Epilepsy is a very common disease in Spain. There is a great lack of information on real epidemiological data and the patient impact of this disease. The objective of the Spanish Foundation for Neurological Diseases (FEEN) report is to collect epidemiological data, morbidity, mortality and costs of this disease in Spain.
DevelopmentA search was carried out in Medline on publications up to 2010, as well as a review of data published by the Spanish National Statistics Institute (INE). There are about 400,000 patients with epilepsy in Spain. Approximately 5–10% of the population will experience a seizure in their lifetime, and up to 20% of these will have recurrent seizures. Using hospital discharge report data, hospital admissions for epilepsy are around 35 patients per 100,000 patients. Mortality risk in epileptic patients is two or three times higher than in non-epileptics. The mean total annual cost of drug-resistant epilepsy patient in Spain is 6935 euros. The total cost of epilepsy according to data from the year 2000 could be around 5% of the total health budget.
ConclusionsIt is very important to maintain disease registers. This initiative should be encouraged by the patient associations and scientific societies. This report confirms that epilepsy has a great social and health impact on the population.
La epilepsia es una enfermedad muy prevalente en España. Existe un gran vacío de información sobre los datos epidemiológicos reales de esta enfermedad así como la repercusión que esta enfermedad produce sobre el paciente. El objetivo de la Fundación Española de Enfermedades Neurológicas con este informe es recoger los datos epidemiológicos, de morbi-mortalidad y coste que de esta enfermedad existen en nuestro país.
DesarrolloSe ha realizado una búsqueda en Medline sobre lo publicado hasta 2010 y una revisión de los datos publicados por el Instituto Nacional de Estadística. En España hay alrededor de 400.000 pacientes con epilepsia. Aproximadamente el 5–10% de la población experimentará una crisis a lo largo de su vida y hasta un 20% de éstos tendrán crisis recurrentes. Los ingresos hospitalarios por epilepsia suponen 35 pacientes por cada 100.000 enfermos dados de alta en un hospital. Un paciente epiléptico tiene dos o tres veces más riesgo de morir que un no epiléptico. El total del coste medio de recursos anual de un paciente farmacorresistente en España es de 6.935 euros. El coste total de la epilepsia prevalente según datos del 2000 puede suponer alrededor del 5% del presupuesto total de Sanidad.
ConclusionesLa epilepsia supone un gran impacto socio-sanitario en la población española. La promoción de registros sobre enfermedades y su repercusión sobre los pacientes debe ser una iniciativa que debe propulsarse desde las sociedades científicas y de pacientes.
Epilepsy was one of the first conditions described in the history of neurology. It was first reported in ancient Babylon over 3000 years ago. It was not until 400 BC that Hippocrates postulated that epilepsy was a brain disorder. Of Greek origin, the word epilepsy means “attack”. The strange behaviour caused by certain types of crises has generated many superstitions and prejudices throughout history. Many important people in history have suffered epilepsy; the best known are the Russian writer Dostoyevsky, the philosopher Socrates, general Napoleon and the inventor of dynamite, Alfred Nobel. Even some Olympic medallists and other athletes have also suffered epilepsy.1
An epileptic crisis is a sudden and temporary disruption caused by abnormal neuronal activity that can cause strange sensations, emotions and behaviour, as well as muscle spasms and loss of consciousness. Epilepsy is a predisposition towards repeated epileptic crises. A person is considered to have epilepsy when he/she has suffered two or more epileptic crises. There are two basic types of crises: generalised crises and partial or focal crises. In generalised crises, the epileptic discharge affects the whole surface of the brain at the same time, whereas the epileptic discharge starts in one part of the brain in partial or focal crises.2
The stigma that exists about epilepsy is often mentioned, but thanks to a better-informed society, the attitude about this disease is changing.
This report has been prepared by the Spanish Foundation of Neurological Diseases in order to provide more data on the epidemiology and disability produced by this disease. Its aim is not only to publicise the existing published data, but also the lack of information available, particularly regarding the disability created by the disease.
DevelopmentEpidemiology of epilepsyThe prevalence of active epilepsy varies widely (between 2.7 and 40 cases per 1000 inhabitants), although most studies put it at around 8/1000 population (this represents approximately 360,000 cases in Spain).
The annual incidence of epilepsy is 31–57/100,000 (between 12,400 and 22,000 new cases each year in Spain), with this incidence being higher in children aged between 6 and 14 years (incidence of 3.7/1000), adolescents and the elderly (the incidence at ages above 60 years is of 134/100,000 inhabitants). The cumulative incidence of epilepsy until age 80 is 3%. Approximately 5–10% of the population will experience a crisis during their lives and up to 20% of these will suffer recurrent crises.3
It is estimated that there are about 400,000 patients with epilepsy in Spain. Slightly over 50% of cases are partial (57%) and over 60% of epileptic syndromes (according to ILAE) are focal syndromes. Around 75–80% of patients with epilepsy are well controlled with medication during the first 2 years after diagnosis. Around 10–15% of these cases are controlled by the association of several antiepileptic drugs and recently introduced drugs achieve control in less than an additional 10% of patients. Overall, it is estimated that between 8% and 33% of epilepsies are uncontrollable through medical treatment. This means that roughly one-third of the approximately 400,000 epileptics in Spain have seizures that cannot be controlled with medication. This represents over 100,000 patients in whom alternative therapies should be considered, included among which is surgery for epilepsy.4
Many studies have found a relatively higher incidence and prevalence in males. Some studies justify this finding by the higher incidence in males of the risk factors for epilepsy (traumatism, cerebrovascular disease, central nervous system infections).
