudios y renta, disponer de trabajo y gozar de salud son factores independientes de un «conocimiento adecuado» del ictus. Las campañas educativas deberían realizarse con un lenguaje sencillo y dirigirse con especial interés a las clases sociales mas desfavorecidas.
Several studies in the literature have identified an association between vascular disease and different socioeconomic risk factors.1 Some of these studies have shown that socioeconomic parameters, specifically income, have a greater influence on vascular health than do many classic risk factors. In fact, they may serve as predictors of vascular diseases.2 Studies have also shown that subjects who have not finished secondary studies tend to display unhealthy lifestyles and poor control over vascular risk factors.3 The same is true of individuals who are unemployed and those performing unskilled or low-paid jobs.3 Other studies have shown that level of income may have a negative impact on health, and their findings have revealed an association between income and stroke risk. One study even found a correlation between income inequality and stroke mortality.4
Likewise, preventing delays should be the main objective during the pre-hospital phase of stroke care in order to provide patients with the best possible treatment.5 Delays to acute stroke care have been identified at different levels: the patient level (patient or family did not recognise symptoms of stroke or seek medical assistance urgently); the emergency unit and doctor level (when stroke patient transfer is not prioritised); and the hospital level (delays in neuroimaging tests or inefficient in-hospital procedures).6 Nevertheless, the longest delays take place during the pre-hospital phase,7,8 and the time interval between symptom onset and the first call for medical help accounts for the largest part of the delays.9–12 The main reasons for these delays include lack of knowledge of symptoms and also denial of the disease and the hope that symptoms might spontaneously resolve.
Therefore, raising public awareness of stroke symptoms so that both patients and bystanders can recognise them should reduce the time between the event and the intervention by first responders, as has been shown in some studies.13,14 Studies aimed at identifying demographic, social, cultural, behavioural, and clinical factors associated with prehospital delays provide new targets for the development of more effective stroke education campaigns.15 This study examines the association between different socioeconomic factors and a good level of stroke knowledge in a representative sample of the general population residing in the region of Extremadura.
MethodsCross-sectional, exploratory, and analytical study. All individuals aged 18 or older living in Extremadura, with no cognitive impairment and willing to participate, were considered potential candidates. For selection of the sample, we used the census sections of Extremadura, available from the database of Spain's National Statistics Institute. These data were updated as of 1 January 2008. All 966 census sections had the same likelihood of being selected. A simple random sample of 10% of all population units was conducted. Within each census district, a second random sample was taken, this time neighbourhood-specific and with the same likelihood of being selected.
The procedure for collecting information was a structured questionnaire and a face-to-face interview. Interviews were conducted by medical students at the University of Extremadura who had previously been trained in the interview method by the researcher; they were performed between July and October 2009.
The first section of the questionnaire collected the following sociodemographic variables: sex, age, area of residence (rural=population with <10000 inhabitants; urban=population with >10000 inhabitants), profession, educational level (little to no studies, primary, secondary, or university studies), income level (<10000, 10001-20000, 20001-30000, 30001-40000 or >40000euros/year), marital status (single, married, widowed, separated, divorced), occupational status (student, employed, unemployed, or retired), and state of health (very good, good, fair, poor, or very poor). The second section contained a list of open-ended questions about knowledge of stroke, its symptoms, risk factors, and unhealthy habits. Possible valid answers when asked about symptoms were neurological signs and warning signs resembling intense headache, paralysis, sensory disorder, visual disorder, balance disorder, altered language or speech, and loss of consciousness. Classic risk factors were regarded as valid answers to the question of diseases that can favour stroke. Valid answers for habits or lifestyles associated with stroke were listed as smoking, excessive consumption of alcohol, drug use, sedentary lifestyle, obesity, and high levels of stress. This section also included specific closed-end questions to determine the weight of each risk factor and habit. The third section consisted of open-ended questions about the respondent's hypothetical response to presenting or witnessing warning signs of a cerebrovascular event in a relative, and upon suspecting stroke or transient ischaemic attack in a family member or himself/herself. Answers were coded in the following seven categories for purposes of analysis: I would call the family doctor, I would go to the health centre, I would go to the hospital without delay, I would call emergency services (112) immediately, I would wait until the symptom disappears and then consult, I would wait until the symptom disappears, and I would not know what to do.