Studies on the aetiology of epilepsy have found that the proportion of epilepsy with known aetiology is consistent, ranging between 23% and 39%, with congenital aetiology being the most frequent in children and cerebrovascular disease in adults.
We have collected the following published data from the numerous studies conducted in various areas of Spain (assuming methodological variability): in 1997, a prevalence of 4.7/1000 population was found in the north of Madrid for all types of epilepsy5; between the years 2002 and 2005, an incidence of 62.6 cases/100,000 inhabitants was found in the child population of Navarra, with a maximum value of 95.3 cases/100,000 inhabitants in the first year of life, which progressively decreased to 48.7 cases/100,000 inhabitants throughout adolescence6; a prevalence of epilepsy in the adolescent population of 6.3/1000 inhabitants was found in Huesca,7 among which generalised seizures of idiopathic aetiology were predominant.
The National Health Survey (data from 2006) shows the data on epilepsy only for the group younger than 16 years. Of these, 2.1% presented epilepsy as a chronic disease of long evolution over the past 12 months. Of these 62.8% were foreign patients. The age group with the highest percentage of epilepsy was between 10 and 15 years in males and between 5 and 9 years in females.
Morbidity of epileptic patientsEpilepsy, especially the drug-resistant variety, represents a great burden for both patients and their families. Patients present significant medical and social problems in relation to recurrent crises, the underlying neurological disease, the side effects of medication and social stigmatisation. They also frequently suffer from cognitive difficulties and social exclusion problems, such as school failure not related to cognitive capacity, unemployment, low marriage rates and fewer children.7
Studies on the frequency of admitted patients with neurological pathologies estimate that epilepsy is one of the most common causes of hospital admission. In a study carried out in Elche, “epilepsy” was the third most common cause of neurological admission (7.6% of the total).8,9 In addition, epilepsy is often the second leading cause for neurological care in Emergency Services, specifically representing 13.06% of patients treated at the Emergency Service, according to a study conducted at the 12 de Octubre Hospital10 in Madrid.
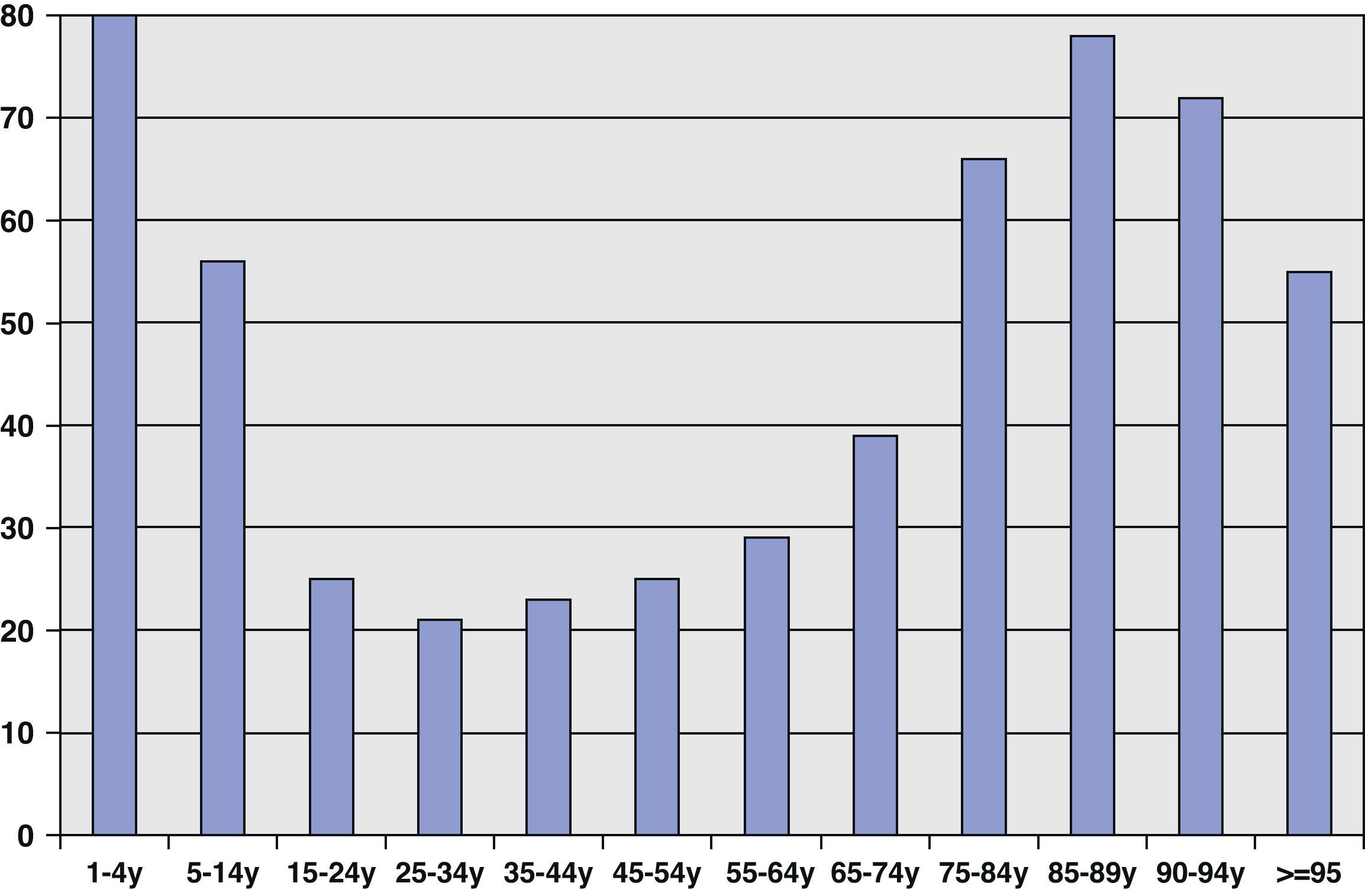
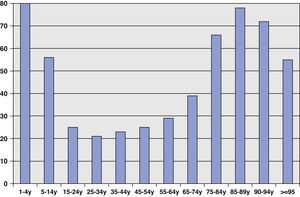
Fig. 1 shows the data for 2007 from the National Institute of Statistics in Spain (INE), which show the number of hospital admissions per 100,000 inhabitants grouped by patient age. The highest rate of hospital admissions for epilepsy corresponded to paediatric and elderly patients, which is consistent with the age groups in which epilepsy is most prevalent. The overall number of hospital admissions of epileptic patients per population of 100,000 is 35. The average stay of an epileptic patient admitted in an ordinary manner is 5.74 days, while the figure for emergency admissions is 6.44 days.
Admission or morbidity of epileptic patients does not only occur due to the presence of epileptic crises, but also through accidents resulting from them. In epileptic patients, the risk factors most commonly related to suffering an accident are gender, generalised tonic–clonic crisis and frequency of crises. The frequency of crises and the adverse effects of medication are the most important risk factors for accidents occurring during swimming and bathing.11
Mortality of epileptic patientsAn epileptic patient is between 2 and 3 times more likely to die than a non-epileptic patient. Mortality rates range from 1 to 2 per 100,000 epileptic patients in most countries. In a prospective community study carried out in Rochester, Hauser12 showed that the mortality rate was 2.3 times higher after 29 years follow-up than the general mortality rate, with the highest rates being shown in the early years of the disease, in males, in patients with neurological deficits and in symptomatic epilepsies.
The lowest mortality rate can be found in idiopathic epilepsies, but this is still higher than for the general population. The highest mortality rate is found in patients with symptomatic epilepsy, with a standardised mortality rate of up to 4.3%.
The aetiology of epilepsy is the most important cause of mortality in newly diagnosed patients. In contrast, crisis-associated mortality (status epilepticus and sudden unexpected death in epilepsy [SUDEP]) is the most common cause in chronic epileptic patients.13
Between 6% and 19% of deaths are directly related to the crises: 20–30% are caused by pneumonia and 10–20% by accidents, particularly drowning.
With regard to the specific causes of death, those caused by traumatisms and accidents are more frequent than in the general population. According to a cohort study including 9000 patients, compared with the general population epileptics died 1.8 times more often due to traffic accidents, 4.6 times due to falling, 10.3 times due to fatal burns and 8.2 times more often due to immersion or asphyxiation with a foreign body. Suicides were also common, being the cause of death 3.5 times more often than in the general population. This study found that death due to malignant tumours of the central nervous system presented a rate 30 times higher than expected for the general population, a fact that probably only expresses how common epilepsy is as presentation form or symptom in these diseases.14
The data from INE for 2007 show that the number of deaths due to epilepsy in that year was 676, of which 158 (23.3%) were caused by status epilepticus. Out of the patients who died due to status epilepticus, over 70% were aged over 65 years. Of those patients who died directly due to epilepsy (no status), 278 (54%) were aged over 65 years and only 7% were under 15 years. Assuming that the prevalence of epilepsy in Spain is approximately 360,000 cases, the annual mortality rate in 2007 was 1.9%, which is consistent with the published data.