The survey included questions regarding perceived severity of stroke compared to that of other vascular diseases, such as acute myocardial infarction. We also inquired about subjects’ sources of information on stroke. The last section contained questions about the respondent's experience with the disease and presence of any risk factors or unhealthy habits. Results from this last section are not included in the present article.
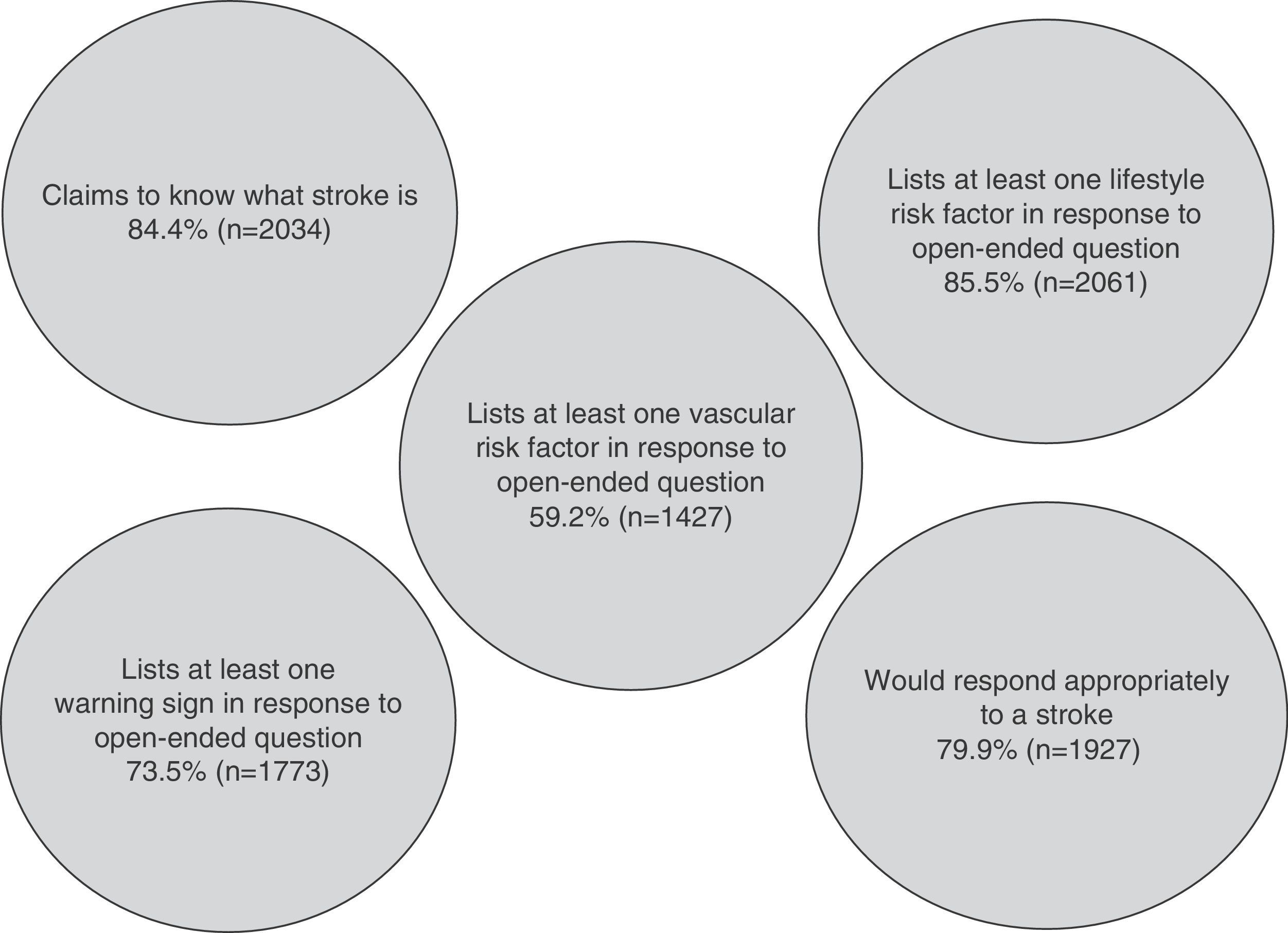
Fig. 1 shows the construct made with data from the second and the third sections of the survey. By consensus of the research group, this construct defines the main variable of the study (‘adequate knowledge of stroke’) as present in an individual expressing understanding of the concept, mentioning at least one stroke symptom, listing at least one vascular risk factor/unhealthy habit/lifestyle choice, and stating a correct potential response to stroke (calling 112 or going directly to the hospital). This definition has been modified and adapted from the literature.16 The study protocol was approved by the Ethics Committee at Hospital Universitario Infanta Cristina.