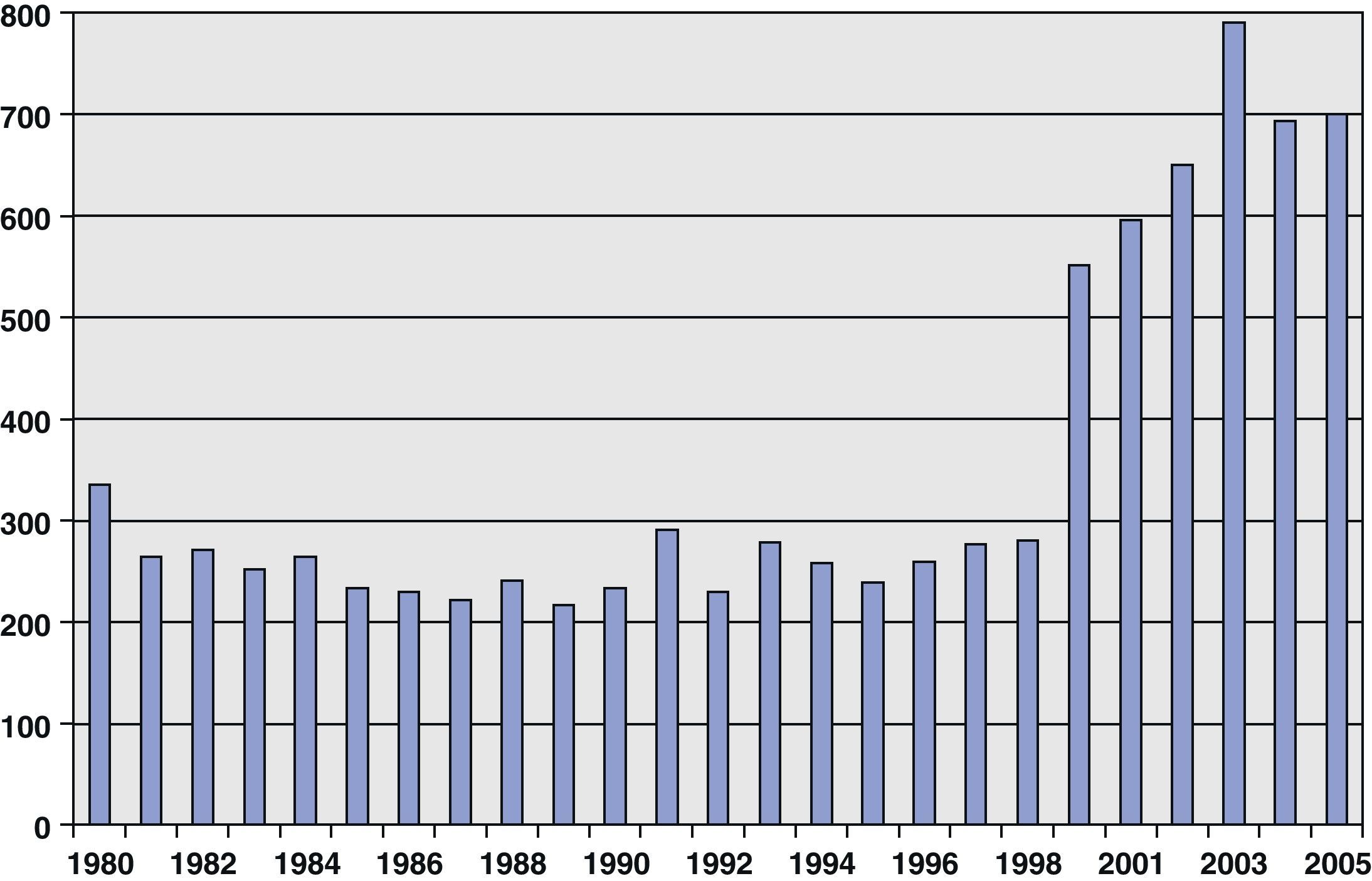
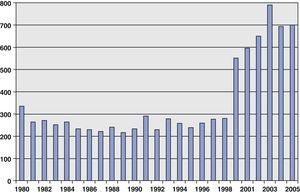
Fig. 2 shows the mortality due to epilepsy from 1980 until 2007 (except in the years 1999 and 2000, for which data were not available). There is a clear quantum leap in mortality from 2001, probably because data after this year also include death due to status epilepticus and we do not know if the previous data collected this point or not. In recent years, we have seen that mortality due to epilepsy has remained stable, with no significant differences in annual mortality.
Disability and dependenceAlthough the vast majority of epileptic crises do not cause accidents, the possibility of these occurring causes unrest and insecurity by itself among patients and their families. Following a series of relatively simple recommendations is enough to reduce the risk of injuries in relation to crises. The application of these recommendations is especially important in situations where crises are more frequent or severe, to prevent permanent disability and dependency due to accidents.
The Labour Force Survey for the second quarter of 2002 showed that the majority of the population with disability was not included within the labour market: 2 out of 3 disabled people of working age were unemployed; the unemployment rate among these people was 40% higher than among healthy people. According to the survey, the number of epilepsy patients of working age in Spain was about 26,200; in other words, 1.1% of patients of working age suffered disability due to epilepsy; of these, 18,300 had work limitations and 12,000 had difficulty to commute to their place of work.15 Within the epileptic patients with recognised disability, only 25% were in active employment status. There were no further data from the INE on disability and epilepsy in Spain.
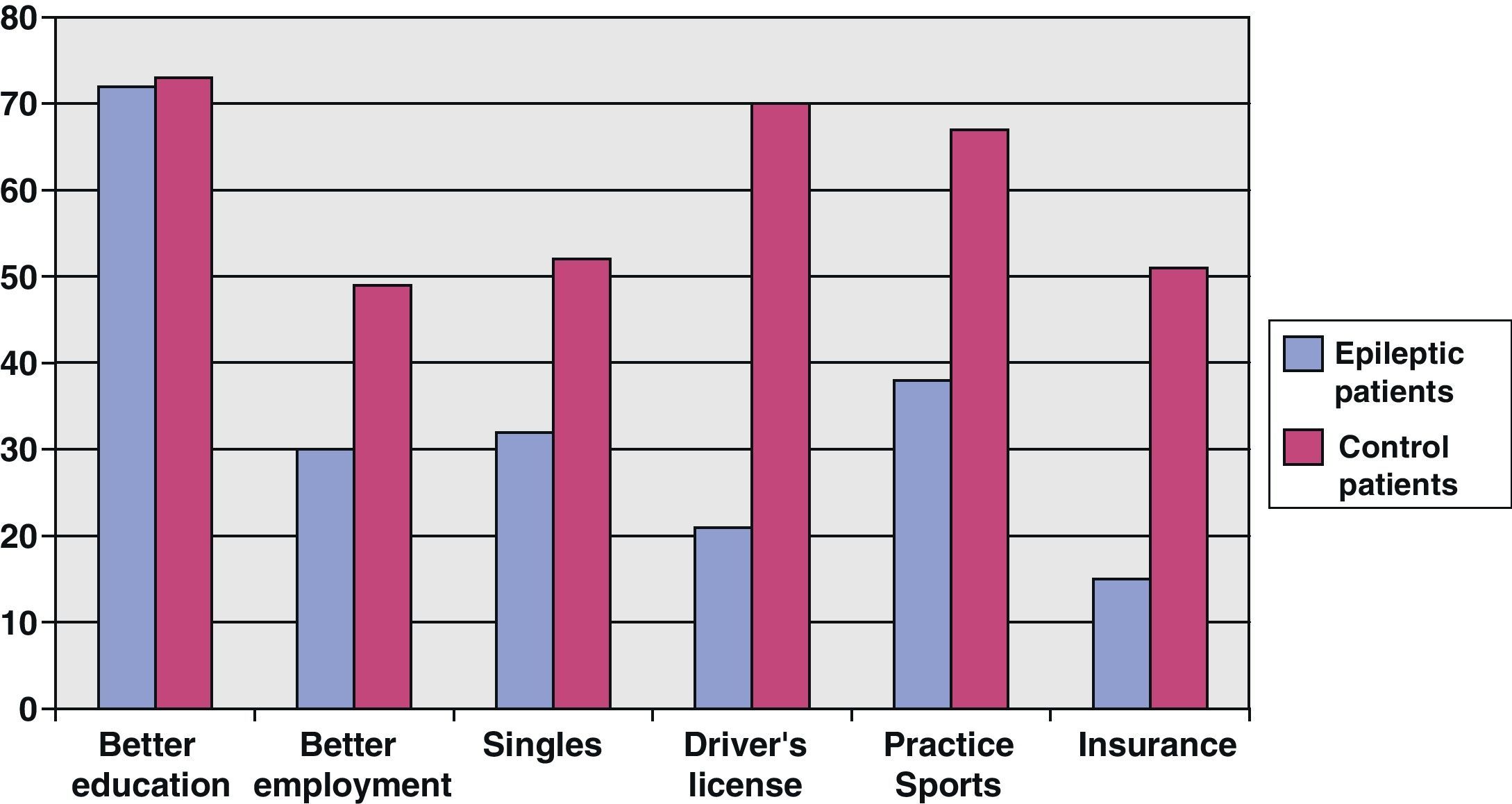
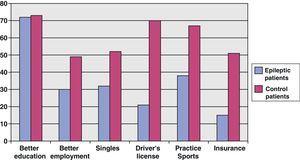
A multicentre European study that included Spain and examined the social aspects of epilepsy patients was published in January 2000. Its results included the following: slightly higher educational level in epileptic patients than in non-epileptic patients; when compared with controls, patients were more often single (56% vs 50%) and unemployed (18% vs 13%); in contrast, compared with controls, fewer patients had a driving license (44% vs 67%) and practiced sports (30% vs 41%)16 (Fig. 3).