Statistical analysisWe performed a descriptive analysis of the demographic characteristics of the individuals surveyed. For continuous variables, means were used as a measure of central tendency, and standard deviations as a measure of dispersion around the mean. Normal distribution for continuous variables was tested using the Kolmogorov–Smirnov test. For purpose of this analysis, subjects were classified by age as younger than 66 or 66 and older. In the univariate analysis, we estimated prevalence with its 95% confidence interval and used the normal approximation to allow for the random variation of the sampling process. As measures of association, we used the prevalence odds ratio (POR) and calculated the 95% confidence interval using the Wilson score interval without continuity correction. For ordinal variables or those with more than two categories, we performed trend analysis using the Mantel–Haenszel test. Lastly, binary logistic regression models adjusted to age, sex, and place of residence were created for every sociodemographic factor studied. The model used the forced entry method with P>.10 as the exclusion criterion and P<.05 as the inclusion criterion. Hosmer–Lemeshow goodness-of-fit test was used for the logistic regression models. A level of P<.05 was regarded as statistically significant both in the univariate analysis and in the adjusted analysis. Statistical analysis was completed using SPSS version 15.0 (SPSS, Inc.).
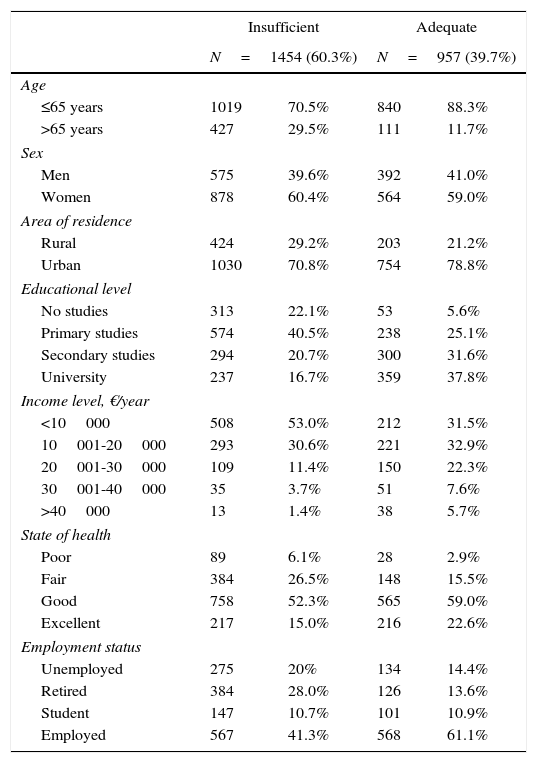
ResultsWe invited 3342 potential subjects, of whom 931 declined to participate (28.8%). We conducted 2658 interviews; 247 (9.3%) were considered not valid because of incorrect data or missing values for the main variables. Therefore, 2411 interviews were included. All of the interviewees lived in Extremadura; 99.5% were Spanish citizens and 0.5% had other nationalities. Women represented 59.8% (1442) of the sample and men, 40.2% (960). Mean age±standard deviation of participants was 49.0±18.7 years (range, 18.1-93.8 years). 26% (627) of the interviewed individuals lived in a rural area; 24.7% of the population had completed university studies and 15.2% presented a low level of schooling (less than 6 years). Only 2.1% of the population reported having an income over 40000euros per year, and income was less than 10000euros in 29.9%. The unemployment rate was 17%. Almost 74% of the population classified their state of health as excellent or good, while the remaining (26%) classified it as fair or poor. According to the research group's consensus definition of ‘adequate knowledge’, only 39.7% (95% CI, 37.7-41.6) of the participants were said to have an adequate knowledge of stroke. Table 1 displays population characteristics broken down by degree of knowledge on stroke.