Social-healthcare costThe World Health Organisation and the World Bank supervised a study that showed that 90% of the costs generated by epilepsy worldwide were produced in developing countries, while 80% of the total health outlay took place in developed countries. Therefore, the European White Paper on epilepsy set as a target for the 21st century the availability of effective epilepsy care for anyone who required it, regardless of national and economic borders.17
A socioeconomic impact study on the cost of childhood epilepsy conducted in Spain in the year 200018 concluded that the annual expenditure in the case of controlled epilepsy was 334,143 pesetas (2008.24 euros) and it was 848,105 pesetas (5097.21 euros) in the case of uncontrolled epilepsy; that is, 2.7 times higher than in controlled. Another study estimated that the total cost of prevalent epilepsy in 1998 represented 11,500 million pesetas (69.1 million euros), which represented 0.55% of the annual healthcare budget for that year.19 By extrapolating these figures to the prevalence of epilepsy in all age groups (1%), the health system spent about 184,000 million pesetas (1106 million euros) to cover epilepsy care. This represented 4.13% of the budget intended for health in the year 2000. The cost of epilepsy in Europe in the year 2004 was approximately 816 million euros.20
A study published in 200421 that analysed the cost of epilepsy in Spain noted that the total amount of pharmaceutical benefits by prescription in 2001 was 1,332,034 million pesetas (8005.69 million euros). The subgroup comprised by antiepileptic drugs represented a cost of 18,155 million pesetas (109.11 million euros) during that year, which corresponded to 1.36% of total costs, with a growth increase of 5.84% in relation to 2000. The total number of antiepileptic drug packages consumed was 5098 million, which represented an increase of 7.13% over the previous year. The average price of each package was 3561 pesetas (21.40 euros). The increase observed in total expenditure in pesetas with respect to the previous year was due to the increasing use of next-generation AEDs, which have a much higher price than classic AEDs.
Studies conducted in Spain22 on the cost-effectiveness of classic vs new drugs concluded that they were equally effective. In addition, the lower cost of classic AEDs made them more effective drugs for the treatment of recently diagnosed partial and generalised epilepsy in adults. These results, which have been corroborated by studies in other countries, have generated some concern among professionals and public bodies, considering that AED acquisition cost represents an important part of the total cost of treating epileptic patients.28
Drug-resistant epilepsy—social-economic impactMost epileptic patients (70–75%) are well controlled with medication, but there is a non-negligible percentage in whom the crises do not cease despite appropriate drug therapy. According to some studies, the percentage of patients with refractory epilepsy is higher than assumed and only half of these patients are evaluated at a specialised unit, with a significant delay that amounts to 10 years in most cases. Crises in these patients pose a significant limitation to most activities and often bring about a greatly reduced quality of life. In addition, the mortality rate due to causes other than the crises (sudden death, suicide) and the rate of psychiatric disorders requiring frequent medical attention and hospital admissions have been shown to be higher in this group of patients. These data show that it is essential to identify these patients and treat them early to decrease morbidity and mortality, as well as to greatly reduce the demand for both emergency and planned hospital admission that this disease currently requires.23
There is no agreed definition or universally accepted criteria for epilepsy refractory to medical therapy, since it is not possible to establish the point when epilepsy goes from being potentially treatable to being considered refractory to medical therapy. A theoretical definition would consider as drug-resistant those cases of epilepsy presenting an unsatisfactory control of crises after having used at least 2 different agents, at appropriate doses, over a period of at least 2 years. In general, this type of epilepsy has less than 5–10% chance of achieving total control with medication.24
In Spain, the average annual cost of healthcare resources for a person with these characteristics is around 6935 euros, according to the results obtained by the LINCE study, developed by the Epilepsy Group of the Spanish Neurology Society in 2005.25
The mean age of patients included in the LINCE study was 40 years, with disease duration of nearly 24 years. Most patients were treated with a different combination of 2 or 3 antiepileptic drugs without achieving control of crises. Up to 70.5% of drug-resistant epilepsy patients presented focal seizures of moderate to severe intensity. The aetiology or cause of the epilepsy was known in 41.5% of patients, with the most common causes being non-progressive encephalopathy in 22.7%, malformations due to cortical alterations during development in 21.3% and postnatal causes in 35%.
Quality of life as a result of the disease was substantially reduced in these patients. The worst valued aspect by patients with this type of epilepsy was the impact of medication on themselves, while monitoring of the disease by the physician was the aspect with the best evaluation. In addition, 54% presented some degree of anxiety associated with epilepsy, while 32% suffered depression.