Demographic characteristics of the population and distribution according to knowledge of stroke.
| Insufficient | Adequate | |||
|---|---|---|---|---|
| N=1454 (60.3%) | N=957 (39.7%) | |||
| Age | ||||
| ≤65 years | 1019 | 70.5% | 840 | 88.3% |
| >65 years | 427 | 29.5% | 111 | 11.7% |
| Sex | ||||
| Men | 575 | 39.6% | 392 | 41.0% |
| Women | 878 | 60.4% | 564 | 59.0% |
| Area of residence | ||||
| Rural | 424 | 29.2% | 203 | 21.2% |
| Urban | 1030 | 70.8% | 754 | 78.8% |
| Educational level | ||||
| No studies | 313 | 22.1% | 53 | 5.6% |
| Primary studies | 574 | 40.5% | 238 | 25.1% |
| Secondary studies | 294 | 20.7% | 300 | 31.6% |
| University | 237 | 16.7% | 359 | 37.8% |
| Income level, €/year | ||||
| <10000 | 508 | 53.0% | 212 | 31.5% |
| 10001-20000 | 293 | 30.6% | 221 | 32.9% |
| 20001-30000 | 109 | 11.4% | 150 | 22.3% |
| 30001-40000 | 35 | 3.7% | 51 | 7.6% |
| >40000 | 13 | 1.4% | 38 | 5.7% |
| State of health | ||||
| Poor | 89 | 6.1% | 28 | 2.9% |
| Fair | 384 | 26.5% | 148 | 15.5% |
| Good | 758 | 52.3% | 565 | 59.0% |
| Excellent | 217 | 15.0% | 216 | 22.6% |
| Employment status | ||||
| Unemployed | 275 | 20% | 134 | 14.4% |
| Retired | 384 | 28.0% | 126 | 13.6% |
| Student | 147 | 10.7% | 101 | 10.9% |
| Employed | 567 | 41.3% | 568 | 61.1% |
In this study, we will describe the prevalence of ‘adequate knowledge’ in the general population according to social, demographic, and economic factors, as well as state of health.
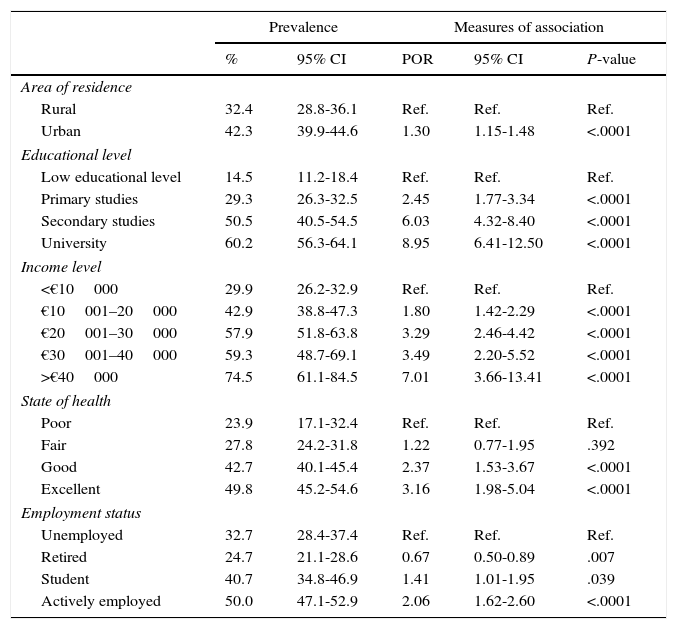
Area of residenceUrban residents have a better knowledge of stroke: 42.3% (95% CI, 39.9-44.6) displayed adequate knowledge vs 32.4% (95% CI, 28.8-36.1) of rural residents. These differences are statistically significant; POR is 1.30 (95% CI, 1.15-1.48; chi-square test of association: 18.9503, P=.0001).