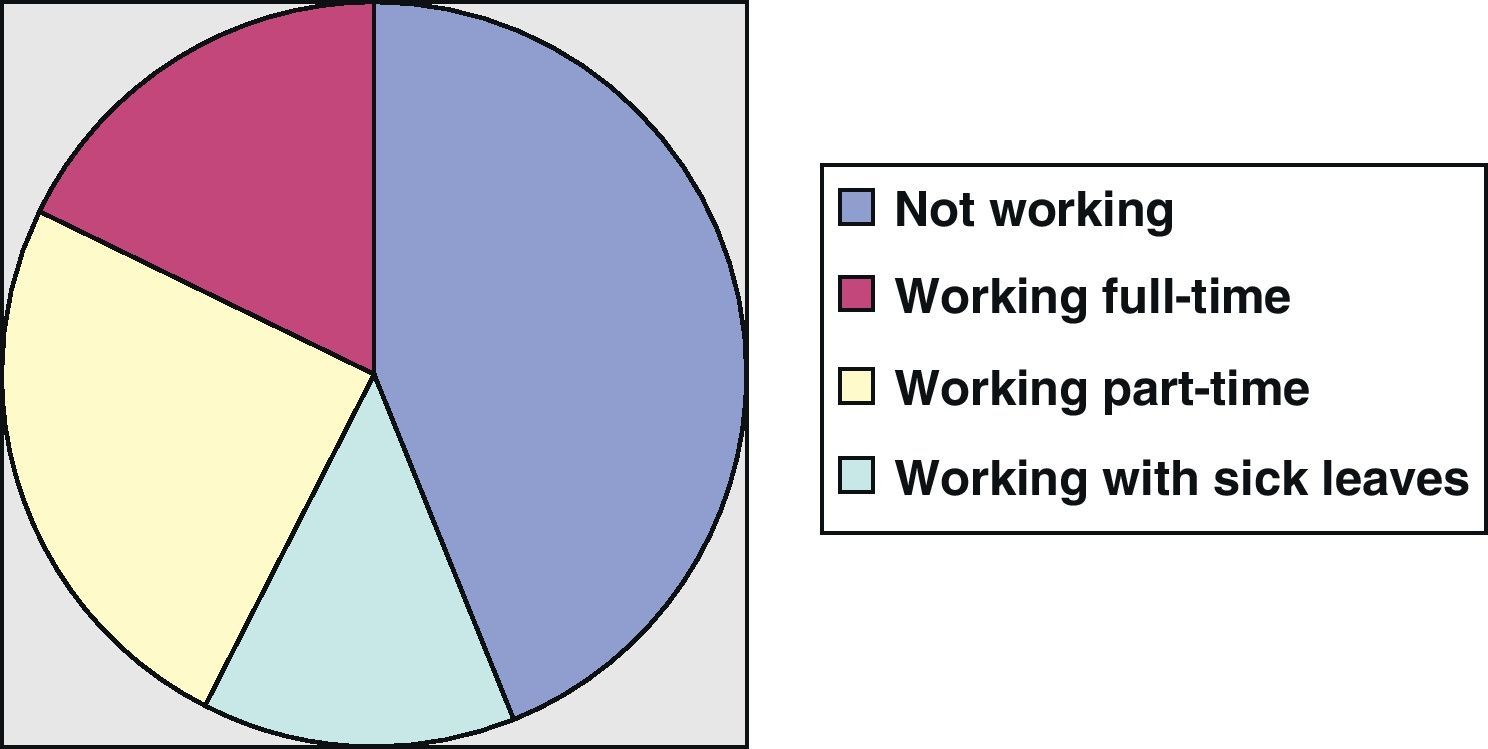
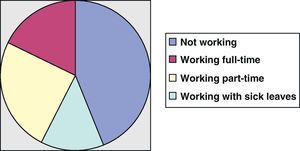
The study showed that drug-resistant epilepsy caused a considerable burden on patients and their families: 44% of patients did not work because of their disease and 37.5% of families reported that their economy was greatly affected, with 32.9% of them requiring the help of a caregiver. Of the patients who did work (56%), 44% had to reduce their working hours and 33% had accumulated at least one sick leave over the past 6 months (Fig. 4). The mean monthly non-reimbursed extra spending due to the disease was 257 euros for each patient.
The mean annual cost of healthcare resources employed by patients was 5254 euros, including visits to doctors, hospitalisation and medication, with a further 1681 euros for non-healthcare costs including those associated with labour productivity and with the economy of the patient. Therefore, the total mean annual cost of the resources for each drug-resistant patient in Spain was 6935 euros.
Epilepsy and drivingEpilepsy represents a safety risk during driving. The risk of an active epileptic person is determined by not only a possible crisis with loss of consciousness while driving, other associated problems such as mental retardation, behavioural disorders and side effects of antiepileptic treatment (mainly sedation) also contribute. Patients should be aware of these complications, because between 50% and 60% of seizures can cause traffic accidents.13
However, 2 major studies concluded that epileptic drivers do not suffer accidents more frequently than non-epileptics. The severity of accidents involving epileptic patients is 40% higher than that of controls and the possibility of death of passengers is doubled.26
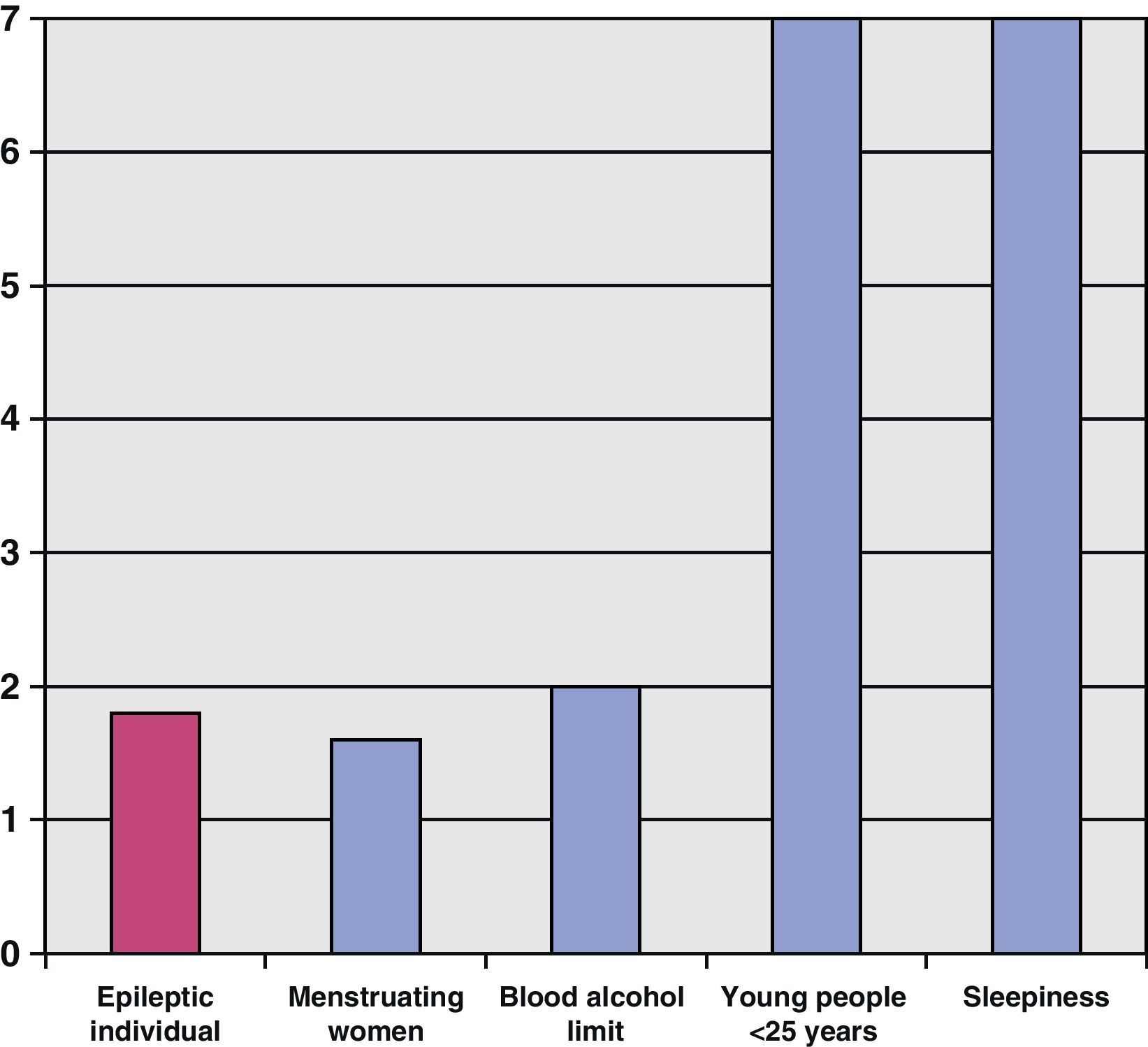
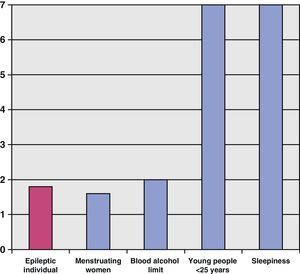