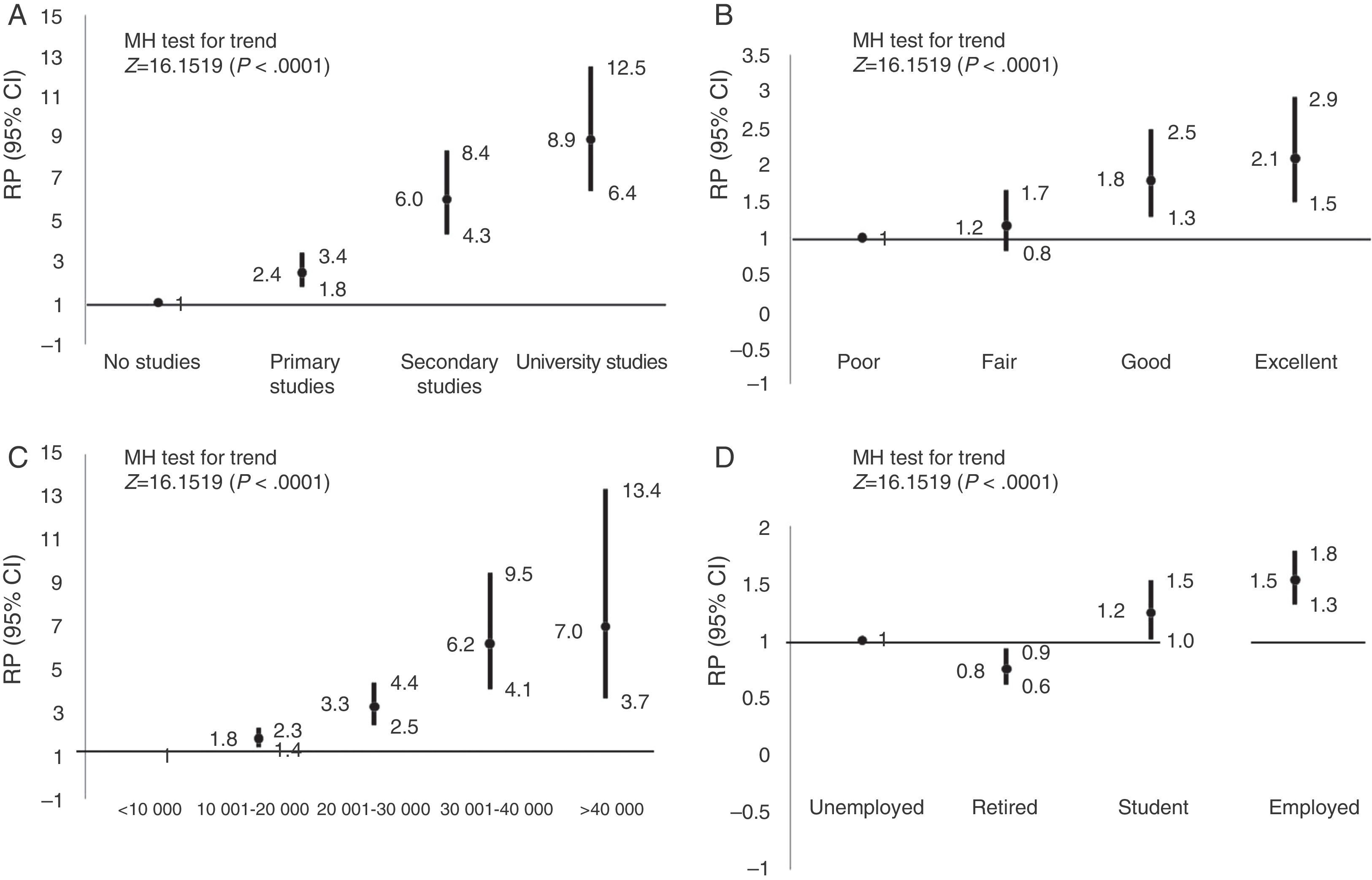
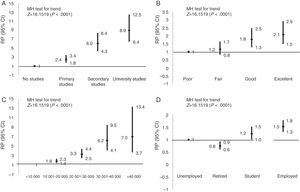
Educational levelPrevalence of adequate knowledge in individuals with a low educational level (less than 6 years) is only 14.5% (95% CI, 11.2-18.4). In individuals with a primary education, prevalence is 29.3% (95% CI, 26.3-32.5), compared to 50.5% (95% CI, 40.5-54.5) in those with secondary studies. Prevalence is notably higher in individuals with university studies: 60.2% (95% CI, 56.3-64.1). The trend analysis (MH test) showed a significant association; the highest educational levels vs the lowest show a clear dose-response gradient for adequate knowledge (Z=15.95; P<.0001) (Fig. 2A).
Self-reported level of incomeAs in the previous section, we compared the study variable ‘adequate knowledge’ with the four income categories provided for self-reported income level. We should highlight that 32.4% of the individuals interviewed chose not to answer this question, and that prevalence of adequate knowledge in this subgroup was 36.5%. Individuals with lower incomes (less than 10000euros/year) showed a low prevalence of knowledge at 29.9% (95% CI, 26.2-32.9). This prevalence increased with higher levels of income: 42.9% (95% CI, 38.8-47.3) in those reporting 10001-20000euros/year, 57.9% (95% CI, 51.8-63.8) in those reporting 20001 to 30000euros/year, and 59.3% (95% CI, 48.7-69.1) in those reporting 30001 to 40000euros/year. Prevalence reached 74.5% (95% CI, 61.1-84.5) in those at the highest income level. The trend analysis (MH test) also showed a significant association which indicates a clear gradient between higher levels of income vs. lower ones in the area of adequate stroke knowledge (Z=10.14, P<.0001) (Fig. 2C).
State of healthIndividuals with poorer health present a lesser degree of knowledge. Prevalence of adequate knowledge is 23.9% (95% CI, 17.1-32.4) and 27.8% (95% CI, 24.2-31.8) in those reporting poor or fair states of health, respectively. This contrasts with the prevalence found in those reporting good or excellent states of health, at 42.7% (95% CI, 40.1-45.4) and 49.8% (95% CI, 45.2-54.6), respectively. Trend analysis (MH test) also shows that having a good state of health is significantly and gradually associated with a higher level of stroke knowledge (Z=7.92; P<.0001) (Fig. 2B).
Professional situationIn our sample, 4.4% of the individuals preferred not to answer this question. A poorer knowledge of stroke was identified among retired and unemployed individuals, with prevalence values of 24.7% and 32.7%, respectively. On the contrary, better knowledge was found among actively employed individuals, with a prevalence of adequate knowledge of 50% (95% CI, 47.1-52.9). Among students, only 40.7% (95% CI, 34.8-46.9) have an adequate knowledge of stroke according to the consensus definition. The trend analysis (MH test) showed that actively employed individuals have a better knowledge of stroke than unemployed individuals, and that the difference is significant (Z=8.98; P<.0001) (Fig. 2D).
Table 2 displays a detailed overview of the prevalence and POR of the variable ‘adequate knowledge’ and the study variables.
Prevalence of ‘adequate knowledge’ and POR according to study variables.
| Prevalence | Measures of association | ||||
|---|---|---|---|---|---|
| % | 95% CI | POR | 95% CI | P-value | |
| Area of residence | |||||
| Rural | 32.4 | 28.8-36.1 | Ref. | Ref. | Ref. |
| Urban | 42.3 | 39.9-44.6 | 1.30 | 1.15-1.48 | <.0001 |
| Educational level | |||||
| Low educational level | 14.5 | 11.2-18.4 | Ref. | Ref. | Ref. |
| Primary studies | 29.3 | 26.3-32.5 | 2.45 | 1.77-3.34 | <.0001 |
| Secondary studies | 50.5 | 40.5-54.5 | 6.03 | 4.32-8.40 | <.0001 |
| University | 60.2 | 56.3-64.1 | 8.95 | 6.41-12.50 | <.0001 |
| Income level | |||||
| <€10000 | 29.9 | 26.2-32.9 | Ref. | Ref. | Ref. |
| €10001–20000 | 42.9 | 38.8-47.3 | 1.80 | 1.42-2.29 | <.0001 |
| €20001–30000 | 57.9 | 51.8-63.8 | 3.29 | 2.46-4.42 | <.0001 |
| €30001–40000 | 59.3 | 48.7-69.1 | 3.49 | 2.20-5.52 | <.0001 |
| >€40000 | 74.5 | 61.1-84.5 | 7.01 | 3.66-13.41 | <.0001 |
| State of health | |||||
| Poor | 23.9 | 17.1-32.4 | Ref. | Ref. | Ref. |
| Fair | 27.8 | 24.2-31.8 | 1.22 | 0.77-1.95 | .392 |
| Good | 42.7 | 40.1-45.4 | 2.37 | 1.53-3.67 | <.0001 |
| Excellent | 49.8 | 45.2-54.6 | 3.16 | 1.98-5.04 | <.0001 |
| Employment status | |||||
| Unemployed | 32.7 | 28.4-37.4 | Ref. | Ref. | Ref. |
| Retired | 24.7 | 21.1-28.6 | 0.67 | 0.50-0.89 | .007 |
| Student | 40.7 | 34.8-46.9 | 1.41 | 1.01-1.95 | .039 |
| Actively employed | 50.0 | 47.1-52.9 | 2.06 | 1.62-2.60 | <.0001 |
95% CI, 95% confidence interval; OR, odds ratio; Ref., reference category.