The European Union report “Epilepsy and driving in Europe” showed that epileptic patients had a 1.8 risk (odds ratio) of suffering accidents. This figure was slightly higher than the risk for women driving at some stage of their menstruation cycle and slightly less than for those driving with blood alcohol levels over the limit. Young males under 25 or people driving with sleepiness reached the highest relative risk levels (Fig. 5). Since the odds ratio for epileptics was less than 2, the risk of suffering an accident within the next year was less than 20%. These figures can be a useful tool for physicians, who can analyse the individual risk for each patient from these data.
In Spain, a person with this disease must prove not to have suffered convulsive crises for 12 months to obtain a driving license (licenses A, A1, B, B+E and moped driving license), in addition to providing a favourable report from a neurologist. In this case, they will be granted a license valid for 2 years. In the case of professional drivers, they should have a 5-year crisis-free period. Patients with crises during sleep should report that they have passed at least 1 year with these symptoms alone. In the case of myoclonus that may affect driving safety, there must be a crisis-free period of at least 3 months. Finally, in the case of a single episode of crisis or one secondary to toxic substances or drugs, a crisis-free period of at least 6 months must be proven.27
ConclusionsEpilepsy is a neurological disease with a major public health impact on the Spanish population. This conclusion is drawn from the following facts: 5–10% of the population will experience a crisis at some time during their lives; out of all hospital admissions, those due to epilepsy represent 35 patients per 100,000 discharged from a hospital; and the total cost of prevalent epilepsy might represent up to 5% of the total health budget according to data from 2000. The limited sources of information, records and epidemiological studies must raise our awareness about their necessity, since they make it possible for us to know the real impact of this disease on our society and to obtain information about the main needs of our patients. This initiative should be supported by scientific societies and patient associations.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: García-Ramos R, et al. FEEN: Informe sociosanitario FEEN sobre la epilepsia en España. Neurología. 2011;26:548–55.