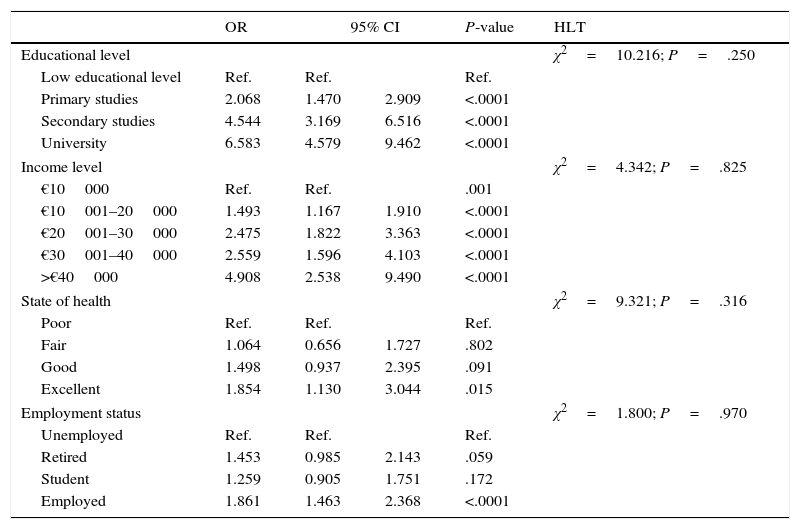
Table 3 includes the logistic regression models adjusted for age, sex, and area of residence. It seems clear that a good level of education and income, having a job, and enjoying an excellent state of health are independent predictors for having an adequate knowledge of stroke. We obtained a non-significant value with the Hosmer and Lemeshow test for the four models.
Logistic regression models adjusted for age, sex, and area of residence.
| OR | 95% CI | P-value | HLT | ||
|---|---|---|---|---|---|
| Educational level | χ2=10.216; P=.250 | ||||
| Low educational level | Ref. | Ref. | Ref. | ||
| Primary studies | 2.068 | 1.470 | 2.909 | <.0001 | |
| Secondary studies | 4.544 | 3.169 | 6.516 | <.0001 | |
| University | 6.583 | 4.579 | 9.462 | <.0001 | |
| Income level | χ2=4.342; P=.825 | ||||
| €10000 | Ref. | Ref. | .001 | ||
| €10001–20000 | 1.493 | 1.167 | 1.910 | <.0001 | |
| €20001–30000 | 2.475 | 1.822 | 3.363 | <.0001 | |
| €30001–40000 | 2.559 | 1.596 | 4.103 | <.0001 | |
| >€40000 | 4.908 | 2.538 | 9.490 | <.0001 | |
| State of health | χ2=9.321; P=.316 | ||||
| Poor | Ref. | Ref. | Ref. | ||
| Fair | 1.064 | 0.656 | 1.727 | .802 | |
| Good | 1.498 | 0.937 | 2.395 | .091 | |
| Excellent | 1.854 | 1.130 | 3.044 | .015 | |
| Employment status | χ2=1.800; P=.970 | ||||
| Unemployed | Ref. | Ref. | Ref. | ||
| Retired | 1.453 | 0.985 | 2.143 | .059 | |
| Student | 1.259 | 0.905 | 1.751 | .172 | |
| Employed | 1.861 | 1.463 | 2.368 | <.0001 | |
OR, odds ratio; 95% CI, confidence interval; Ref., reference category; €, euros; HLT, Hosmer and Lemeshow test.
The GDP of the region of Extremadura is much lower than the European mean (EU-27). The region occupies a large area of more than 42000km2 and its population density is low as the population barely exceeds 1000000 inhabitants. There is considerable population ageing, with almost 20% of its population aged 66 or older. According to official sources, stroke discharge rate per 1000 inhabitants in Extremadura in 2009 was 2.28 cases, which was above the Spanish mean of 1.8. Standardised stroke mortality rate is also 6 points above the Spanish mean, at 42.2 cases per 100000 inhabitants.17
Our study clearly shows that general knowledge of stroke is poorer among more socially disadvantaged groups, in which stroke incidence is usually higher.
There is no consensus regarding the definition of a basic knowledge of stroke for the general population. Most of the studies have defined it as the ability to list more than one or 2 stroke warning signs when asked an open-ended question.18–20 Our view is that this somewhat arbitrary cut-off point may reflect an unrealistic image of what citizens know about stroke and overestimate actual knowledge. As other authors have suggested, knowledge of stroke must be associated not only with the ability to identify symptoms but also with knowing how to react to a stroke, its main risk factors, and what to do if experiencing one.16,21,22 Furthermore, the ability to name at least one stroke symptom has not been shown to prevent delays in getting to the hospital in case of stroke, which may indicate a discrepancy between level of theoretical knowledge and response to symptoms.23 Our research group decided to define general knowledge of stroke as a construct including different essential factors; according to our measurement, an adequate level of knowledge is present in less than 40% of the population surveyed.
Our study focuses on the influence of sociodemographic factors on the knowledge about cerebrovascular disease. It shows a positive gradient between better knowledge and higher level of education, higher self-reported income, better state of health, and being actively employed, even after adjusting for potential confounders such as age, sex, and area of residence. We also detected a better level of knowledge among urban residents and in individuals aged 65 and younger.
Most previous studies have also found a positive association between education and knowledge, and some of them do mention an association with socioeconomic status.24,25 The effect of age on stroke knowledge is more difficult to analyse. Data from several studies suggest that knowledge of stroke describes an inverted U-shaped function with age, meaning that levels are lower among younger individuals and elderly people.25 Our study has also identified this association with age (data not presented here). A previous study has shown an association between good or excellent self-reported state of health and better knowledge of warning signs and responding correctly to stroke26; our study shows similar results. We have also observed that employment status impacts knowledge such that unemployed or retired individuals present poorer knowledge of warning signs, as has also been suggested by other articles.16,26,27
Intravenous thrombolysis is considered the most effective reperfusion therapy for stroke. Since the technique was introduced, researchers have tried multiple strategies intended to reduce delays in hospital arrival times, since thrombolysis has a narrow therapeutic window. Most of these actions have been awareness campaigns aimed at different target groups, and their main focus has been on identifying warning symptoms and knowing how to react to them.28–30 These awareness campaigns seem to be successful, as we observe in a 2009 meta-analysis based on 65 population studies that showed a progressive decrease in prehospital delays in stroke patients since 1980.31 Data from the Spanish registry EPICES have also revealed an important reduction in onset-to-door and door-to-neurologist times.32
Research has demonstrated that individuals with higher levels of education and income are more likely to seek prompt medical care when they experience stroke symptoms.33 Other studies suggest that social inequality, mainly in economic and educational terms, has associated psychosocial factors that promote or exacerbate vascular risk factors, and in turn, risk of vascular events.1,4 Therefore, socioeconomic status is a factor that affects both an individual's health-related behaviour and the state of health of the population as a whole.
As other authors have stated, the most common reason for delays in pre-hospital care is failure to identify stroke symptoms on the part of the general population, who remain unaware that the situation is in fact an emergency and often wait to see if it will resolve spontaneously. They refrain from seeking medical assistance or else call after a significant delay.25,34 Delays may be even longer among socially disadvantaged groups, rural residents, and elderly patients, considering their low level of stroke knowledge.
Awareness campaigns may improve knowledge of stroke and of proper responses to the disease. The effectiveness of these campaigns may be increased by making good use of mass media to transmit simple messages adapted to the public's social reality. It is crucial for campaigns to stress that prompt response to warning symptoms is the key to reducing mortality and disability risks in case of stroke.
FundingThis study was financed by a grant for neuroscience research from FUNDESALUD and the Society of Neurology of Extremadura (FUNNE0901).
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank the Office of the Dean of the Faculty of Medicine of the University of Extremadura for their involvement with the project, and FUNDESALUD for their logistical help. We would also like to thank Dr. González Dorrego for his constant encouragement, as well as the participating medical students for their hard work and commitment.
Please cite this article as: Ramírez-Moreno JM, Alonso-González R, Peral Pacheco D, Millán-Nuñez MV, Roa-Montero A, Constantino-Silva AB, et al. Impacto del nivel socioeconómico en el conocimiento del ictus de la población general: un gradiente de desigualdad social. Neurología. 2016;31:24–32.